During wound preparation, chlorhexidine and alcohol should never be used. State the rationale as to why these agents should be avoided.
State which agents are appropriate for wound preparation.
Harsh antiseptics (e.g., chlorhexidine, alcohol) are cytotoxic and delay healing.
Dilute Betadine and sterile saline safely cleanse without damaging viable cells.
10 year old Pony mare presenting for acute onset left forelimb lameness (AAEP grade 4/5). Blocks out to PD nerve block.
What are your top differential diagnosis?
Subsolar abscess
P3 fracture
Owners of colicking horses are often distressed and will ask what they can do before you arrive to examine the horse.
Outline what advice you would give an owner over the phone
Withhold feed, be careful of own safety- if the horse is violently colicky do not try to walk the horse or keep it from rolling
If it is safe to do so, the owner may walk the horse gently on a safe soft surface away from fences
Do not administer any medications or home remedies
Define posterior synechiae and what does it commonly signify?
Definition - when a segment of iris adheres to the lens
This indicates there is inflammation (uveitis)
You are called out to evaluate a wound near the lateral aspect of the carpus. Given the anatomical location you are concerned about possible synovial communication.
What diagnostic steps should be taken to confirm synovial involvement?
Arthrocentesis for cytology and total protein (TP)
Pressurization of the joint with sterile saline
Describe the anatomical location to perform a PD nerve block
Just proximal to the heel bulbs, at the level of the collateral cartilages.
Axial to the medial and lateral neurovascular bundle.
You perform an abdominocentesis.
The total protein (TP) concentration in the peritoneal fluid obtained is 48g/L.
What is the normal range and what is your interpretation of the results?
Normal peritoneal fluid TP concentration is generally < 25 g/L.
In this case 48g/L indicates a significant increase.
In general, an increase in peritoneal fluid TP concentration can be due to several possible causes involving inflammation of structures within the abdomen (infectious or non-infectious) leading to protein leakage from blood vessels into the abdominal cavity (high protein transudate).
You see a horse with a cough and mucopurulent nasal discharge.
What diagnostics should you perform?
Transtracheal wash (TTW) for culture
Upper airway endoscopy
You obtain synovial fluid from a horse with a puncture wound near the fetlock. The sample is turbid and orange.
Cytology reveals:
- 20 × 10⁹/L TNCC
- 89% neutrophils.
What is your interpretation?
Synovial sepsis
15 year old Warmblood mare, showjumper. Bilateral hindlimb lameness (mild AAEP 2/5). No abnormalities on palpation. Flexes positive to the R and L hind proximal limb. No response to digital pressure of the proximal suspensory ligaments bilaterally.
Did not block out with low 4 point nerve block.
What is your next step in the lameness workup? Justify your answer based on your primary differential diagnosis.
Intra-articular local anesthesia of the tarsus
Primary differential diagnosis is osteoarthritis, which commonly occurs in the tarsus. Diagnosis is best radiographically, but need to localize lameness to this region prior to obtaining radiographs.
 What are your differential diagnosis based on this ultrasound
What are your differential diagnosis based on this ultrasound
Small intestinal causes of colic
- Strangulating lipoma
- Small intestinal volvulus
- Epiploic foramen entrapment
- Gastrosplenic entrapment
- Proximal enteritis
You go to see a horse with acute respiratory distress.
Does the horse need a tracheostomy? What portions of your clinical examination will help you decide whether this is indicated or not
Tracheotomy will only be useful if it is an upper airway obstructive issue.
On PE rule out lower respiratory causes with your thoracic and tracheal auscultation.
Upper airway endoscopy is also very useful for the definitive diagnosis of the cause of the upper airway obstruction.
A wound over the body has a large pocket of dead space that cannot be closed with sutures.
Name two appropriate techniques to manage the dead space
Drain placement: allows fluid egress but can serve as a bacterial conduit if left in for >3 days.
Pressure bandage: eliminates space without foreign body but may impair perfusion if applied too tightly.
Describe the anatomical locations to perform a Low 4 point nerve block
What nerves are being desensitized at each location?
For medial and lateral palmar/plantar metacarpal/metatarsal nerve:
- Below the distal end of the MC/MTII and MC/MTIV (i.e. the "button of the splint bone")
For medial and lateral palmar/plantar nerve:
- Between suspensory ligament and the deep digital flexor tendon, injection site will be about 2cm proximal to the buttons of the splint bones.
You get called out to see a horse with colic. On your physical examination you note the horse is tachycardic (HR 80 bpm) and absent borborygmi
What should your immediate next step in the workup be and why?
Pass a nasogastric tube!
Tachycardia can occur secondary to gastric distention. Pass NGT to decompress stomach first, to prevent potential gastric rupture.
Name the joints of the tarsus
Tarsocrural joint (or tibiotarsal joint)
Talocalcaneal joint
Proximal intertarsal joint
Distal intertarsal joint
Tarsometatarsal joint
A 6-year-old gelding has a wound over the distal cannon bone that remains unhealed three weeks after the initial injury. The wound continues to drain purulent material.
Radiographs reveal a small fragment of cortical bone surrounded by a radiolucent rim and an area of sclerosis in the adjacent bone.
What is the most likely diagnosis?
Briefly explain the pathophysiology of this condition and why it delays wound healing.
Outline the recommended treatment approach.
Diagnosis: Sequestrum formation
Pathophysiology: Loss of periosteal blood supply → necrosis of cortical bone fragment → fragment becomes a sequestrum, which acts as a foreign body harboring bacteria → persistent inflammation and drainage, thus preventing wound granulation and epithelialization.
Treatment: Surgical removal of the sequestrum (sequestrectomy), debridement of necrotic tissue.
What are the common locations of OCD lesions in the horse?
Tarsus: Distal intermediate ridge of the tibia, Lateral trochlear ridge of the talus, Medial malleolus
Stifle: Lateral trochlear ridge of the femur, Medial trochlear ridge of the femur, patella
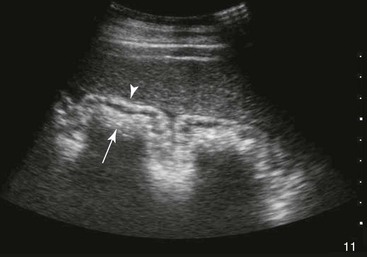
You assess a patient with acute, severe colic. On ultrasound you note the following abnormality.
Make a list of differential diagnosis for this abnormality.
How would you determine if this patient can be managed medically or requires surgery?
DDX: large colon volulus, large colon displacement, colitis
Abdominocentesis (assess peritoneal vs peripheral lactate)
Name which cranial nerves course through the medial compartment of the guttural pouch
CN 9, 10, 11, 12