What would you do if your patient has a neuro change following IV Tenecteplase administration?
Obtain NIHSS and notify provider IMMEDIATELY. Anticipate a STAT head CT.
Reference:
"Intravenous (IV) Tenecteplase for Acute Ischemic Stroke" Procedure
How do you know if your patient is eligible for mechanical thrombectomy?
There would be a target clot identified via CTA, and viable tissue via CTP. You would likely find this out from the Stroke team.
Reference:
AHA/ASA Clinical Practice Guidelines
How often is stroke education for patients completed and documented?
At least once per shift
When do you conduct a swallow screen (dysphagia screen)? Where do you document it?
Conduct a swallow screen for any patient who is suspected of having a stroke or presenting with new neurological changes. Conduct swallow screen before ANY p.o. intake, including medications.
Document the swallow screen in the complex assessment flowsheet
What does the SMART goals format stand for?
S: Specific M: Measurable A: Achievable R: Relevant T: Timely
If the patient had a Mechanical Thrombectomy, how do you know that it was successful?
Explanation of the intervention can be found in the provider post-op note. A Thrombolysis In Cerebral Infarction (TICI) score is documented in the post-op note. Desirable TICI scores are 2B, 2C or 3.
What is the timeframe for IV Tenecteplase administration?
IV Thrombolytic therapy can be given to eligible patients within 3 hrs of LKW. In some cases, it can be given up to 4.5 hrs from LKW.
Reference:
AHA/ASA Clinical Practice Guidelines
"Intravenous (IV) Tenecteplase for Acute Ischemic Stroke" Procedure
What is documented post-TCAR or CEA? What frequency are these items documented?
Vital Signs, Neuro Check, Cranial Nerves
Q15min X 1 hr
Q30 min X 2 hrs
Q60min X 21 hours
*RFI
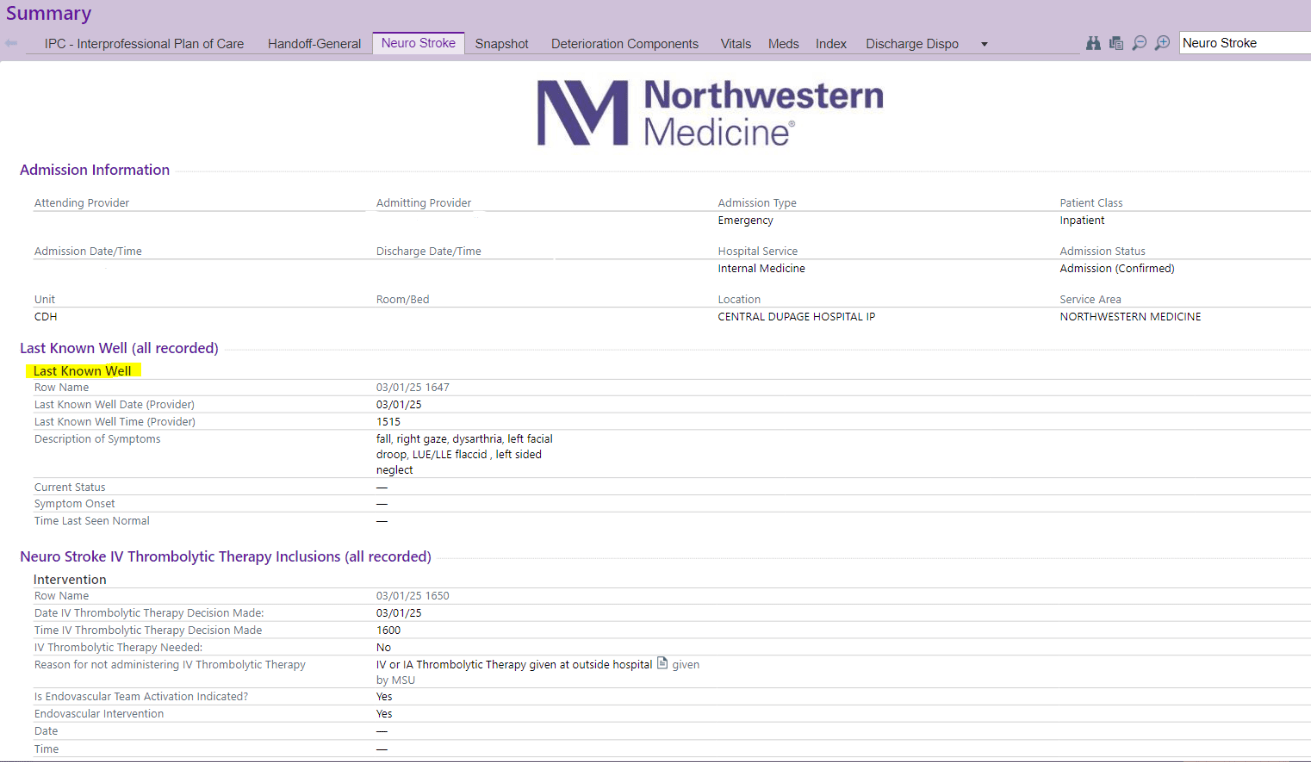
Where do you find documentation on "Last Known Well (LKW)"?
LKW is documented during the initial stroke consult.
It can be found on the Neuro Stroke tab or in provider notes.
What bedside swallow screen tool do we use?
Rapid Aspiration Screen for Suspected Stroke (RAS³)
What education do you receive for stroke care?
Annual Stroke Module in MyLearning
NIHSS every other year
Unit specific education days
How do you know if IV Tenecteplase was considered for your patient?
This determination is made during the initial stroke consult.
It can be found on the Neuro Stroke tab or in provider notes.
What are BP parameters to safely administer IV Tenecteplase?
<185/110
"Intravenous (IV) Tenecteplase for Acute Ischemic Stroke" Procedure
How frequently do you check VS/neuro checks/puncture site after mechanical thrombectomy?
Q 15 min X 2hrs
Q 30 min X 6 hrs
Q 60 min X 16 hrs
Reference:
AHA/ASA Clinical Practice Guidelines
"Intravenous (IV) Tenecteplase for Acute Ischemic Stroke" Procedure
How do you know if a stroke order set was used for a patient?
This can be found on the bottom of the Neuro Stroke Tab.
If the patient’s symptoms resolve, can you perform another swallow-screen for the patient?
NO! The patient must be evaluated by Speech Therapy prior to any p.o. intake if they failed the bedside swallow screen.
How many hours of stroke specific education do you need every year?
Per CDH Education Plan:
3B/3ICU Staff RNs 4 hr/yr
3B/ICU CSC 8 hr/yr
ED CSC/Staff RNs 4hr/yr
ED Techs 2 hr/yr Nursing resource (intermediate/critical care/WR floats, and system resource) 4 hr/yr
4ABC/3South CSC 4 hr/year
4ABC/3 South Staff RNs 2 hr/yr
Neuro IR RNs 4 hrs/yr
How do you know what therapy recommends for your stroke patient?
Therapy recommendations from SLP, PT, and OT can be found in their notes. Some recommendations also pull into the Interprofessional Plan of Care (IPC) tab.
What are BP parameters post IV Tenecteplase administration?
<180/105
"Intravenous (IV) Tenecteplase for Acute Ischemic Stroke" Procedure
https://nm.ellucid.com/documents/view/16465
What are BP parameters post mechanical thrombectomy?
<180/105
Unless otherwise specified by a provider
Reference:
AHA/ASA Clinical Practice Guidelines
Your stroke patient refuses their SCDs, what should you do?
All stroke patient should have SCDs ordered unless contraindicated.
-Educate the patient on the importance of SCDs
-Document refusal in Cares flowsheet
-Notify Provider of refusal
What do you do if the patient fails the swallow screen?
Make the patient NPO, obtain order for Speech Therapy consult, and notify provider.
Why are personal risk factors important and where do you document them?
The best way to prevent future strokes is to educate patients based on their personal risk factors for stroke. Teach them which risk factors are modifiable, and how to modify them. Document personal risk factors in the Stroke Education template.
How do you locate Clinical Practice Guidelines for stroke?
CDH Stroke Microsoft Teams site
How do you administer IV Tenecteplase?
The IV Tenecteplase dose is calculated as 0.25mg/kg.
(1) Withdraw 10ml of sterile water using the 10ml syringe.
(2) Inject the 10ml of sterile water into the Tenecteplase vial, directing the sterile water at the powder.
(3) Gently swirl the Tenecteplase vial until contents are fully dissolved. DO NOT SHAKE. The solution should be colorless or pale yellow and transparent. The concentration of the Tenecteplase vial is now 5mg/ml.
(4) Using the verified order in EPIC and the stroke dosing table, draw up the appropriate Tenecteplase dose in a separate 5 mL luer lock syringe.
It is given as a IV push over 5 seconds. Be sure to flush with 10ml 0.9% sodium chloride post administration. The max dose of Tenecteplase for stroke treatment is 25mg.
Why was the Stroke Alert window expanded to LKW within 24 hrs in 2018?
The AHA/ASA Clinical Practice Guidelines were updated in Jan. 2018. They now state that it is beneficial to do mechanical thrombectomy up to 24 hrs from LKW for certain eligible patients. CDH expanded the window to capture this population.
Reference:
"Stroke Alert” Procedure
and
AHA/ASA Clinical Practice Guidelines
What does the modified Rankin scale (mRS score) measure? When are you required to document it?
mRS is a functional status scale that measures the degree of disability. Use the algorithm on the back of the red core measure sheet to properly score the patient. The mRS needs to be documented for: • Pre-admit (baseline status) • Admit (status at stroke symptom onset) • Discharge (Discharge status) These incremental scales are used to track stroke patient outcomes.
Remember:
The pre-admit and the admit mRS can be the same, but the pre-admit mRS should never be higher than the admit mRS. That would mean the patient’s baseline status was worse than when they came to the hospital.
What do you do if your NPO stroke patient has orders for oral route medications?
Notify provider to get route changed i.e. IV or via feeding tube. Patients who are NPO with a feeding tube should not have oral route medications documented in the MAR.
*A comment placed to correct the route is not appropriate; the order must be changed to reflect the correct route
Your patient is an 67 year old male with PMHx (confirmed with patient) of hypertension, tobacco abuse and GERD
Admitted 2 days ago for a CVA, with incidental finding of severe carotid stenosis and had a CEA today. Is the below stroke education compliant?
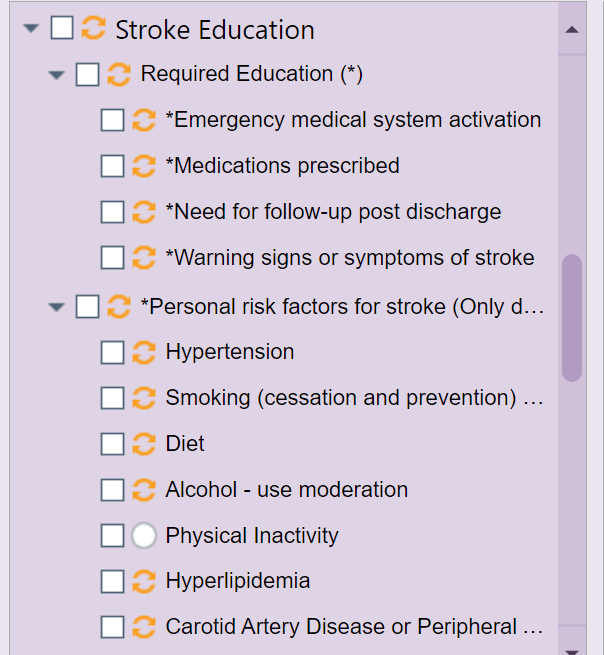
No, the patient does not have a history of hyperlipidemia.
Who is eligible for IV Tenecteplase? What is a resource you can use to look at inclusion exculsion criteria?
Inclusion/Exclusion criteria for IV Tenecteplase is located on the CDH Stroke Microsoft Teams site.
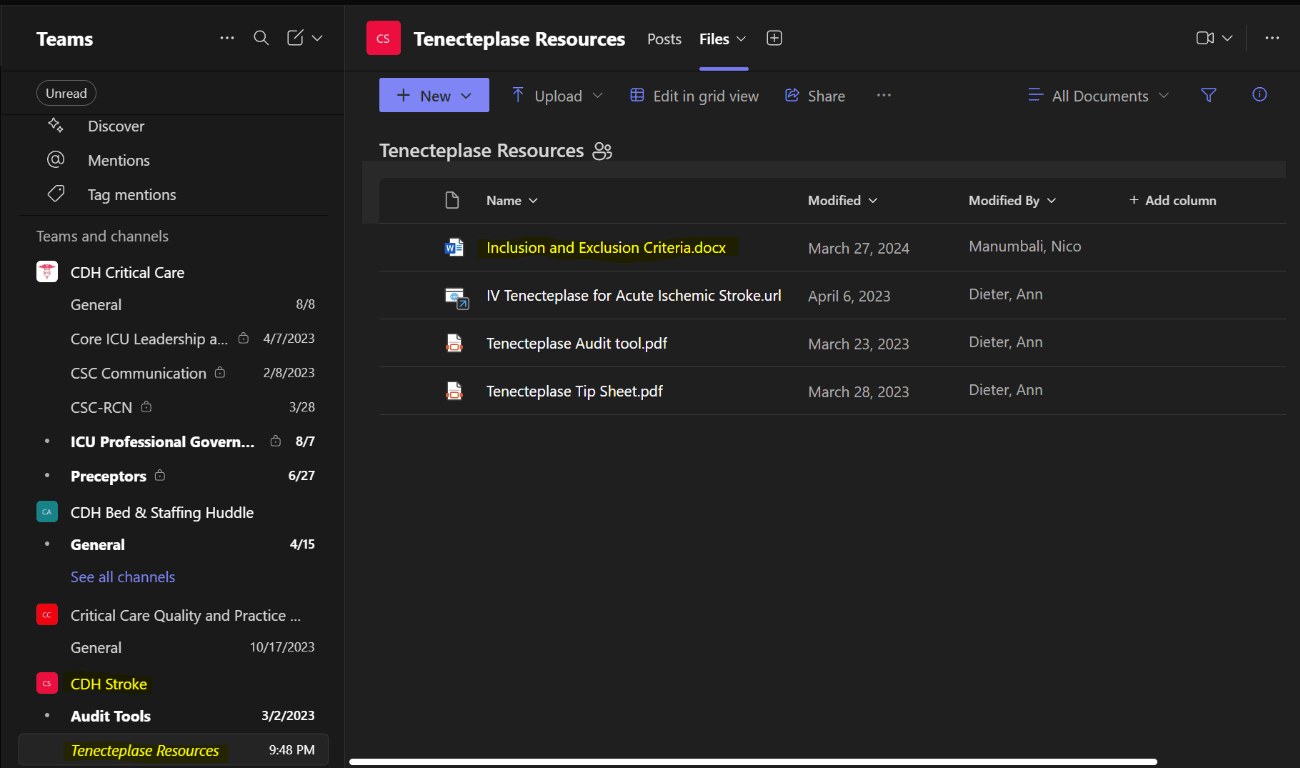
Reference:
CDH Stroke Teams site
AHA/ASA Clinical Practice Guidelines
What are the two most common adverse effects of IV Tenecteplase?
1. Bleeding (watch for signs of hemorrhagic conversion)
2. Angioedema
Reference:
"Intravenous (IV) Tenecteplase for Acute Ischemic Stroke" Procedure
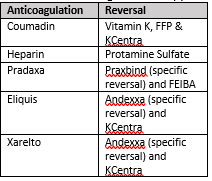
What medications would you anticipate giving a HEMORRHAGIC stroke patient on anticoagulation?
"Intravenous (IV) Tenecteplase for Acute Ischemic Stroke" Procedure
How do you monitor/document vital signs with vasoactive infusions?
Follow the Titrating IV Medications and Block Charting Procedure PROCEDURE: A. While these medications are being titrated to their prescribed therapeutic effects or weaned, the physiologic parameter is monitored and recorded every 2 minutes to every 4 hours depending on the order, the patient’s condition and response. B. When the desired therapeutic effect has been reached and the medication is no longer being titrated, or is weaned off, the physiologic parameter is monitored and recorded in 15 minutes x1 then every 1-4 hours depending on the order, the patient’s condition and response. C. The nurse is responsible for validation of vital signs in the electronic medical record.
Your stoke patient has an order for a supplement but they continue to refuse it, what should you do?
-Document patient's refusal
-Let the dietician know so they can modify or discontinue the supplement. (supplements can be costly, and may continue to be delivered if the order is not modified)
What is the difference between Clinical Practice Guidelines and Clinical Pathways?
Clinical Practice Guidelines are journal articles published by the AHA/ASA. All stroke related policies and procedures are formed out of the Clinical Practice Guidelines.
The Clinical Pathways are internal documents that take the info in the Clinical Practice Guidelines and put it in a more readable/useable format. They are in a table format, and a great reference for daily stroke care.
Both are located on the CDH Stroke Microsoft Teams site
How do you locate Stroke Program Outcomes?
Our scorecard can be located on the CDH Stroke Microsoft Teams site.