HELP
What physiologic change occurs as a direct result of cardiogenic shock?
A.) increase in capacitance
B.) increase in afterload
C.) decrease in SVR
D.) decrease in preload
What is B.) increase in afterload?
Afterload increases in cardiogenic shock because the body constricts blood vessels to compensate for low blood pressure. This compensatory mechanism, called vasoconstriction, increases the amount of pressure the heart has to work against to pump blood.
A patient has heart failure secondary to ischemic cardiomyopathy and end-stage coronary artery disease. Which agents would be the MOST beneficial?
A. digoxin (Lanoxin) and diltiazem (Cardizem)
B. carvedilol (Coreg) and lisinopril (Zestril)
C. verapamil (Calan) and spironolactone (Aldactone)
D. flecainide (Tambocor) and hydralazine (Apresoline)
What is C. verapamil (Calan) and spironolactone (Aldactone)?
The patient has end-stage coronary artery disease causing systolic dysfunction. These drugs decrease afterload and minimize remodeling that is associated with heart failure. Calcium-channel blockers are contraindicated in heart failure. Digoxin may be used in heart failure. Spironolactone is given to block the aldosterone effect. Hydralazine is an alpha-blocker, which reduces afterload and is used in heart failure. Flecainide is contraindicated with structural heart disease.
This rhythm is exhibited by a patient with an acute inferior wall MI who has a BP of 74/38: 
The DEFINITIVE treatment for this patient is:
A.) synchronized cardioversion
B.) atropine sulfate
C.) epinephrine
D.) transvenous pacing
What is D.) transvenous pacing?
Synchronized cardioversion is usually used to treat Atrial fibrillation, Atrial flutter, Supraventricular tachycardia (SVT), and Ventricular tachycardia (with a pulse). All the other answer choices are TEMPORARY solutions but are not treating the cause.
Which 12-lead ECG changes should be expected in a patient with ACS involving the inferior wall?
A. ST segment elevation and deeply inverted T waves in leads V4 - V6, I and aVL
B. ST segment elevation in leads II, III and all the precordial leads
C. ST segment elevation and deeply inverted T waves in leads II, III and aVF
D. ST segment depression and T wave elevation in leads II, III and aVL
What is C. ST segment elevation and deeply invertedT waves in leads II, III and aVF?
An inferior wall MI is associated with changes in leads II, III and aVF. ST segment elevation in leads V4-V6 and aVL are associated with an anterolateral MI. ST elevation in leads II, III, and all of the precordial leads are consistent with a lateral wall MI. ACS is not associated with changes in leads II, III and aVL. Leads I and aVL are the lateral leads. ST segment depression is indicative of ischemia or an NSTEMI.
A patient with unstable angina requires cardiac catheterization. Which statement should demonstrate the patient understands the post-procedural teaching?
A. "I will be able to go home as soon as the dressing is removed from my leg."
B. I will have to lie flat until the next day so I don't have circulation problems in my leg."
C. "I will have my blood sugar checked a lot in case my diabetes flares up."
D. "I will receive IV fluids and need to urinate a lot to protect my kidneys."
What is D. "I will receive IV fluids and need to urinate a lot to protect my kidneys."?
Due to the contrast used during the procedure, the patient will require more IV fluids to excrete the contrast.
A patient is admitted after a PCI to the RCA. Four
hours later, the patient’s data are:
BP 76/48, HR 120, RR 32, SpO2 95%
ST segment changes are noted
The nurse should suspect
A. pulmonary embolism.
B. abrupt reclosure.
C. coronary artery dissection.
D. restenosis of the right coronary artery.
What is C. coronary artery dissection?
Abrupt reclosure should be suspected with marked hypotension and ST segment changes following PCI. Patients with a pulmonary embolism will not typically have an SpO2 of 95%; it would be much lower. Coronary artery dissection may be a consequence of an intramural hematoma of a coronary artery, resulting in a false lumen that compresses a true lumen with myocardial ischemia. Symptoms can range from unstable angina to sudden death. If the right coronary artery is narrowed, the patient will have chest pain, shortness of breath, or both.
The rationale for using dobutamine at an infusion of 10-12 mcg/kg/min for cardionegic shock is to:
A. decrease myocardial ischemia
B. improve urinary output
C. decrease oxygen consumption
D. improve myocardial contraction
What is D. improve myocardial contraction?
Dobutamine directly stimulates β1 and α1 receptors, with weak affinity for β2 receptors, resulting in direct regulation of mean arterial pressure by increasing cardiac output, at the expense of SV and heart rate
The rhythm shown below MAY be associated with
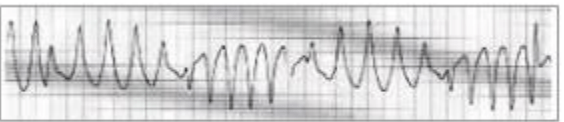
A. left ventricular aneurysm
B. cardiogenic shock
C. atropine adminstration
D. procainamide administration
What is D. procainamide administration?
The electrocardiogram may reflect these effects by showing slight sinus tachycardia (due to the anticholinergic action) and widened QRS complexes and, less regularly, prolonged Q-T and P-R intervals (due to longer systole and slower conduction), as well as some decrease in QRS and T wave amplitude.
Which parameter indicates successful management of right ventricular (RV) failure?
A. decreased CVP
B. decreased PAOP
C. increased PAD
D. increased RV pressure
What is A. decreased CVP?
The goal in RV failure is to decrease right-sided pressure. The PAOP and PAD are not elevated in RV failure.
A patient states "I have pain radiating down my back and legs."
Upon assessment, BP is 190/105, distal peripheral pulses are weak, and there is a loud systolic murmur present. The nurse should suspect
A. descending aortic dissection
B. mitral valve stenosis
C. ascending aortic dissection
D. aortic valve stenosis
What is A. descending aortic dissection?
When an aortic dissection occurs, one may experience symptoms similar to those of a heart attack:
- Pain: You may experience sudden severe pain in the chest, back or abdomen. A radiating pain in the chest or upper back is described as a tearing or ripping sensation. The pain can extend to the legs and make walking difficult.
- Difficulty breathing: You may feel short of breath or lose consciousness.
- Paralysis: You may lose vision, the ability to speak, or the ability to use limbs on one or both sides of your body.
- Weak pulse: Because less blood is circulating in your body, you may notice a weakened pulse.
A patient is admitted complaining of crushing chest pain, which began 2 hours ago. An ECG shows ST elevation in leads V 2-V 4, which is treated with a PCI procedure to the LAD. Following the procedure the patient develops oliguria and bilateral, diffuse crackles. Which hemodynamic findings should be expected at this point?
A. BP 80/50, CO 3.8, SVR 2200, PA Pressure 40/24
B. BP 86/50, CO 5.0, SVR 1000, PA Pressure 30/10
C. BP 85/56, CO 2.9, SVR 660, PA Pressure 20/14
D. BP 90/60, CO 6.8, SVR 500, PA Pressure 18/4
What is A. BP 80/50, CO 3.8, SVR 2200, PA Pressure 40/24?
This patient had an anterior infarction, which predisposes the development of left ventricular failure/cardiogenic shock. The hemodynamic data of BP 80/50, cardiac output 3.8, SVR 2200 and PA pressure 40/24 are consistent with left ventricular failure/cardiogenic shock. The other hemodynamic data are not consistent with left ventricular failure/cardiogenic shock.
A patient is on a regimen of nitroprusside (Nipride) and nitroglycerin (Tridil). Because of the combined effects of these drugs, the nurse should be alert to the possible development of
A. atrial dysrhythmias, particularly paroxysmal atrial tachycardia.
B. prolonged PR interval and bundle branch block.
C. reduced coronary artery perfusion secondary to hypotension.
D. increased peripheral vascular resistance
What is C. reduced coronary artery perfusion secondary to hypotension.?
Both of these agents are vasodilators, which are known to cause hypotension. If hypotension develops, a decrease in coronary artery perfusion may result even though nitroglycerin is given to increase coronary artery blood flow. There is no significant association between the development of atrial fibrillation, PR interval prolongation or bundle branch block, and nitroprusside or nitroglycerin administration. These agents will decrease peripheral vascular resistance.
An unresponsive patient is admitted with a BP 72/50 and the rhythm shown below:
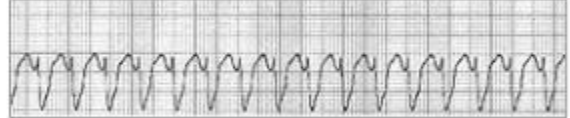
MOST APPROPRIATE therapy in this situation is:
A. cardioversion
B. verapamil 5mg IV
C. lidocaine 1 mg/kg IV
D. defibrillation
What is A. cardioversion?
EXPLAIN WHY TO GET DOUBLE POINTS
Patients with unstable ventricular tachycardia are initially treated with synchronized cardioversion. Unsynchronized delivery of electricity can cause R-on-T phenomenon, which can result in ventricular fibrillation. Lidocaine is not recommended in the current American Heart Association guidelines for the management of unstable ventricular tachycardia. Verapamil is not indicated for the management of wide complex tachycardia.
Left ventricular failure can be caused by
A. aortic regurgitation and hypertension.
B. aortic stenosis and COPD.
C. mitral regurgitation and pulmonary embolus.
D. mitral stenosis and AMI.
What is A. aortic regurgitation and hypertension.?
Aortic regurgitation increases the volume of the left ventricle and left ventricular end-diastolic pressure (LVEDP). Hypertension increases afterload. If uncompensated, stroke volume will decrease due to increased afterload. COPD causes right-sided heart failure. A pulmonary embolus causes increased pressure on the right side of the heart. Mitral stenosis results in decreased filling of the left ventricle.
A patient with a history of angina is admitted to the unit after surgical repair of an abdominal aortic aneurysm (AAA). The patient is receiving a sodium nitroprusside (Nipride) drip for severe postoperative hypertension. Twelve hours later, the patient complains of back pain. Assessment at this time reveals:
BP: 80/60. HR-120. U/O 20mL/hr. +1 Dorsalis pedis pulse bilaterally. After notifying the provider of the change in patient condition, the nurse should anticipate which immediate intervention?
A. administration of normal saline 200 mL/hr and preparation for Doppler studies
B. spiral chest CT and emergent pericardiocentesis
C. procedural sedation and IABP insertion
D. discontinuation of Nipride and preparation for surgery
What is D. discontinuation of Nipride and preparation for surgery?
Nipride must be discontinued because the patient is hypotensive. The patient is also demonstrating signs of postoperative bleeding/ hypovolemic shock. A return to the operating room is indicated. Pulses are present, so there is no need for Doppler studies. Volume resuscitation is an acceptable intervention. Since the pulse pressure is normal, the patient is not manifesting signs of cardiac tamponade.
. A patient with a history of ischemic cardiomyopathy is admitted with a BP of 102/74, HR of 122 with occasional irregular beats, RR of 42, productive cough with frothy sputum, and pitting edema in the lower extremities. The patient is anxious, restless and short of breath. This patient’s primary problem is MOST LIKELY
A. pulmonary edema.
B. pulmonary embolism.
C. acute coronary syndrome.
D. acute papillary muscle rupture.
What is A. pulmonary edema.?
Patients with end-stage coronary artery disease (ischemic cardiomyopathy) may develop fluid overload because of acute decompensation. This patient has classic signs and symptoms of fluid overload resulting in pulmonary edema (e.g., tachypnea, dyspnea, frothy sputum). Pulmonary embolism is possible but will not manifest as frothy sputum or other symptoms of pulmonary edema described in this scenario. Acute coronary syndrome would manifest with ST segment elevation and concomitant angina symptoms. There is no regurgitant murmur described in this scenario. Papillary muscle rupture is usually associated with early onset of acute coronary syndrome - not end-stage coronary artery disease - and does not develop acutely without acute coronary syndrome.
A direct effect of sodium nitroprusside (Nipride) is to
A. decrease stroke volume.
B. increase venous return.
C. decrease afterload.
D. increase pulmonary vascular resistance.
What is C. decrease afterload?
Sodium nitroprusside is an arterial vasodilator. As such, afterload will decrease with its use. It causes an increase in stroke volume due to a decrease in resistance and decreases venous return due to vasodilation.
The ECG is MOST INDICATIVE OF:
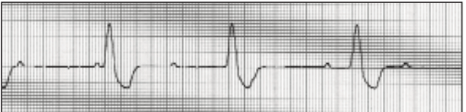
A. 2nd degree AV block, type I (Wenckebach)
B. 2nd degree heart block, type II.
C. 1st degree AV block
D. third-degree AV heart block.
What is D. third-degree AV heart block?
In this ECG strip, the P waves are not in relation to the QRS complexes. The QRS is greater than .10 second. There are no atrial impulses conducting through the AV node to cause ventricular depolarization. The atria and ventricles are each firing independently.
Reference: Morton PG, Fontaine DK. 2018.
A patient is admitted with chest pain and nausea. The ECG shows new deep Q waves in leads I, aVL, V5 and V6. The patient’s ECG pattern is MOST CONSISTENT with a diagnosis of
A. subendocardial infarction.
B. anterior MI.
C. inferior MI.
D. lateral MI. The lateral wall leads are I, aVL, V 5 and V 6 .
What is D. lateral MI.?
The lateral wall leads are I, aVL, V5 and V6.
Following ACS affecting the anterior wall, a patient develops shortness of breath. Assessment reveals moist bibasilar crackles and a moderately loud S3. A PA catheter is inserted, and a PAOP of 22 mm Hg is obtained. These findings are MOST indicative of
A. impending cardiac tamponade.
B. venous distention.
C. tricuspid valve dysfunction.
D. left ventricular decompensation.
What is D. left ventricular decompensation.?
This patient has a risk factor for and signs of left ventricular failure (anterior MI). A rise in the PAOP and an S3 is reflective of increased left ventricular end-diastolic pressure (LVEDP). When pressure in the left ventricle increases suddenly, fluid is forced into the alveoli by an increase in hydrostatic pressure. Consequently, in acute heart failure and acute decompensation, bibasilar crackles occur. Aside from shortness of breath, this patient does not have symptoms consistent with cardiac tamponade. JVD is associated with right-sided failure and an inferior wall MI. JVD is associated with right-sided failure and an inferior wall MI.