A 6 month old girl, known to have large ventricular septal defect initially gained weight appropriately, however, 2 months ago began to gain weight poorly, and in the last 2 weeks is loosing weight. The child is on digoxin, lasix and captopril. The cause of weight loss in this child could be attributed to:
A. Decrease caloric consumption and increase expenditure.
B. Interference of medications with absorption.
C. Presence of at least moderate pulmonary stenosis with ventricular septal defect.
D. Elevated pulmonary vascular resistance.
Children with large ventricular septal defects develop large left to right shunting and increased pulmonary blood flow. This will result in pulmonary edema, producing difficulty in breathing effort (tachypnea and respiratory distress). The left to right shunting at the septal defect causes volume overload of the right ventricle and the increase in pulmonary blood flow will cause the pulmonary venous return to increase thus overloading the left heart as well. This increase in cardiac load will cause myocardial fatigue.
The increase in work load of the myocardium and respiratory system consumes a significant portion of caloric intake, which together with reduced caloric intake due to respiratory distress and inability to feed properly will lead to failure to thrive.
Option B is incorrect since these medications do not interfere with intestinal absorption.
Option C is incorrect since pulmonary stenosis would actually restrict pulmonary blood flow resulting in less and not more congestive heart failure.
Option D is incorrect, since elevation in pulmonary vascular resistance, though carries worse prognosis, actually causes less pulmonary blood flow and consequently less congestive heart failure.
A one week old is seen at well child care. Mom is concerned that the baby is not feeding well. He takes one half to one ounce every 1-2 hours, thereafter he falls asleep. HR 70 bpm, RR is 45/min; Examination reveals no cyanosis or jaundice. A wide spread rash is noted over the face and trunk. Capillary refill is 3 seconds. Femoral and brachial arterial pulses are equal and full. Liver edge is palpated at 4-5 cm below right costal margin. Lungs are clear to auscultation, S1 is normal; S2 splits with no systolic or diastolic murmurs.
Important question to ask mother is:
A. Type of formula used for feeding.
B. History of attempted nursing of this child or previous children.
C. History of maternal ailment during gestation. .
D. History of congenital heart disease
This child has a heart rate of 75 bpm, which is slow for this age. This may be a manifestation of fetal affliction by maternal systemic lupus erythematosus. Electrocardiography will most probably show complete atrioventricular block. The poor feeding, hepatomegaly and delayed capillary refill (normal less than 2 seconds) are all features of poor cardiac output and heart failure secondary to bradycardia. The rash is another manifestation of systemic lupus erythematosus. Other cardiac complications of maternal lupus include cardiomyopathy and l-transposition of the great vessels, also known as ventricular inversion or corrected transposition.
Option A is incorrect since the type of formula is irrelevant when the problem is small volume of feeds. Babies may poorly tolerate certain formulas resulting in emesis or diarrhea.
Option B is incorrect since nursing is irrelevant in this case, particularly with clear symptoms of heart failure.
Option D is incorrect since auscultation does not appear to suggest congenital heart disease, but instead the problem seems to stem from a slow heart rate.
A 13 year old girl weighs 35 kg and is 178 cm tall. She is asymptomatic and is seen for assessment of a heart murmur detected by school nurse. Heart rate is 80 bpm, respiratory rate is 20/min. BP in right arm is 110/70. Mucosa is pink, capillary refill is brisk. Femoral and arterial pulses are equal and full. No hepatomegaly is detected. Precordium is with no palpable thrill. On auscultation, first heart sound is normal, second heart sound splits and varies with respiration. There is a 3/6 holosystolic murmur at apex. System review shows significant myopia. Family history is not significant.
In addition to mitral regurgitation, what else would you expect the echocardiogram to demonstrate?
A. Mitral valve prolapse and ventricular septal defect.
B. Mitral valve prolapse and aortic root dilation.
C. Aortic stenosis.
D. Tricuspid valve regurgitation.
This child appears to have Marfan syndrome, an autosomal dominant disease which may present as a spontaneous mutation with negative family history. This child is tall (above 95 percentile) with myopia and a murmur consistent with mitral regurgitation. Patients with Marfan syndrome are tall, with long arm length span and ocular abnormalities such as myopia and retinal detachment. The cardiac pathologies, which are secondary to collagen disorder, present as mitral valve prolapse, mitral regurgitation, aortic root dilation and aortic regurgitation. Patients with Marfan syndrome may develop significant aortic root dilation, leading to aneurysm and aortic root rupture with catastrophic consequences.
Option A is incorrect since the murmur is consistent with mitral regurgitation and not ventricular septal defect (VSD). VSD murmurs are heard best at the left lower sternal border.
Option C is incorrect since a murmur of aortic stenosis is heard as a harsh ejection systolic murmur at right upper sternal border. Patients with Marfan syndrome are not at risk to develop aortic stenosis.
Option D is incorrect since the murmur is not consistent with tricuspid valve regurgitation.
A 3 month old infant, born at 29 weeks gestation, in the neonatal intensive care unit continues to require ventilatory support due to severe and chronic lung disease attributed to prematurity. A recent short and harsh ejection systolic murmur is heard over the left mid-sternal border. Vital signs and physical examination is otherwise unchanged. Echocardiography demonstrates severe, bilateral ventricular hypertrophy with intracavitory obstruction to flow within the right and left ventricles.
The cardiac changes could be attributed to:
A. Use of bronchodilators in managing severe lung disease.
B. Use of steroids in managing lung disease secondary to prematurity.
C. Use of surfactant soon after delivery. Correct answer is B:
D. Cor pulmonale secondary to severe lung disease.
Steroids used chronically in premature infants in the treatment of chronic lung disease due to prematurity may cause hypertrophic cardiomyopathy. This resolves when steroid therapy is withdrawn. Hypertrophied muscles will cause reduction of ventricular cavity size leading to obstruction to blood flow.
Option A and C are incorrect since these are not known side effects to these medications.
Option D is incorrect since core pulmonale may cause right ventricular hypertrophy and right heart failure, however, the left heart will not be affected.
An 8 year old girl followed by a GI specialist for the past few years for irritable bowel disease. She was referred to a pediatric cardiologist for evaluation of a heart murmur. Heart rate 90 bpm, respiratory rate 20/minute, Oxygen saturation 95% while breathing room air, BP in right upper extremity 110/60 mmHg. Mucosa is pink, though pale. Capillary refill is brisk. Fingers show clubbing. No hepatomegaly is present, precordium is hyperactive with increase right and left ventricular impulse, no palpable thrill. The murmur is 2/6 systolic flow murmur heard over the left and right upper sternal borders. Lungs were clear to auscultation bilaterally. The cardiologist felt that the heart murmur is secondary to increase flow across aortic and pulmonary valves due to chronic anemia.
What is the most probable cause of clubbing of fingers in this patient?
A. Clubbing is most probably a result of bowel disease.
B. The child may have concomitant lung disease.
C. The child may have concomitant heart disease.
D. Clubbing is frequently seen in otherwise normal individuals.
Irritable bowl disease causes chronic anemia, which results in chronic hypoxia, which like cyanotic heart disease and chronic lung disease may lead to clubbing of fingers. This patient has no evidence of significant heart or lung disease. Idiopathic clubbing is possible, though rare.
Clubbing of fingers resulting from hypoxia which induces tissues to expand capillary beds to increase blood flow, this will result in thickening of peripheral tissues, such as fingers and toes.
A 4 year old child is referred to the emergency room for evaluation of abnormal heart rate. The child was seen in the pediatrician’s office for evaluation of emesis when a heart rate of 60 bpm was detected. The child has had a viral URI for few days but was thought to be getting better when emesis developed overnight. Past medical history is unremarkable; the child was receiving a decongestant-cold medication for the past 2 days. Family history is remarkable for a grandmother who resides with the child who suffers from congestive heart failure and history of tachyarrhythmia.
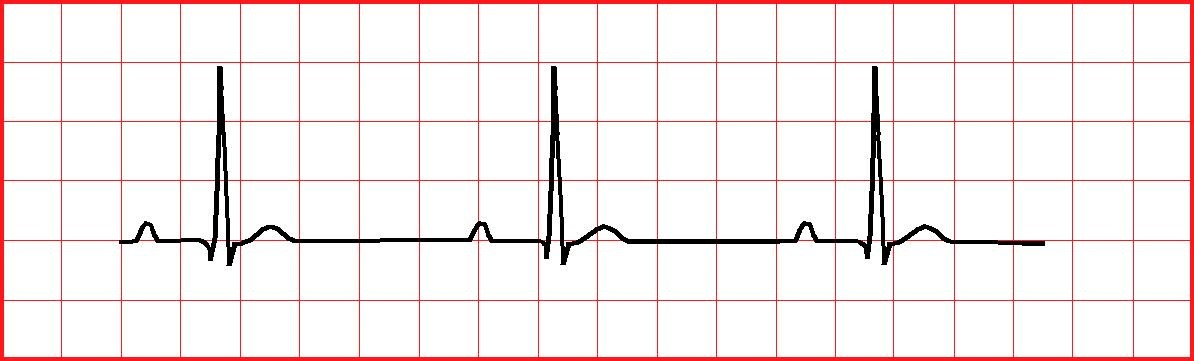
12 lead ECG and rhythm strip is shown below.

A. What are the ingredients of the cold medication?
B. Was rash, conjunctivitis or peeling of digits noted?
C. What medications is grandmother on?
D. How long did the fever persist?
This child has sinus bradycardia with first degree atrioventricular block (AVB). The cold symptoms do not appear to be related to bradycardia. Fever, due to a viral infection causes sinus tachycardia, not bradycardia. Cold medications with decongestants cause tachycardia as well. Congestive heart failure may be treated with digoxin which if ingested inadvertently by a toddler may cause bradycardia and first degree AVB. Management of a child with digoxin toxicity may include Digibind; this is used when the total ingested dose is > 4 mg in children or > 10 mg in adults. It is also used if there are significant ECG changes, such as ventricular arrhythmias. First degree AVB and mild sinus bradycardia could be observed. Hyperkalemia results from digoxin toxicity, not Hypokalemia. Emesis induction or activated charcoal is used when ingestion is less than 30 minutes ago.