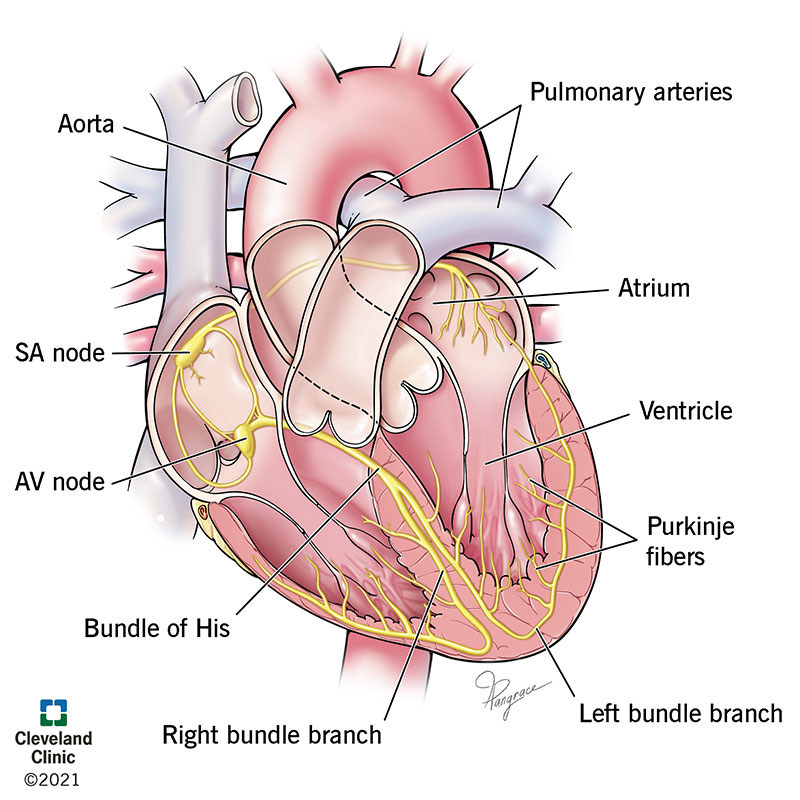
Primary Pacemakers in the heart
SA node
AV node
Movement towards an EKG lead causes this to happen on the EKG paper.
Positive deflection. 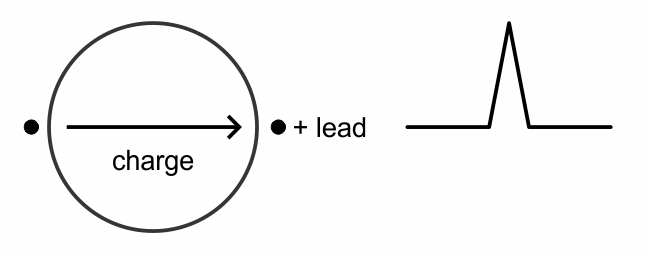
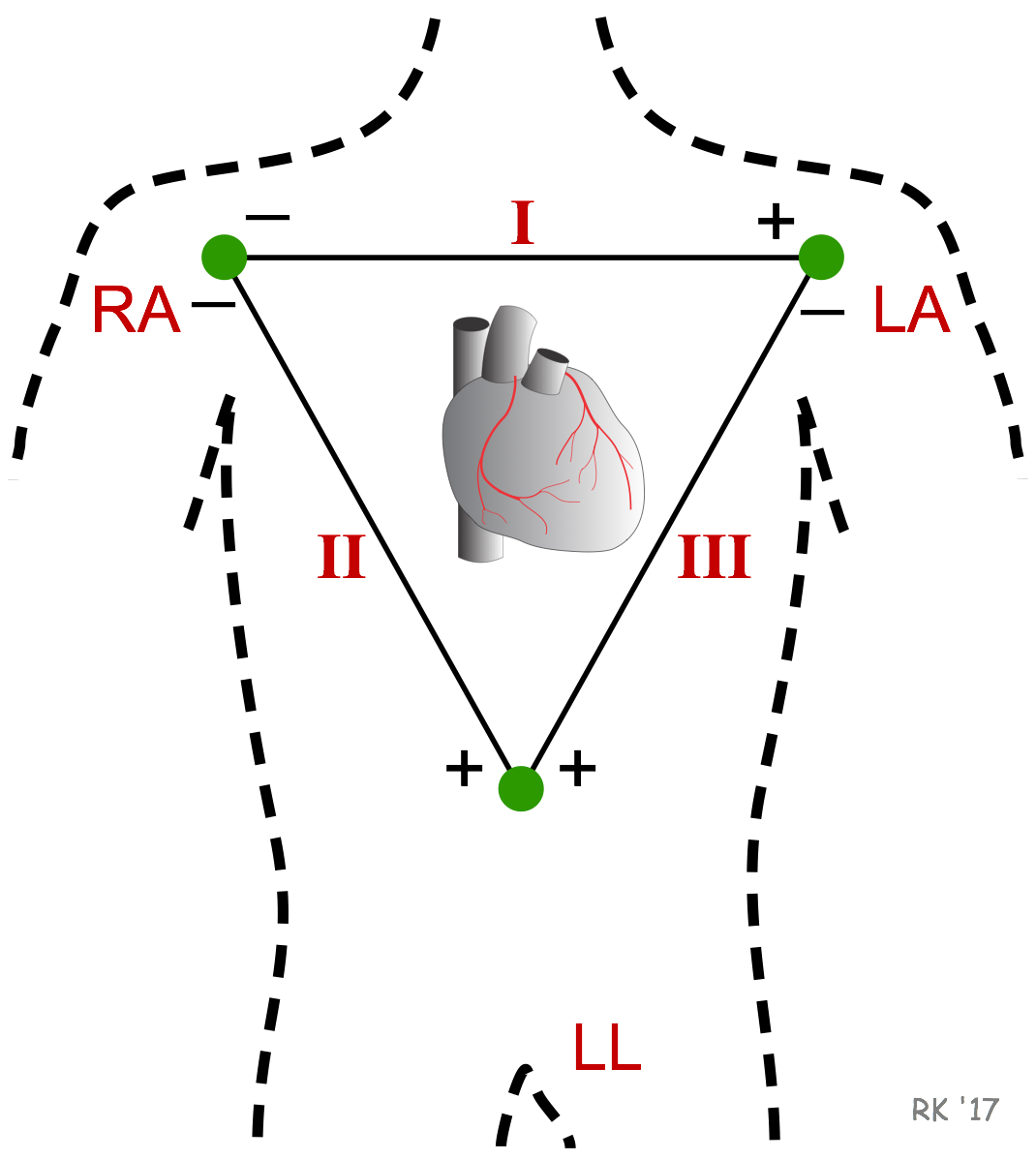
The standard limb leads (I,II,III) Look at what?
Lead I: Left high lateral wall
Lead II: Inferior wall
Lead III: Inferior wall
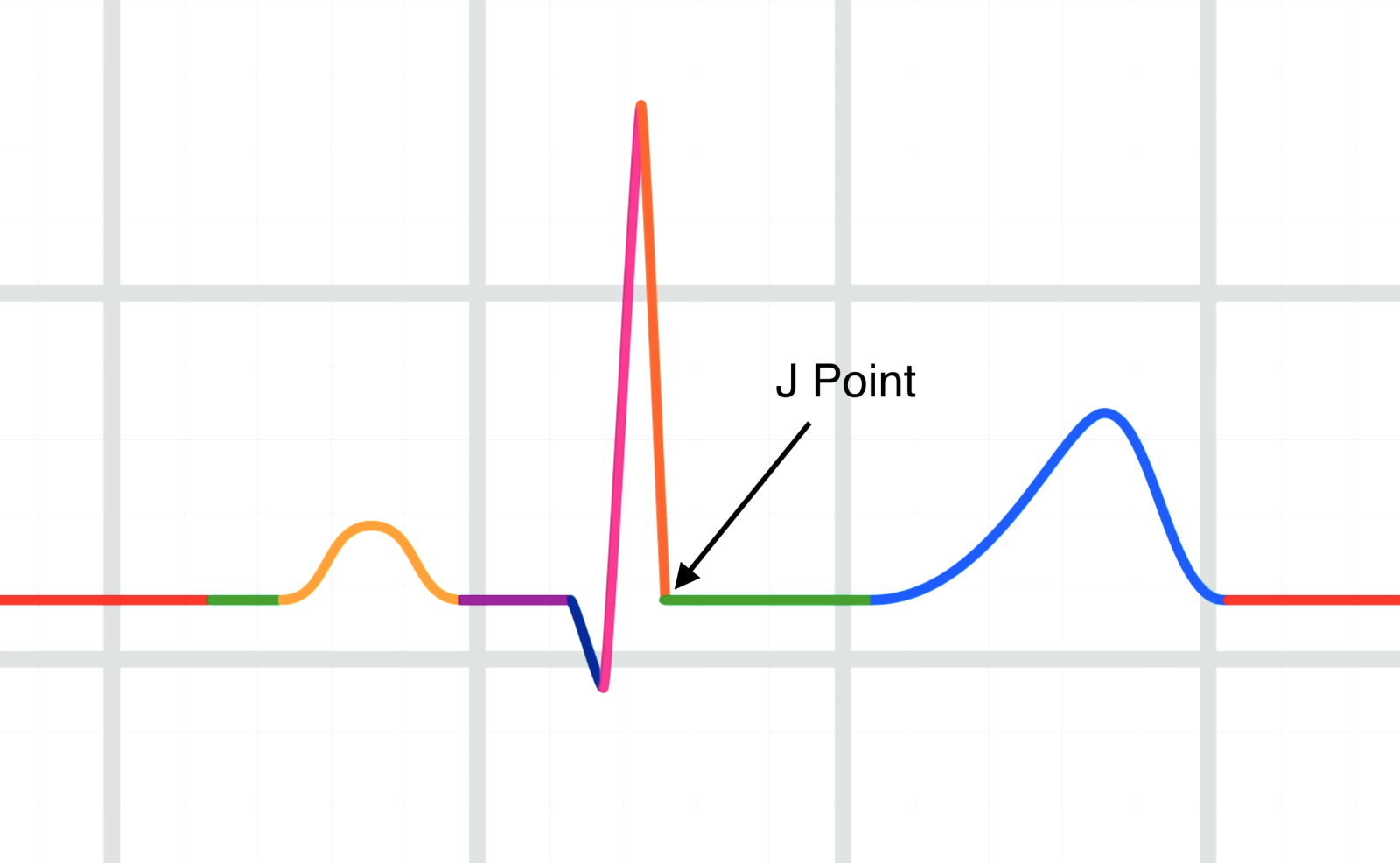
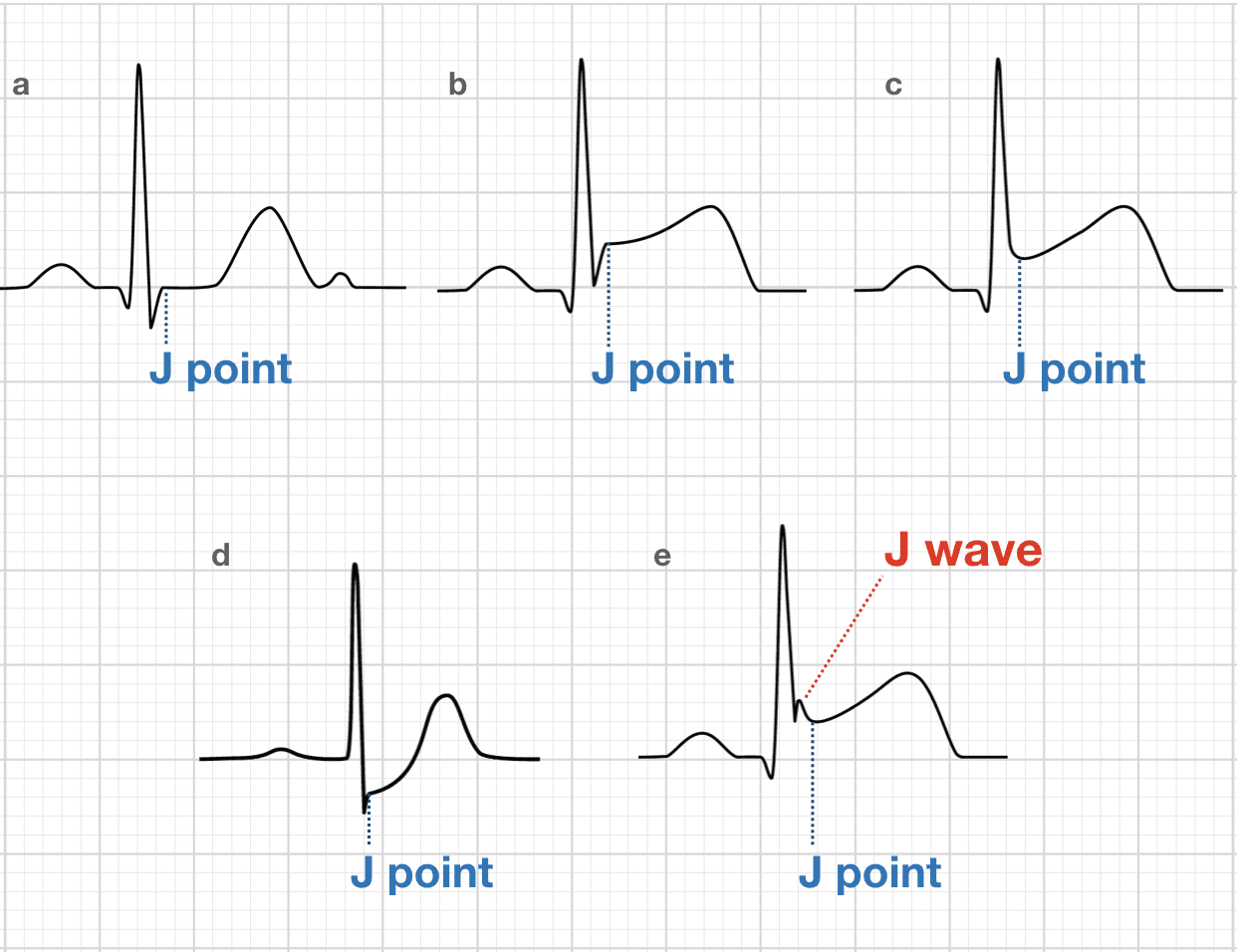
This is the junction between the termination of the ARS complex and the beginning of the ST segment.
J-Point.
Heart failure results from ANY disorder that causes.
1.____________
AND / OR
2.____________
1. Reduces myocardial contractility (Can't pump)(Systolic dysfunciton)
Normal EF = 55-70%
Systole = Emptying
Diastole = Filling
2. Reduces ventricular filling (Diastolic dysfunction) (Can't Fill)

These are primary cardiac electrolytes / ions inside and outside of cardiac cells used to develop electricity.
Sodium Na+
Potassium K+
Calcium Ca++
This portion of the EKG represents atrial depolarization.
P Wave
The augmented limb leads (aVR, aVL, aVF), look at what?
aVR: Right high lateral wall
aVL: Left high lateral wall
aVF: Inferior wall

We evaluate the J-point and ST segment for these things.
Elevation (MI)
Depression (Ischemia)
Notching and J-waves (BER and Hypothermia).
This definition is the mechanical function of the heart.
The amount of blood pumped out during systole.
Stroke Volume.
Must have normal heart structure and adequate filling of the cardiac chambers.
This is defined as the movement of sodium ions across the cell membrane, changing the electrical potential of the cell to positive, leading to cardiac contraction.
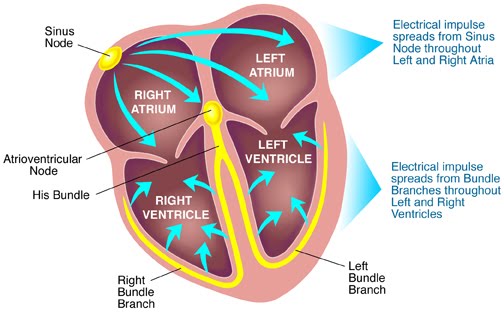
Depolarization. Conduction cycle phase "0"
This portion of the EKG represents electrical conduction through the AV Junction.
PR Interval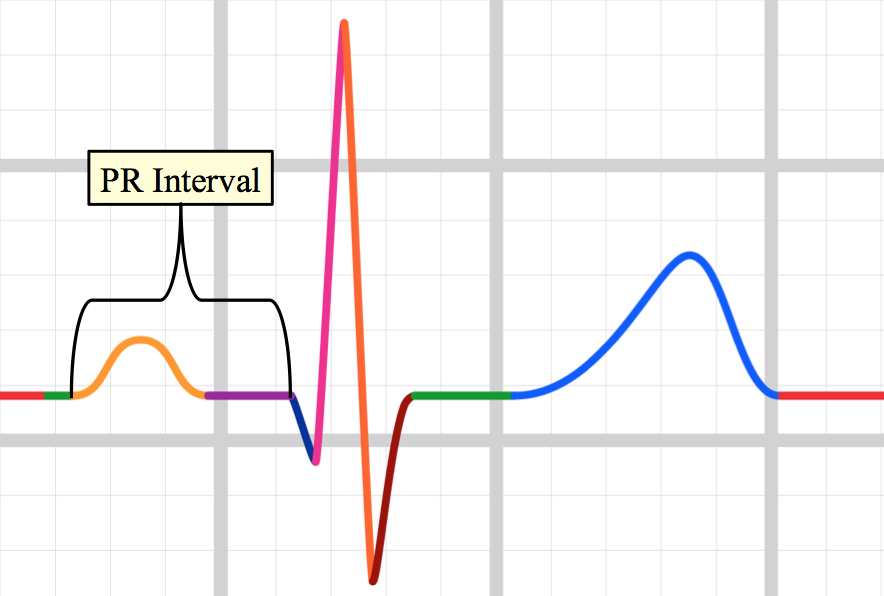
The precordial leads (V1-V6) look at what?
V1-V2: Septum
V3-V4: Anterior wall
V5-V6: Lateral wall

Infarction / Ischemia causes depolarization and repolarization changes in the dead/dying tissues, causing WHAT 3 EKG changes?
ST segment changes
T Wave changes
Pathologic Q waves

This is the pressure that the ventricles must contract against to eject blood.
This is the amount of blood stretching the myocardial cells just prior to contraction
Afterload
Preload

This is defined as the movement of ions until the cardiac cell is more NEGATIVE, and at its resting negative potential (Ready for another cardiac contraction)
Repolarization
This portion of the EKG represents ventricular depolarization.
QRS Complex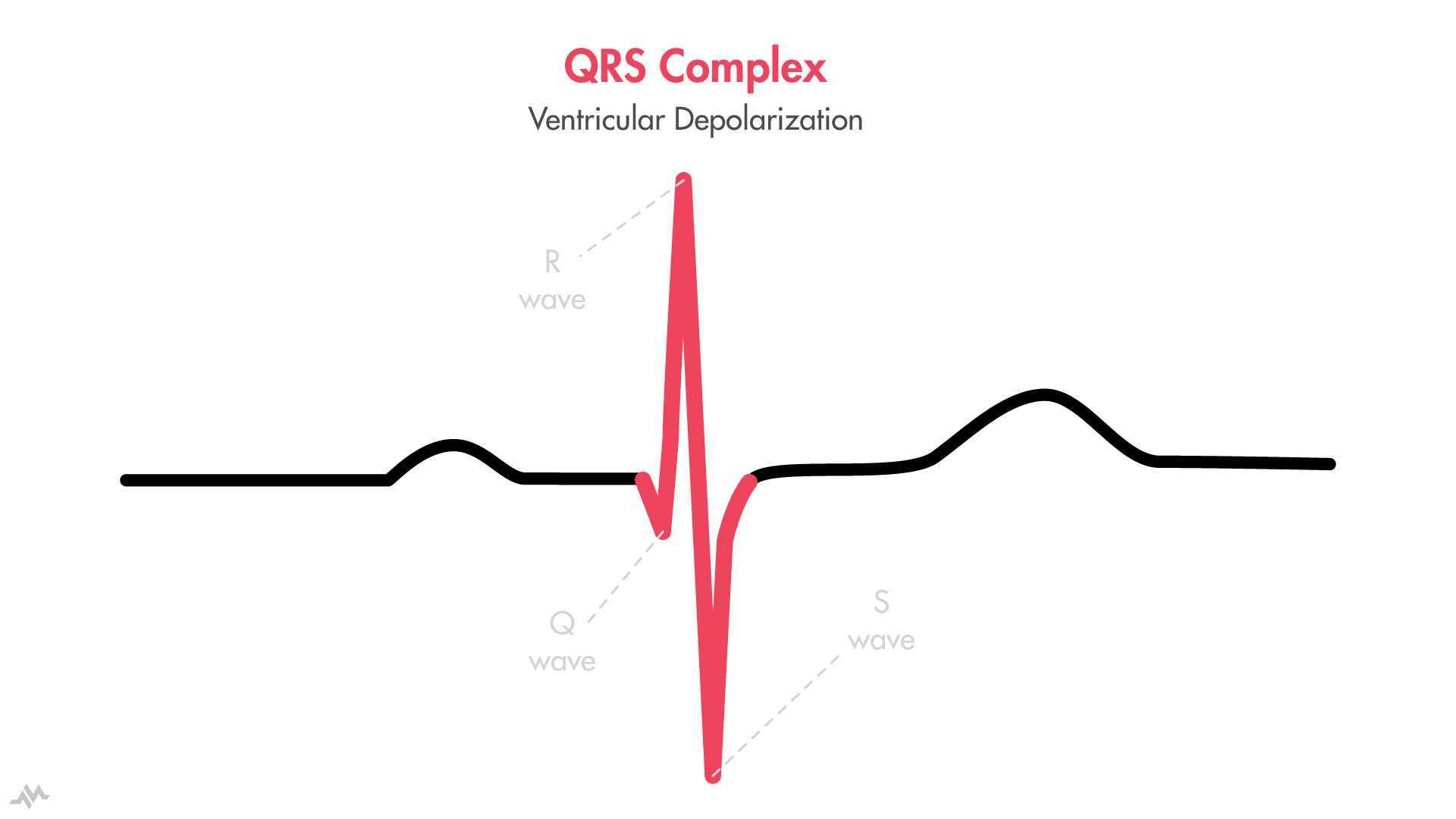
These EKG leads look at the right side of the heart
V1, V2, V3
aVR Right high lateral
(Not a view of the right ventrical.
When measuring for ST segment elevation / depression, "what" do we base our measurement off of?
T-P Segment.
Time between the end of the T wave and prior to the P wave.
Systemic Vascular Resistance (SVR)(force that the body's vasculature exerts on circulating blood) CAUSES hypertention.
What ventricle is effected by Hypertension?
What happens to afterload with increased SVR?
Left ventricle is affected.
Afterload is Increased.

The cardiac conduction system is comprised of these five areas.
SA Node, AV Node, Bundle of HIS, Bundle Branches, Purkinje Fibers.
This EKG portion is the time BETWEEN ventricular depolarization and repolarization.
ST Segment
These ekg leads look at the inferior side of the heart
II
III
aVF
if "this" shape is present in ST elevation, it is more likely that the patient is truly having an MI.
Convex shape. 
increased "Pulmonary vascular resistance" (Left ventricular failure, Chronic hypoxia, PE).
What ventricle is affected?
What happens to afterload?
Right ventricle
Increased afterload.
Systole:max_bytes(150000):strip_icc()/cardiac_cycle-597a5d8168e1a200115e5937.jpg)
This portion of the EKG represents ventricular repolarization
T Wave
These leads look at the left side of the heart.
V5
V6
I
aVL
These types of T-waves are broad and asymmetrically large.
And indicative of early MI, prior to ST elevation & Q waves
Hyperacute T waves
Increased afterload causes heart muscle to?
Causing?
Work harder to overcome the constricted vasculature.
Become hypertrophied or Dilated.
Hypertrohied = Threw a bunch of springs on top of a trampoline and it didn't increase the bounciness.
Dilated = The springs are all stretched out and aren't as bouncy anymore.

This portion of the EKG is the total time for ventricular Depolarization AND repolarization
QT interval
These leads look at the posterior of the heart
Opposite of V1-V2
ST Elevation MI Evolution.
EKG Findings for answer
1. Before Injury
2. Ischemia
3. Infarction
4. Fibrosis
1. Normal EKG / Baseline
2. ST Depression, Hyperacute T waves, T wave inversions
3. ST elevation, Q waves appear
4. ST segment returnes to baseline, Q Waves persist.