Regulated by ADH, thirst, renin-angiotensin-aldosterone system.
How is Sodium regulated in the body?
The period of 2-3 weeks after continuous TB medication therapy.
How much time before patients with TB are no longer infectious?
Serum >10.5 mg/dL
What is the serum level for hypercalcemia?
- Transports and metabolizes glucose for energy
- Stimulates storage of glucose in the liver and muscle (in the form of glycogen)
- Signals the liver to stop the release of glucose
- Enhances storage of dietary fat in adipose tissue
- Accelerates transport of amino acids (derived from dietary protein) into cells
- Inhibits the breakdown of stored glucose, protein, and fat
What is the function of insulin?
Most abundant electrolyte in the ECF.
What is Sodium?
Intravascular Fluid (the fluid within the blood vessels), Interstitial Fluid (contains the fluid that surrounds the cell and totals about 11 to 12 L in an adult), & Transcellular Fluid (cerebrospinal, pericardial, synovial, intraocular, and pleural fluids, sweat, and digestive secretions) that consists of 20% of the body weight.
What makes up Extracellular Fluid compartment ---extracellular space (fluid outside the cells) ?
The term to describe rapid onset, severe, and persistent asthma that does not respond to conventional therapy.
What is status asthmaticus?
There is a reduced PaO2 and initial respiratory alkalosis, with a decreased PaCO2 and an increased pH. As status asthmaticus worsens, the PaCO2 increases and the pH decreases, reflecting respiratory acidosis.
98-106 mEq/L of Intracellular Concentration and 3-4 mEq/L of Extracellular Concentration.
What are the normal values of Chloride?
The three P's of Diabetes!
What are Polyuria (Increased Urination), Polydipsia (Increased thirst), & Polyphagia (Increased appetite)?
Incomplete emptying of alveoli during expiration due to loss of lung tissue elasticity (emphysema), bronchospasm (asthma), or airway obstruction.
What is air-trapping?
Primary anion of the ICF. About 85% is located in bones and teeth, 14% in soft tissue, and less than 1% in the ECF
What is Phosphorus?
It measures the lungs abilities to oxygenate blood and remove carbon dioxide.
What is the purpose of an arterial blood gas analysis?
(1.3 mg/dL [0.62 mmol/L]) or lower and is frequently associated with hypokalemia and hypocalcemia.
What are the values for Hypomagnesemia?
A metabolic derangement in type 1 diabetes that results from a deficiency of insulin; highly acidic ketone bodies are formed, resulting in acidosis.
What is Diabetic Ketoacidosis (DKA)?
Approximately two thirds of body fluid is in the this compartment and is located primarily in the skeletal muscle mass, accounting for 40% of the body weight.
What is the Intracellular fluid (ICF) compartment which consists of the intracellular space (fluid in the cells)?
Anorexia, nausea and vomiting, headache, lethargy, dizziness, confusion, muscle cramps and weakness, muscular twitching, seizures, papilledema, dry skin, ↑ pulse, ↓ BP, weight gain, edema.
What are the signs and symptoms of Hyponatremia?
Reversible diffuse airway inflammation that leads to long-term airway narrowing. This narrowing, which is exacerbated by various changes in the airway, includes bronchoconstriction, airway edema, airway hyperresponsiveness, and airway remodeling.
What is the Pathophysiology of Asthma?
serum level exceeds 4.5 mg/dL (1.5 mmol/L). Usually corresponds with low calcium levels.
What is Hyperphosphatemia?
BLANK is absorbed before other nutrients and does not require insulin for absorption. Large amounts can be converted to fats, increasing the risk for DKA, so moderation is recommended.
What is Alcohol?

Produce a more rapid effect that is of shorter duration than regular insulin. Because of their rapid onset, the patient should be instructed to eat no more than 5 to 15 minutes after injection. Not suitable for Type 1 and some Type 2 Diabetes.
What are rapid-acting insulins?
Muscle weakness, tachycardia → bradycardia, dysrhythmias, flaccid paralysis, paresthesias, intestinal colic, cramps, abdominal distention, irritability, anxiety. ECG: tall tented T waves, prolonged PR interval and QRS duration, absent P waves, ST depression
What are the signs and symptoms of Hyperkalemia?
isoniazid (INH), rifampin (Rifadin), pyrazinamide (PZA), and ethambutol (Myambutol) for 6-12 months.
What are the drugs to treat Tuberculosis and how long are they taken for?
Value below 2.5 mg/dL (0.8 mmol/L). May develop in malnourished patients who receive parenteral nutrition if the loss is not corrected. Other causes include heat stroke, prolonged intense hyperventilation, alcohol withdrawal, poor dietary intake, diabetic ketoacidosis, respiratory alkalosis, hepatic encephalopathy, and major thermal burns. Low magnesium levels, low potassium levels, and hyperparathyroidism related to increased urinary losses of contribute as well.
What is the value of Hypophosphatemia?
A metabolic disorder of type 2 diabetes resulting from a relative insulin deficiency initiated by an illness that raises the demand for insulin.
What is Hyperglycemic Hyperosmolar Syndrome (HHS)
Increase in the red blood cell concentration in the blood; in COPD, the body attempts to improve oxygen carrying capacity by producing increasing amounts of red blood cells.
What is Polycythemia?
Headache, confusion, drowsiness, increased respiratory rate and depth, nausea, and vomiting, decreased blood pressure, cold and clammy skin, dysrhythmias, and shock. Peripheral vasodilation and decreased cardiac output occur when the pH drops to less than 7.
What are the signs and symptoms of Metabolic Acidosis?
An inflammation of the lung parenchyma caused by various microorganisms, including bacteria, mycobacteria, fungi, and viruses.
What is pneumonia?
Answer: HCO3_ = 22–26 mEq/L.
Learning tip: Kidneys regulate the NORMAL level in the ECF; they can regenerate, as well as reabsorb them from the renal tubular cells. The body’s major extracellular buffer system is the BLANK-BLANK BLANK buffer system.
Question: What are normal Bicarbonate levels?
Learning tip: Bicarbonate-carbonic acid buffer system.
SMBG. It is a key component of treatment for any intensive insulin therapy regimen (i.e., 2 to 4 injections per day or the use of an insulin pump) and for diabetes management during pregnancy. It is also recommended for patients with the following conditions:
- Unstable diabetes (severe swings from very high to very low blood glucose levels within a 24-hour day)
- A tendency to develop severe ketosis or hypoglycemia
- Hypoglycemia without warning symptoms
For patients not taking insulin, SMBG is helpful for monitoring the effectiveness of exercise, diet, and oral antidiabetic agents
What is Self-Monitoring Blood Glucose?
Low-grade fever, cough, night sweats, fatigue, and weight loss. The cough may be nonproductive, or mucopurulent sputum may be expectorated. Hemoptysis also may occur.
What are the signs and symptoms of TB?
Lightheadedness due to vasoconstriction and decreased cerebral blood flow, inability to concentrate, numbness and tingling from decreased calcium ionization, tinnitus, and sometimes loss of consciousness. Cardiac effects include tachycardia and ventricular and atrial dysrhythmias. PaCO2 is less than 38 mm Hg
What are the signs and symptoms of Respiratory Alkalosis?
Spread or dissemination of TB infection to nonpulmonary sites of the body. It is the result of invasion of the bloodstream by the tubercle bacillus. Usually, it results from late reactivation of a dormant infection in the lung or elsewhere.
What is miliary TB?
↑pH and HCO3– HCO3– >26 mEq/L
What are the values for Metabolic Alkalosis?
Polyuria, polydipsia (increased thirst), and marked fatigue. Blurred vision, weakness, and headache. Patients with marked intravascular volume depletion may have orthostatic hypotension (drop in systolic blood pressure of 20 mm Hg or more on changing from a reclining to a standing position).
Can lead to gastrointestinal symptoms, such as anorexia, nausea, vomiting, and abdominal pain. The patient may have acetone breath (a fruity odor). In addition, hyperventilation (with very deep, but not labored, respirations) may occur. These Kussmaul respirations represent the body’s attempt to decrease this condition, counteracting the effect of the BLANK buildup. In addition, mental status varies widely. The patient may be alert, lethargic, or comatose.
What are the clinical manifestations (signs and symptoms) of DKA, Diabetic Ketoacidosis?
Most common cause of BLANK is kidney injury. A surplus can also result from excessive BLANK given to treat hypertension of pregnancy. Increased serum levels can also occur in adrenocortical insufficiency, Addison disease, or hypothermia. Excessive use of antacids OR laxatives, and medications that decrease GI motility, including opioids and anticholinergics, can also increase serum levels. Lithium intoxication can also cause an increase in serum levels. Extensive soft tissue injury or necrosis as with trauma, shock, sepsis, cardiac arrest, or severe burns can also result in BLANK. ECG findings may include a prolonged PR interval, tall T waves, a widened QRS, and a prolonged QT interval, as well as an atrioventricular block.
What is Hypermagnesemia?
Occurs in emergency situations, such as acute pulmonary edema, aspiration of a foreign object, atelectasis, pneumothorax, and overdose of sedatives, as well as in nonemergent situations, such as sleep apnea associated with morbid obesity. Also can occur in diseases such as muscular dystrophy, multiple sclerosis, myasthenia gravis, and Guillain–Barré syndrome.
What causes Acute Respiratory Acidosis?
Accumulation of purulent material in the pleural space.
What is empyema?
Level decreases to less than 3 mEq/L (3 mmol/L). If prolonged, can lead to an inability of the kidneys to concentrate urine, causing dilute urine (resulting in polyuria, nocturia) and excessive thirst. Depletion suppresses the release of insulin and results in glucose intolerance. Flat T waves or inverted T waves or both, suggesting ischemia, and depressed ST segments. An elevated U wave.
What are values for Hypokalemia?
A measure of glucose control that is a result of glucose molecule attaching to hemoglobin for the life of the red blood cell (120 days).
What is Glycated Hemoglobin (glycosylated hemoglobin, HgbA1C, or A1C)?
The insulin is absorbed very slowly over 24 hours and can be given once a day. Because the insulin is in a suspension with a pH of 4, it cannot be mixed with other insulins because this would cause precipitation.
What are "Peakless" basal, or very long-acting insulins?
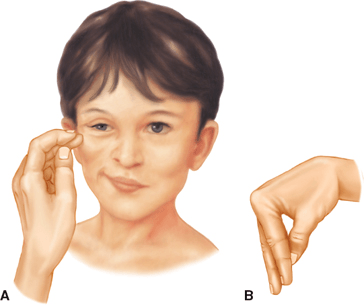 A: Contraction of the facial muscles elicited in response to light tap over the facial nerve in front of the ear B: Carpopedal spasm induced by inflating a blood pressure cuff above systolic blood pressure. Associated with Hypocalcemia.
A: Contraction of the facial muscles elicited in response to light tap over the facial nerve in front of the ear B: Carpopedal spasm induced by inflating a blood pressure cuff above systolic blood pressure. Associated with Hypocalcemia.
What are a Chvostek sign and a Trousseau sign?
Nonspecific pulmonary response to a variety of pulmonary and nonpulmonary insults to the lung; characterized by interstitial infiltrates, alveolar hemorrhage, atelectasis, decreased compliance, and refractory hypoxemia.
What is Acute Respiratory Distress Syndrome (ARDS)?
Blood glucose levels may vary between 300 and 800 mg/dL (16.6 and 44.4 mmol/L). Some patients have lower glucose values, and others have values of 1000 mg/dL (55.5 mmol/L) or higher. Serum bicarbonate (0 to 15 mEq/L) and pH (6.8 to 7.3) values. PCO2 10 to 30 mm Hg.
What are the lab values for Diabetic Ketoacidosis?
Initially, 0.9% sodium chloride (normal saline [NS]) solution is given at a rapid rate, usually 0.5 to 1 L per hour for 2 to 3 hours. Half-strength NS (0.45%) solution (also known as hypotonic saline solution) may be used for patients with hypertension or hypernatremia and those at risk for heart failure. After the first few hours, half-strength NS solution is the fluid of choice for continued rehydration, provided the blood pressure is stable and the sodium level is not low. Moderate to high rates of infusion (200 to 500 mL per hour) may be needed for several more hours. When the blood glucose level reaches 300 mg/dL (16.6 mmol/L) or less, the IV solution may be changed to dextrose 5% in water (D5W) to prevent a precipitous decline in the blood glucose level.
How is Diabetic Ketoacidosis treated?
An abundant intracellular cation. It acts as an activator for many intracellular enzyme systems and plays a role in both carbohydrate and protein metabolism. The normal serum level is 1.3 to 2.3 mg/dL (0.62 to 0.95 mmol/L)
What is Magnesium?