What two rhythms are considered shockable during CPR?
Ventricular fibrillation and pulseless ventricular tachycardia
Why is ETCO2 monitoring considered one of the most reliable predictors of CPR effectiveness in vet med?
ETCO2 reflects cardiac output during CPR. Higher ETCO2 indicates more effective compressions and better perfusion. A sudden increase often predicts ROSC
What is the first thing you should do if you find a pet unresponsive?
ABC's! First, check if the animal has a clear airway, provide ventilation once the airway is secured, begin chest compressions immediately if the patient has no pulse or heartbeat.
How often should team members switch roles during chest compressions to prevent fatigue?
Every 2 minutes!
Bonus: How long does it take to regain the progress made if compressions are stopped too early?
What is the first-line drug used in veterinary CPR to stimulate the heart?
Epinephrine
Bonus: What can be caused by giving too high of an Epi dose?
What is the recommended biphasic defibrillation dose for dogs and cats?
2–4 J/kg
You are doing chest compressions on a cat in lateral recumbency. The EtCO₂ reading suddenly drops from 25 mmHg to 8 mmHg without changes in technique.
Possible dislodgement of the endotracheal tube, equipment disconnect (must confirm visually; however more pertinent during anesthesia and not in CPR events), or decreased perfusion/impending fatigue of compressor. First, quickly check the airway/equipment while continuing compressions.
What is the recommended compression-to-breath ratio for single rescuer CPR in animals?
30:2
What percent of perfusion are chest compressions producing?
30%
What is the recommended IV/IO dose of epinephrine during CPR?
0.01 mg/kg (low dose) every other round
What is happening in this ECG?
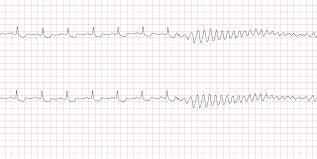
Sinus rhythm progressing into ventricular fibrillation
A dog in cardiac arrest has severe anemia from trauma. You start compressions and ventilation.
Why might CPR be less effective, and what additional intervention is critical?
Hypovolemia reduces preload and forward flow during compressions; rapid IV fluids or blood transfusion is needed for effective resuscitation.
The “cardiac pump” theory of CPR is most relevant in what size group of patients?
Small dogs and cats
The sudden, sustained increase in this value is the earliest indicator of ROSC.
EtCO₂
During CPR on a 30 kg dog, the team has been giving epinephrine every 2 minutes along with compressions. After 12 minutes, the ECG shows asystole and EtCO₂ remains < 8 mmHg.
What mistakes are being made, and what should change in the protocol?
Mistake 1: Epinephrine is being given too frequently — it should be every 3–5 minutes, not every 2.
Mistake 2: Asystole with persistently low EtCO₂ after prolonged efforts carries a grave prognosis — focus should remain on optimizing compression quality and considering reversible causes, but recognize when CPR may no longer be effective.
What rhythm is this? What do you do next?
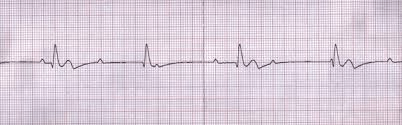
PEA (pulseless electrical activity) a non-shockable rhythm, continue compressions/ administer drugs
A 25 kg mixed-breed dog presents in cardiac arrest. CPR is initiated with proper compressions, intubation, and ventilation. After 12 minutes, ECG shows organized complexes without a palpable pulse. EtCO₂ has remained around 7 mmHg, despite switching compressors and confirming technique. The patient has a history of urethral obstruction earlier today, but treatment was delayed.
What is the most likely underlying cause of the arrest, what specific treatment should be given in addition to CPR drugs, and why has resuscitation been ineffective so far?
Hyperkalemia secondary to urethral obstruction.
Severe hyperkalemia prevents depolarization of cardiac myocytes → organized ECG activity without effective contractions (PEA). Chest compressions alone cannot overcome this without correcting the electrolyte abnormality.
Why is full chest recoil between compressions important?
It allows venous return to the heart, optimizing cardiac output
Why is hyperventilation harmful during CPR?
Interrupts Chest Compressions, causes Hypocapnia (low CO₂), decreases Coronary Perfusion Pressure (CPP), increases Intrathoracic Pressure.
ETCO2 is 12 mmHg with appropriate ventilation and you notice your compressor is compressing about 1/3 of the chest depth of your patient. What is something that you can change?
Increase compression depth to 1/2