Which of the following is a second generation cephalosporin?
a) Cefuroxime
b) Cefixime
c) Cefotaxime
d) Ceftazidime
First gen cephalosporins
Oral - Cephalexin
IV/IM - cefazolin
Second gen cephalosporins
Oral - Cefaclor, Cefuroxime
Third gen cephalosporins
Oral: Cefixime, Cefpodoxime, Cefdinir
IV: Ceftriaxone, Cefotaxime, Ceftazidime
IM: Ceftriaxone
4th gen
Cefepime
5th gen
Ceftaroline
a) Pyridoxine
b) Thiamine
c) Cyanocobalamin
d) Riboflavin
Isoniazid and it's metabolites bind to pyridoxine and it's active form, pyridoxal 5'- phosphate. This forms a hydrazone complex that is inactive and excreted in the urine reducing the body's pyridoxine supply.
INH inhibits the enzyme pyridoxine phosphokinase which is responsible for converting pyridoxine into it's active form PLP
Which of the following groups of antibiotics are commonly associated with oto and vestibulotoxicity?
Bonus 1000 if you know a drug that can decrease ototoxicity in conjunction with the answer
a) Aminoglycosides
b) Monobactams
c) Tetracyclines
d) Carbapenems
Aminoglycosides are commonly associated with oto and vestibular toxicity.
Bind to 30S subunit of the bacterial ribosome → irreversible inhibition of initiation complex → inhibition of bacterial protein synthesis → cell death (bactericidal effect)
- Misreading of mRNA
- Blockage of translocation
- Synergistic effect when combined with β-lactam antibiotics: β-lactams inhibit cell wall synthesis → facilitated entry of aminoglycoside drugs into the cytoplasm
Increasing evidence suggests that aminoglycosides may mimic the effects of polyamines on NMDA receptors (Puel, 1995). Aminoglycosides play a key role in ototoxicity by activating polyamine-like NMDARs. More importantly, overactivation of NMDARs produces NO, which induces oxidative stress on hair cells. Therefore, it has been suggested that NMDA receptors antagonists may prevent aminoglycoside-induced ototoxicity. Memantine is an NMDA receptors antagonist that reduces aminoglycoside induced hearing loss
First line drug for serious MRSA infections such as bacteremia, endocarditis and pneumonia?
a) Vancomycin
b) Daptomycin
c) Ceftriaxone
d) Nafcillin
Vancmycin is the first line drug for serious MRSA infections such as bacteremia, endocarditis and pneumonia
Persistent MRSA bacteremia
High-dose daptomycin (10 mg per kg per day), if the isolate is susceptible, in combination with another agent (e.g., gentamicin, rifampin, linezolid, TMP/SMX, a beta-lactam antibiotic) should be considered. If reduced susceptibility to vancomycin and daptomycin is present, alternative treatment options include dalfopristin/quinupristin (Synercid; 7.5 mg per kg intravenously every eight hours), TMP/SMX, linezolid, or telavancin. These may be given as a single agent or in combination with other antibiotics.
What is Zebraxa?
Ceftolazone/tazobactam
5th gen cephalosporin used in combination with a beta lactamase inhibitor
FDA recommended indications
• Complicated Intra-abdominal Infections, used in combination with metronidazole
• Complicated Urinary Tract Infections, including Pyelonephritis (1.2)
Which of the following beta lactam is not an anti pseudomonal drug?
a) Piperacillin
b) Ticarcillin
c) Aztreonam
d) Dicloxacillin
- Piperacillin and Ticarcillin are extended-spectrum penicillins with activity against Pseudomonas aeruginosa.
- Aztreonam is a monobactam that also has activity against Pseudomonas.
- Dicloxacillin, however, is a narrow-spectrum penicillin used primarily for Staphylococcus aureus (especially MSSA) and has no activity against Pseudomonas.
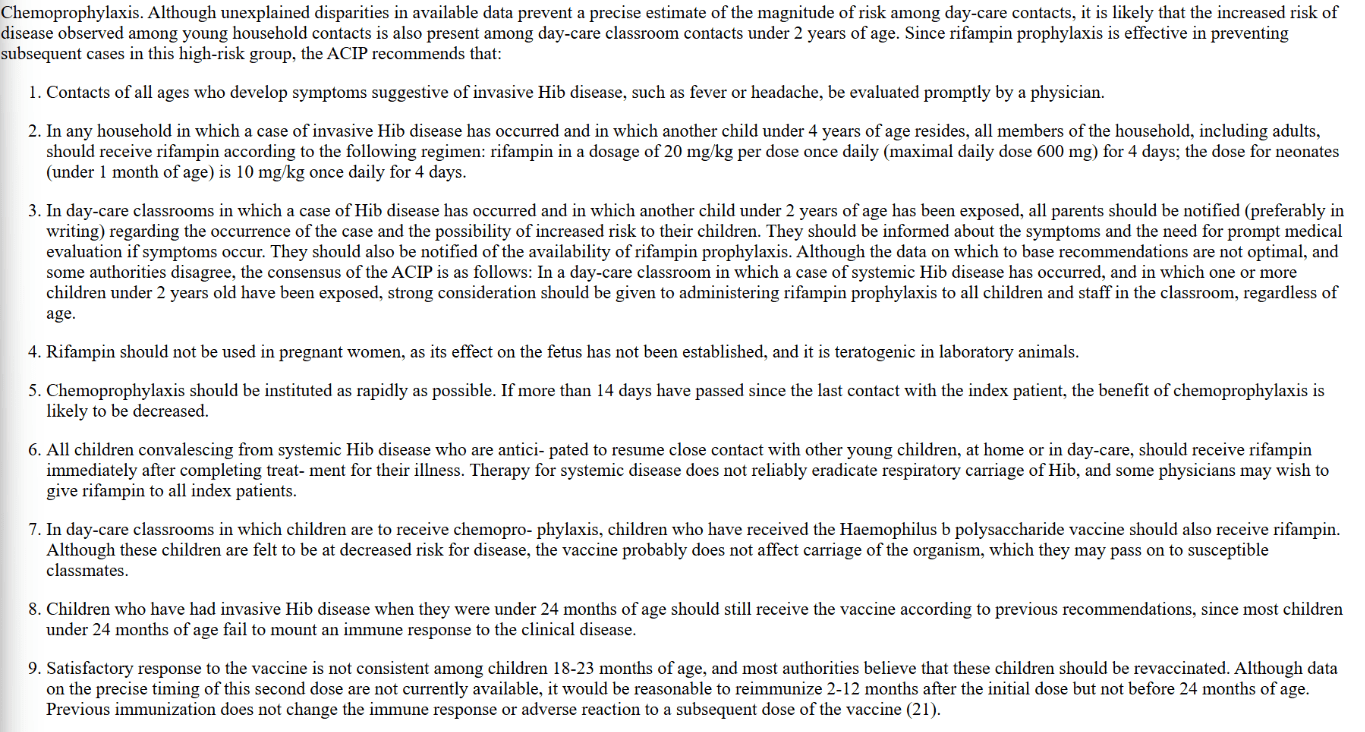
Which of the following drugs is used as chemoprophylaxis for patients exposed to Hemophilus influenza b?
a) Isoniazid
b) Rifampin
c) Pyrazinamide
d) Dapsone
Rifampin
In patients given which of the following antibiotics do we see commonly see an anaphylactoid reaction with diffuse flushing of skin?
a) Gentamicin
b) Tobramycin
c) Daptomycin
d) Vancomycin
Vancomycin flushing reaction (also known as red man syndrome): an anaphylactoid reaction caused by rapid infusion of vancomycin
- Nonspecific mast cell degranulation → rapid release of histamine
- Symptoms
- Diffuse flushing of the skin, pruritus mainly of the upper body
- Muscle spasms and pain in the back and chest
- Possible hypotension and dyspnea
- Can be prevented by slowing the rate of infusion and pretreating with antihistamines
This class of antibiotics is preferred for treating infections caused by ESBL-producing enterobacteria, such as E. coli and Klebsiella.
a) Fifth generation cephalosporins
b) Carbapenem
c) Monobactam
d) Vancomycin
- Examples
- IV imipenem (combined with cilastatin)
- IV meropenem
- IV ertapenem
- IV doripenem
- Special characteristics
- Imipenem is always given with cilastatin, which inhibits human dehydropeptidase I (a renal tubular enzyme that breaks down imipenem).
- Meropenem is stable to dehydropeptidase I.
- Broad-spectrum antibiotics with intrinsic beta-lactamase resistance
- Gram-positive cocci (except for MRSA and Enterococcus faecalis and Enterococcus faecium, which are intrinsically resistant)
- Gram-negative rods, including Pseudomonas aeruginosa (except ertapenem which has limited activity against Pseudomonas)
- Anaerobes
What is Zevtera?
Zevtera is the brand name for ceftobiprole medocaril (pro drug) converted to active version.
ZEVTERA is a cephalosporin antibacterial indicated for the treatment of:
Adult patients with Staphylococcus aureus bloodstream infections (bacteremia) (SAB), including those with right-sided infective endocarditis (
Adult patients with acute bacterial skin and skin structure infections (ABSSSI) and
Adult and pediatric patients (3 months to less than 18 years old) with community-acquired bacterial pneumonia (CABP)
How are beta lactams eliminated, and give an example of a beta lactam which is an exception to the rule
a) Hepatic, Cefdinir
b) Renal, Nafcillin
c) Biliary, Ticarcillin
d) Hepatic, Ceftaroline
Beta lactams are primarily excreted renally (via tubular secretion)
Exceptions:
Primary biliary: Nafcillin
Both renal and biliary: anti staph penicillins (eg, oxacillin, diclox) and ceftriaxone
Which of the following anti tubercular drugs is contraindicated in patients with optic neuritis?
a) Rifamycin
b) Isoniazid
c) Pyrazinamide
d) Ethambutol
d) Ethambutol
Ethambutol can directly injure the optic nerve, a condition known as ethambutol induced optic neuropathy--> decreased visual acuity, color vision problems, visual field defects and irreversible blindness
Which one of the following drug classes can cause acute intrahepatic cholestasis?
a) Macrolides
b) Cephalosporins
c) Aminoglycosides
d) Glycopeptides
Macrolides such as Erythromycin, Azithromycin are excreted through the biliary route and can cause intrahepatic cholestasis.
Adverse effects
- Increased intestinal motility → GI upset
- QT-interval prolongation , arrhythmia
- Acute cholestatic hepatitis
- Rash
- Increased risk of hypertrophic pyloric stenosis (erythromycin and azithromycin) in infants up to 6 weeks of age
Which of the following is one of the two drugs that can be is traditionally used in the empiric management of patients with Vancomycin resistant Enterococcus?
Bonus 1000 points for novel agent used to treat VRE
a) Daptomycin
b) Nitrofurantoin
c) Clindamycin
d) Kanamycin
Answer: Daptomycin
Drugs of choice in patients with VRE are Linezolid> Daptomycin
The streptogramins are macromolecular antibiotics produced by Streptomyces pristinaepiralis.They belong to the macrolide-lincosamide-streptogramin group of antibiotics. Quinupristin-dalfopristin is made up of chemically modified, water-soluble, injectable derivatives of type B streptogramin (quinupristin) and type A streptogramin (dalfopristin) in a 30:70 ratio, can also be used to treat VRE
What is Blujepa?
BLUJEPA (Gepotidacin) is a triazaacenaphthylene bacterial type II topoisomerase inhibitor indicated for the treatment of female adult and pediatric patients 12 years of age and older weighing at least 40 kilograms (kg) with uncomplicated urinary tract infections (uUTI) caused by the following susceptible microorganisms: Escherichia coli, Klebsiella pneumoniae, Citrobacter freundii complex, Staphylococcus saprophyticus, and Enterococcus faecalis.
Like a fluoroquinolone but not a fluoroquinolone. First in class
What is the rationale for always giving imipenem with cilastatin?
Imipenem is always given with cilastatin which inhibits human dihydropeptidase I prolonging the half life of Imipenem
Get a kill that is lasting with Imipenem plus Cilastatin
Which of the following anti mycobacterial drugs can be used in the management of dermatitis herpetiformis?
a) Dapsone
b) Ethambutol
c) Rifapentine
d) Rifaximin
Dapsone - competitive antagonist of para mino benzoic acid for dihydropteroate synthetase --> inhibition of dihydrofolic acid synthesis. Essentially interferes with folate synthesis which is an essential component needed for bacterial DNA replication.
Dapsone also has an anti inflammatory role - inhibits neutrophil activity by inhibiting MPO which prevents production of ROS
Interferes with neutrophil adherence. This is how dapsone is effective in suppressing the immune system and producing a favourable effect in patients with dermatitis herpetiformis.
DH is an intensely pruritic chronic blistering auto immune skin disease caused by a reaction to gluten.
Which of the following tetracyclines is not contraindicated in patients with renal failure?
a) Minocycline
b) Tetracycline
c) Doxycycline
d) Demeclocycline
Doxycycline is the only tetracycline that is not contraindicated in patients with renal failure. It is eliminated extrarenally through the GI tract. It does not require dose adjustment in patients with renal failure.
This aminoglycoside is used can be used as second line agent for the treatment of M.tuberculosis and M. avium-intracellulare
Streptomycin is used as a second-line treatment for Mycobacterium tuberculosis and M. avium-intracellulare
What is Emblaveo?
EMBLAVEO is a combination of aztreonam, a monobactam antibacterial, and avibactam, a beta-lactamase inhibitor, that when used in combination with metronidazole, is indicated in patients 18 years and older who have limited or no alternative options for the treatment of complicated intra-abdominal infections (cIAI) including those caused by the following susceptible gram-negative microorganisms: Escherichia coli, Klebsiella pneumoniae, Klebsiella oxytoca, Enterobacter cloacae complex, Citrobacter freundii complex, and Serratia marcescens.
Which of the following statements about beta lactams is true?
a) Monobactams are highly effective against gram negative bacteria only
b) 4th generation cephalosporins are least active against gram positive bacteria
c) Only 4 th generation cephalosporins work effectively against Enterococcus
d) Cefotetan is an example of a fifth generation cephalosporin
a) Monobactams (Aztreonam) are highly effective against gram negative bacteria only and they usually need to be used in combination with other agents
b) Third generation cephalosporins have the least activity against gram negative bacteria. First, 4th and fifth generation cephalosporins are highly effective
c) Only 5th generation cephalosporins work effectively Enterococcus
d) Ceftaroline is an example of a 5th gen cephalosporin, Cefotetan is a 3rd gen cephalosporin
Which of the following drugs is preferred for the treatment of mycobacterial infections in patients with HIV?
a) Rifampin
b) Rifabutin
c) Rifaximin
d) Rifapentine
b) Rifabutin
All these drugs are examples of Rifamycins
Mechanism of action: inhibit bacterial DNA dependent RNA polymerase--> prevention of mRNA synthesis--> inhibition of bacterial protein synthesis--> cell death
Route of elimination: bilary
Rifabutin is preferred for the treatment of mycobacterial infections in patients with HIV because it has a lower potential for CYP induction than rifampin. Rifampin's strong CYP inducing effect causes significant drug- drug interaction that can render many ART medications ineffective
Which of the following groups of antibiotics can rarely precipitate pseudotumor cerebri?
a) Aminoglycosides
b) Glycopeptides
c) Tetracyclines
d) Polymyxin B
Tetracyclines can rarely cause pseudotumor cerebri
- Mechanism of action: bind 30S subunit → aminoacyl-tRNA is blocked from binding to ribosome acceptor site → inhibition of bacterial protein synthesis (bacteriostatic effect)
- Examples
- Oral or IV minocycline
- Oral or IV tetracycline
- Oral doxycycline
- Oral demeclocycline
Idiopathic intracranial hypertension, or pseudotumor cerebri, is a syndrome of increased intracranial pressure without a space-occupying lesion. Can be seen in 4-5% of patients prescribed Tetracyclines
What is a CRAB infection?
Acinetobacter is a gram-negative coccobacillus. The organism has the ability to accumulate diverse mechanisms of resistance, leading to the emergence of strains that are resistant to all commercially available antibiotics.
Acinetobacter baumannii is one of the ESCAPE organisms, a group of clinically important, predominantly health care-associated organisms that have the potential for substantial antimicrobial resistance. Other ESCAPE organisms are Enterococcus faecium, Staphylococcus aureus, Clostridioides difficile, Pseudomonas aeruginosa, and Enterobacteriaceae.
Carbapenem is an antibiotic of choice in patients with Acinetobacter baumannii --> they now produce carbapenemases
- Sulbactam-durlobactam, in combination with meropenem or imipenem-cilastatin, was added as the preferred agent for the treatment of CRAB infections.
- High-dose ampicillin-sulbactam in combination with at least one other agent has been changed from a preferred to an alternative regimen if sulbactam-durlobactam is not available. (IDSA 2024)
What is Orlynvah?
ORLYNVAH a combination of sulopenem etzadroxil, a penem antibacterial, and probenecid, a renal tubular transport inhibitor, is indicated for the treatment of uncomplicated urinary tract infections (uUTI) caused by the designated microorganisms Escherichia coli, Klebsiella pneumoniae, or Proteus mirabilis in adult women who have limited or no alternative oral antibacterial treatment options
PIVYA is a penicillin class antibacterial indicated for the treatment of female patients 18 years of age and older with uncomplicated urinary tract infections (uUTI) caused by susceptible isolates of Escherichia coli, Proteus mirabilis and Staphylococcus saprophyticus.