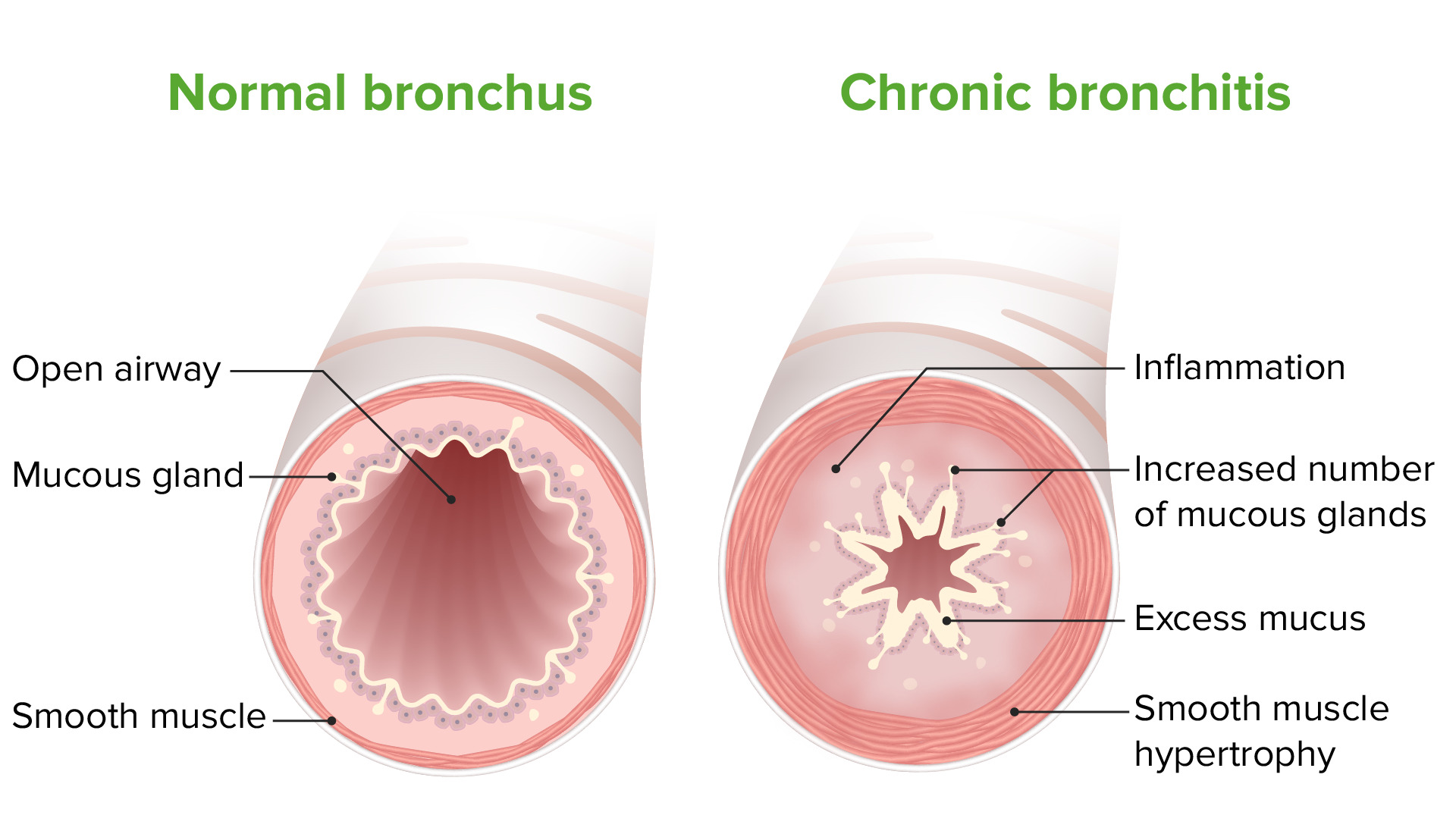
Diagnosis of a patient with a productive cough for at least 3 months each year for 2 consecutive years
Chronic Bronchitis
- Promotion of goblet cell proliferation and hypertrophy, mucus secretion, and impaired ciliary function → chronic productive cough
- Inflammation mediated by CD8+ T lymphocytes
- Reid index characteristic of chronic bronchitis is > 0.5 (the ratio of the thickness of the submucosal mucus-secreting glands to the thickness between the epithelium and cartilage in the bronchial tree)
3 depictions of reversible airflow obstruction in asthma
1. Coughing
2. End-expiratory Wheezing
3. Dyspnea
Antihypertensive medication that can cause cough due to accumulation of bradykinin
ACE Inhibitors
First line diagnostic test in patients with suspected asthma
PFTs
What is the x-ray finding and the diagnosis?

Hyperinflation (barrel chest) and emphysema
-PE will show hyperresonant lungs, decreased breath sounds, accessory muscle use for breathing
2 types of asthma
Allergic asthma (most common)
Nonallergic asthma (uncommon)
Young child presents with coughing, wheezing, foul-smelling sputum, does not respond to bronchodilators
Foreign body aspiration
The most common cause of community-acquired pneumonia across all age groups
streptococcus pneumoniae
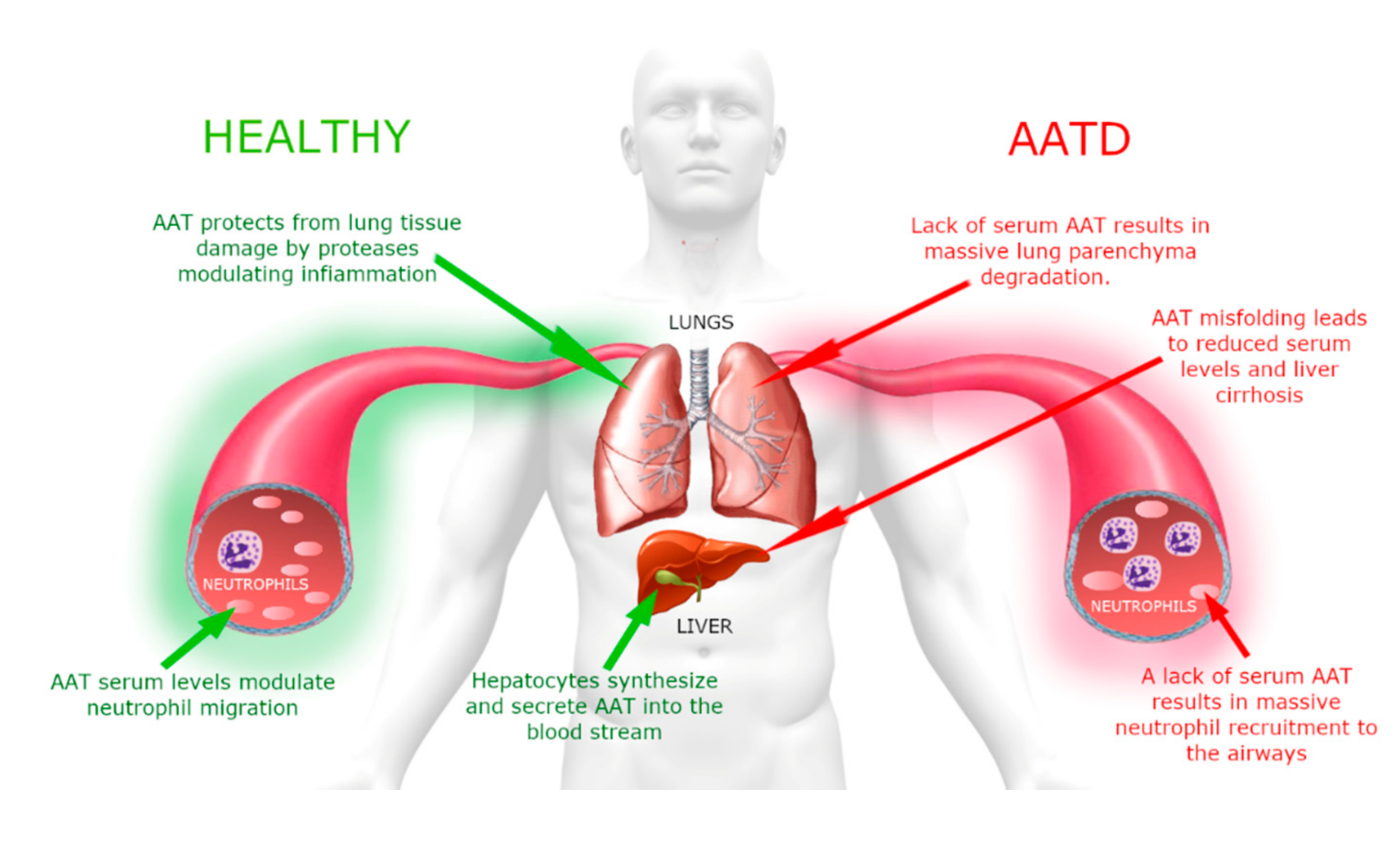
An endogenous risk factor for emphysema
alpha1-Antitrypsin deficiency
-Panlobar (panacinar) emphysema subtype
-Will typically see liver manifestations as well, like jaundice
-Should screen all patients for this at time of diagnosis
True or false?
Characteristic findings of pulmonary function testing in asthmatics include:
1. Obstructive pattern
2. Reversibility of obstruction w/ medication
3. Variability w/ repeat testing
True
Patient presents to clinic with fever, cough, dyspnea. CBC shows neutrophilic leukocytosis, chest xray shows infiltrates. Antibiotic treatment?
B-lactams, Macrolides (azithromycin), Fluoroquinolones, or Doxycycline
Short acting β2-agonist that directly induces bronchodilation and used in the treatment of acute asthma exacerbation
Albuterol
Methylxanthines (e.g. theophylline) can be used to treat COPD. What is the mechanism of action?

Nonselectively antagonize adenosine receptors and inhibit phosphodiesterase
- Used in severe and refractory cases
- It acts as a competitive nonselective phosphodiesterase inhibitor (inhibiting type III and type IV phosphodiesterase), which increases the concentration of intracellular cAMP, activates protein kinase A, inhibits TNF-alpha, and leukotriene synthesis, and also decreases inflammation and innate immunity.
- It is also a nonselective adenosine receptor antagonist. It acts on A1, A2, and A3 receptors with almost the same affinity, which possibly explains theophylline's cardiac effects. Adenosine-mediated channels also increase the contraction force of diaphragmatic muscles by enhancing their calcium uptake
- Relaxation of the bronchial musculature → bronchodilation
Inflammatory process is driven by which type of immune cell?
Th2-cell


A child presents with a fever, barking cough, and inspiratory stridor - what virus is responsible
Parainfluenza virus
PFT shows: increased residual volume, decreased FEV1, decreased FEV1/FVC, normal DLCO. Diagnosis?
Chronic Bronchitis
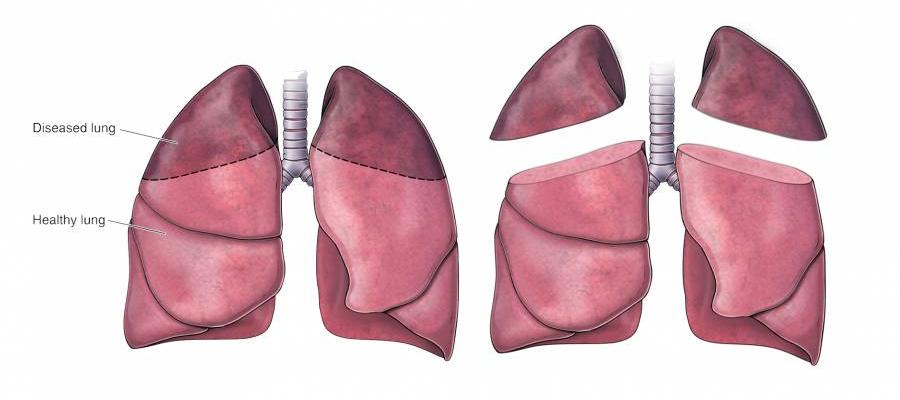
A surgical procedure that involves a wedge excision of emphysematous tissue to help in the treatment of COPD
Lung Volume Reduction Surgery (LVRS)
- Helps by reducing the size of hyperinflated lungs, thus improving expiratory airflow in the non-diseased lungs
- Studies show that elastic recoil of the lungs may improve after LVRS, which in turn improves the expiratory airflow in the lungs
- There are extensive criteria for LVRS including notable airflow obstruction on spirometry, evidence of air trapping on lung volume measurements, and CT findings of heterogeneously distributed emphysema
Can you name the 6 different classes of medications most commonly used to treat asthma?
1. Short-Acting Beta Agonist (SABA)
2. Short-Acting Muscarinic Antagonist (SAMA)
3. Long-Acting Beta Agonist (LABA)
4. Long-Acting Muscarinic Antagonist (LAMA)
5. LeukoTriene-Receptor Antagonist (LTRA)
6. Steroids
Goal is to decrease parasympathetic tone and bronchial inflammation as much as possible!
Pt presents with sudden shortness of breath, chest pain, and coughing up blood - what lab test/imaging to order
D-dimer/CTA
PFT shows: increased residual volume, decreased FEV1, decreased FEV1/FVC, and decreased DLco. Diagnosis?
Emphysema
