The nurse is analyzing a rhythm strip. What component of the ECG corresponds to the resting state of the patients heart?
A) P wave
B) T wave
C) U wave
D) QRS complex
B) T wave
The T wave specifically represents ventricular muscle depolarization, also referred to as the resting state. Ventricular muscle depolarization does not result in the P wave, U wave, or QRS complex.
An adult patient with third-degree AV block is admitted to the cardiac care unit and placed on continuous cardiac monitoring. What rhythm characteristic will the ECG most likely show?
A) PP interval and RR interval are irregular.
B) PP interval is equal to RR interval.
C) Fewer QRS complexes than P waves
D) PR interval is constant.
C) Fewer QRS complexes than P waves
In third-degree AV block, no atrial impulse is conducted through the AV node into the ventricles. As a result, there are impulses stimulating the atria and impulses stimulating the ventricles. Therefore, there are more P waves than QRS complexes due to the difference in the natural pacemaker (nodes) rates of the heart. The other listed ECG changes are not consistent with this diagnosis.
A patient has returned to the cardiac care unit after having a permanent pacemaker implantation. For which potential complication should the nurse most closely assess this patient?
A) Chest pain
B) Bleeding at the implantation site
C) Malignant hyperthermia
D) Bradycardia
B.) Bleeding at implantation site
Bleeding, hematomas, local infections, perforation of the myocardium, and tachycardia are complications of pacemaker implantations. The nurse should monitor for chest pain and bradycardia, but bleeding is a more common immediate complication. Malignant hyperthermia is unlikely because it is a response to anesthesia administration.
A nurse is caring for a patient who is exhibiting ventricular tachycardia (VT). Because the patient is pulseless, the nurse should prepare for what intervention?
A) Defibrillation
B) ECG monitoring
C) Implantation of a cardioverter defibrillator
D) Angioplasty
A.) Defibrillation
Any type of VT in a patient who is unconscious and without a pulse is treated in the same manner as ventricular fibrillation: Immediate defibrillation is the action of choice. ECG monitoring is appropriate, but this is an assessment, not an intervention, and will not resolve the problem. An ICD and angioplasty do not address the dysrhythmia.
The nurse is caring for a patient who has had a dysrhythmic event. The nurse is aware of the need to assess for signs of diminished cardiac output (CO). What change in status may signal to the nurse a decrease in cardiac output?
A) Increased blood pressure
B) Bounding peripheral pulses
C) Changes in level of consciousness
D) Skin flushing
C.) Changes in Levels of Consciousness
The nurse conducts a physical assessment to confirm the data obtained from the history and to observe for signs of diminished cardiac output (CO) during the dysrhythmic event, especially changes in level of consciousness. Blood pressure tends to decrease with lowered CO and bounding peripheral pulses are inconsistent with this problem. Pallor, not skin flushing, is expected.
The nursing educator is presenting a case study of an adult patient who has abnormal ventricular depolarization. This pathologic change would be most evident in what component of the ECG?
A) P wave
B) T wave
C) QRS complex
D) U wave
C) QRS Complex
The QRS complex represents the depolarization of the ventricles and, as such, the electrical activity of that ventricle.
The nurse caring for a patient whose sudden onset of sinus bradycardia is not responding adequately to atropine. What might be the treatment of choice for this patient?
A) Implanted pacemaker
B) Trancutaneous pacemaker
C) ICD
D) Asynchronous defibrillator
B.) Transcutaneous Pacemaker
If a patient suddenly develops a bradycardia, is symptomatic but has a pulse, and is unresponsive to atropine, emergency pacing may be started with transcutaneous pacing, which most defibrillators are now equipped to perform. An implanted pacemaker is not a time-appropriate option. An asynchronous defibrillator or ICD would not provide relief
The nurse is writing a plan of care for a patient with a cardiac dysrhythmia. What would be the most appropriate goal for the patient?
A) Maintain a resting heart rate below 70 bpm.
B) Maintain adequate control of chest pain
C) Maintain adequate cardiac output.
D) Maintain normal cardiac structure.
C) Maintain Adequate Cardiac Output
For patient safety, the most appropriate goal is to maintain cardiac output to prevent worsening complications as a result of decreased cardiac output. A resting rate of less than 70 bpm is not appropriate for every patient. Chest pain is more closely associated with acute coronary syndrome than with dysrhythmias. Nursing actions cannot normally influence the physical structure of the heart.
8. The nurse is caring for an adult patient who has gone into ventricular fibrillation. When assisting with defibrillating the patient, what must the nurse do?
A) Maintain firm contact between paddles and patient skin.
B) Apply a layer of water as a conducting agent.
C) Call all clear once before discharging the defibrillator.
D) Ensure the defibrillator is in the sync mode.
A. Maintain firm contact between paddles and pt skin.
When defibrillating an adult patient, the nurse should maintain good contact between the paddles and the patients skin to prevent arcing, apply an appropriate conducting agent (not water) between the skin and the paddles, and ensure the defibrillator is in the nonsync mode. Clear should be called three times before discharging the paddles.
During a CPR class, a participant asks about the difference between cardioversion and defibrillation. What would be the instructors best response?
A) Cardioversion is done on a beating heart; defibrillation is not.
B) The difference is the timing of the delivery of the electric current.
C) Defibrillation is synchronized with the electrical activity of the heart, but cardioversion is not.
D) Cardioversion is always attempted before defibrillation because it has fewer risks.
B.) The difference is the timing of the delivery of the electric current.
One major difference between cardioversion and defibrillation is the timing of the delivery of electrical current. In cardioversion, the delivery of the electrical current is synchronized with the patients electrical events; in defibrillation, the delivery of the current is immediate and unsynchronized. Both can be done on beating heart (i.e., in a dysrhythmia). Cardioversion is not necessarily attempted first.
An ECG has been ordered for a newly admitted patient. What should the nurse do prior to electrode placement?
A) Clean the skin with providone-iodine solution.
B) Ensure that the area for electrode placement is dry.
C) Apply tincture of benzoin to the electrode sites and wait for it to become tacky.
D) Gently abrade the skin by rubbing the electrode sites with dry gauze or cloth
D.) Gently abrade the skin by rubbing electrode sites with dry gauze or cloth
An ECG is obtained by slightly abrading the skin with a clean dry gauze pad and placing electrodes on the body at specific areas. The abrading of skin will enhance signal transmission. Disinfecting the skin is unnecessary and conduction gel is used.
A patient converts from normal sinus rhythm at 80 bpm to atrial fibrillation with a ventricular response at 166 bpm. Blood pressure is 162/74 mm Hg. Respiratory rate is 20 breaths per minute with normal chest expansion and clear lungs bilaterally. IV heparin and Cardizem are given. The nurse caring for the
patient understands that the main goal of treatment is what?
A) Decrease SA node conduction
B) Control ventricular heart rate
C) Improve oxygenation
D) Maintain anticoagulation
B.) Control Ventricular HR
Treatment for atrial fibrillation is to terminate the rhythm or to control ventricular rate. This is a priority because it directly affects cardiac output. A rapid ventricular response reduces the time for ventricular filling, resulting in a smaller stroke volume. Control of rhythm is the initial treatment of choice, followed by anticoagulation with heparin and then Coumadin.
11. The nurse is caring for a patient who has just had an implantable cardioverter defibrillator (ICD) placed. What is the priority area for the nurses assessment?
A) Assessing the patients activity level
B) Facilitating transthoracic echocardiography
C) Vigilant monitoring of the patients ECG
D) Close monitoring of the patients peripheral perfusion
C.) Vigilant Monitoring of a patients ECG
After a permanent electronic device (pacemaker or ICD) is inserted, the patients heart rate and rhythm are monitored by ECG. This is a priority over peripheral circulation and activity. Echocardiography is not indicated.
A patient has had an ICD inserted. What should the nurse be sure to include in the education of this pt prior to discharge? Select ALL THAT APPLY
A.) Avoid magnetic fields such as metal detector booths
B.) Call for emergency assistance if feeling dizzy
C.)Record events that trigger a shock sensation
D.) The pt may have a throbbing pain that is normal
E.) The pt will have to schedule monthly chest x-rays to make sure device is patent
A.) Avoid magnetic fields
B.) Call for emergency assistance if feeling Dizzy
C.) Record events that trigger a shocking sensation
. The nurse is caring for a patient who has had a biventricular pacemaker implanted. When planning the patients care, the nurse should recognize what goal of this intervention?
A) Resynchronization
B) Defibrillation
C) Angioplasty
D) Ablation
A.) Resynchronization
Biventricular (both ventricles) pacing, also called resynchronization therapy, may be used to treat advanced heart failure that does not respond to medication. This type of pacing therapy is not called defibrillation, angioplasty, or ablation therapy.
A group of nurses are participating in orientation to a telemetry unit. What should the staff educator tell this class about ST segments?
A) They are the part of an ECG that reflects systole.
B) They are the part of an ECG used to calculate ventricular rate and rhythm.
C) They are the part of an ECG that reflects the time from ventricular depolarization through repolarization.
D) They are the part of an ECG that represents early ventricular repolarization.
D) They are the part of an ECG that represents early ventricular repolarization.
ST segment is the part of an ECG that reflects the end of the QRS complex to the beginning of the T wave. The part of an ECG that reflects repolarization of the ventricles is the T wave. The part of an ECG used to calculate ventricular rate and rhythm is the RR interval. The part of an ECG that reflects the time from ventricular depolarization through repolarization is the QT interval.
A patient with Mitral Valve Stenosis and CAD is in the telemetry unit with pneumonia. The nurse assesses a 6 second strip and determines that the ventricular rhythm is highly irregular at 88, with no discernible P waves. What does the nurse determine this rhythm to be?
A.) Atrial Flutter
B.)Ventricular Flutter
C.) Ventricular Tachycardia
D.) Ventricular Fibrillation
A.) Atrial Flutter
7. A patient the nurse is caring for has a permanent pacemaker implanted with the identification code beginning with VVI. What does this indicate?
A) Ventricular paced, ventricular sensed, inhibited
B) Variable paced, ventricular sensed, inhibited
C) Ventricular sensed, ventricular situated, implanted
D) Variable sensed, variable paced, inhibited
A.) Ventricular Paced, Ventricular Sensed, Inhibited
10. A nurse is providing health education to a patient scheduled for cryoablation therapy. The nurse should describe what aspect of this treatment?
A) Peeling away the area of endocardium responsible for the dysrhythmia
B) Using electrical shocks directly to the endocarduim to eliminate the source of dysrhythmia
C) Using high-frequency sound waves to eliminate the source of dysrhythmia
D) Using a cooled probe to eliminate the source of dysrhythmia
D.) Using a cooled probe to eliminate the source of dysrhythmias
Cryoablation therapy involves using a cooled probe to create a small scar on the endocardium to eliminate the source of the dysrhythmias. Endocardium resection involves peeling away a specified area of the endocardium. Electrical ablation involves using shocks to eliminate the area causing the dysrhythmias. Radio frequency ablation uses high-frequency sound waves to destroy the area causing the dysrhythmias.
The nurse is caring for a patient who is in the recovery room following the implantation of an ICD. The patient has developed ventricular tachycardia (VT). What should the nurse assess and document?
A) ECG to compare time of onset of VT and onset of devices shock
B) ECG so physician can see what type of dysrhythmia the patient has
C) Patients level of consciousness (LOC) at the time of the dysrhythmia
D) Patients activity at time of dysrhythmia
A.) ECG to compare time of onset of VT and onset of devices shock.
If the patient has an ICD implanted and develops VT or ventricular fibrillation, the ECG should be recorded to note the time between the onset of the dysrhythmia and the onset of the devices shock or antitachycardia pacing. This is a priority over LOC or activity at the time of onset.
New nurses on the telemetry unit have been paired with preceptors. One new nurse asks her preceptor to explain depolarization. What would be the best answer by the preceptor?
A) Depolarization is the mechanical contraction of the heart muscles.
B) Depolarization is the electrical stimulation of the heart muscles.
C) Depolarization is the electrical relaxation of the heart muscles.
D) Depolarization is the mechanical relaxation of the heart muscles.
B.) Depolarization is the electrical stimulation of the heart muscle.
The electrical stimulation of the heart is called depolarization, and the mechanical contraction is called systole. Electrical relaxation is called repolarization, and mechanical relaxation is called diastole.
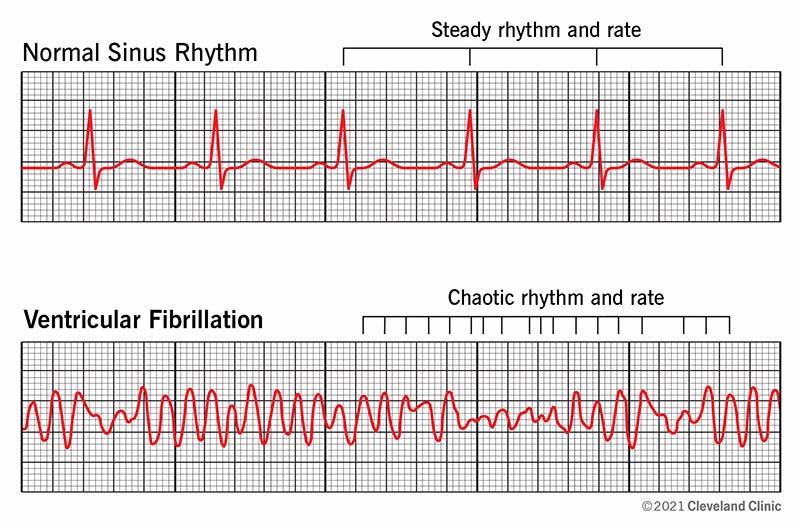
A pt who had a myocardial infarction is experiencing severe chest pain and alerts the nurse. The nurse begins the assessment but suddenly the pt becomes unresponsive, no pulse, with monitor showing a rapid, disorganized ventricular rhythm. What does the nurse interpret this rhythm to be?
A.) Ventricular Tachycardia
B.) Atrial Fibrilation
C.) Third- Degree heart block
D.) Ventricular Fibrillation
D.) Ventricular Fibrillation
Ventricular Fibrillation is completely chaotic, rapid rhythm with no cardiac output ( pulseless)
A patient is 2 days postoperative after having a permanent pacemaker inserted. The nurse observes that the pt is having continous hiccups as the pt states "I thought this was normal." What does the nurse understand is occurring with this patient?
A.) Fracture of lead wire
B.) Lead wire dislodgment
C.) Faulty generator
D.) Sensitivity is too Low
B.) Lead wire dislodgement
The nurse and the other members of the team are caring for a patient who converted to ventricular fibrillation (VF). The patient was defibrillated unsuccessfully and the patient remains in VF. According to national standards, the nurse should anticipate the administration of what medication?
A) Epinephrine 1 mg IV push
B) Lidocaine 100 mg IV push
C) Amiodarone 300 mg IV push
D) Sodium bicarbonate 1 amp IV
A.) Epinephrine 1 mg IV push
Epinephrine should be administered as soon as possible after the first unsuccessful defibrillation and then every 3 to 5 minutes. Antiarrhythmic medications such as amiodarone and licocaine are given if ventricular dysrhythmia persists.
The nurse in the ICU hears an alarm sound in th pts room. Arriving in the room, the pt is unresponsive, without a pulse, and a flatline on the monitor. What is the first action by the nurse?
A. Begin CPR
B.) Adminsiter Epinephrine
C.) Administer Atropine (0.5 mg)
D.) Defibrillate with 360 joules