What is the correct Expanse Name or Mnemonic for this Insurance card?
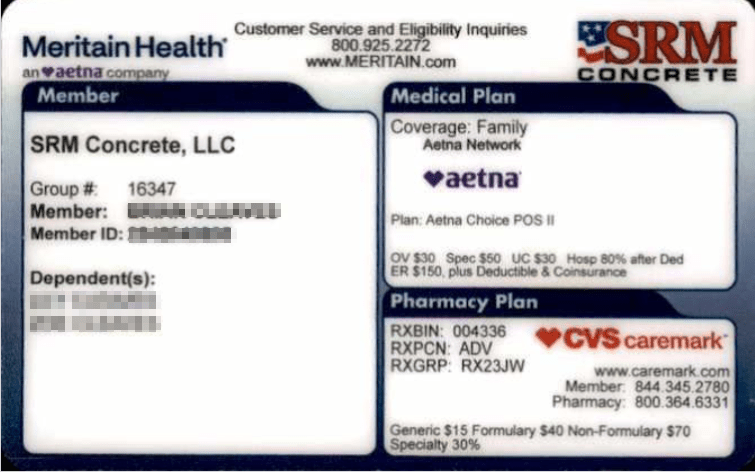
Meritain Health - MERITAIN
Identifiers: Meritain logo top left
What is the correct Expanse Name or Mnemonic for this Insurance card?
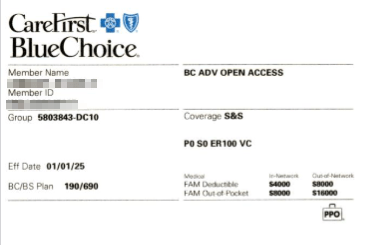
Carefirst BlueChoice - BCBLUCHOI
Identifiers: BlueChoice logo top left AND local plan # 190/690
What is the correct Expanse Name or Mnemonic for this Insurance card?
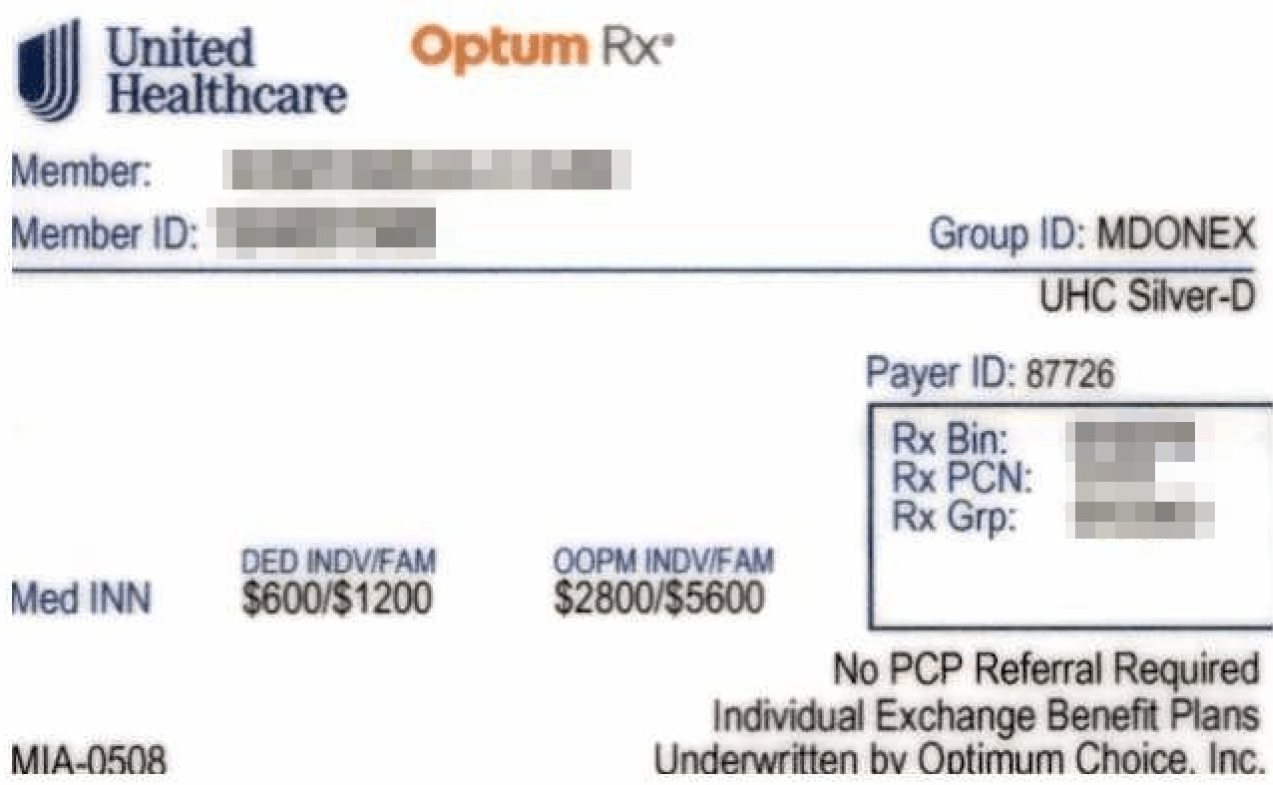
United Healthcare Select HMO
Identifiers: Individual Exchange - The exchange plans go under the UHC-HMO selection. Ignore the Optimum Choice identifier on the card.
What is the correct Expanse Name or Mnemonic for this Insurance card?
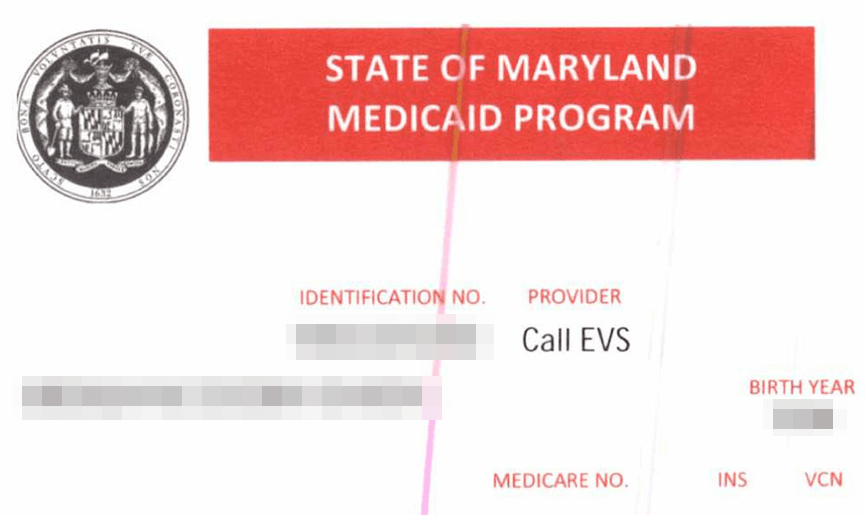
Maryland Medicaid - MAMD-F
Identifier: State of Maryland Medicaid program listed at the top
What should staff do if they receive this card at check-in?
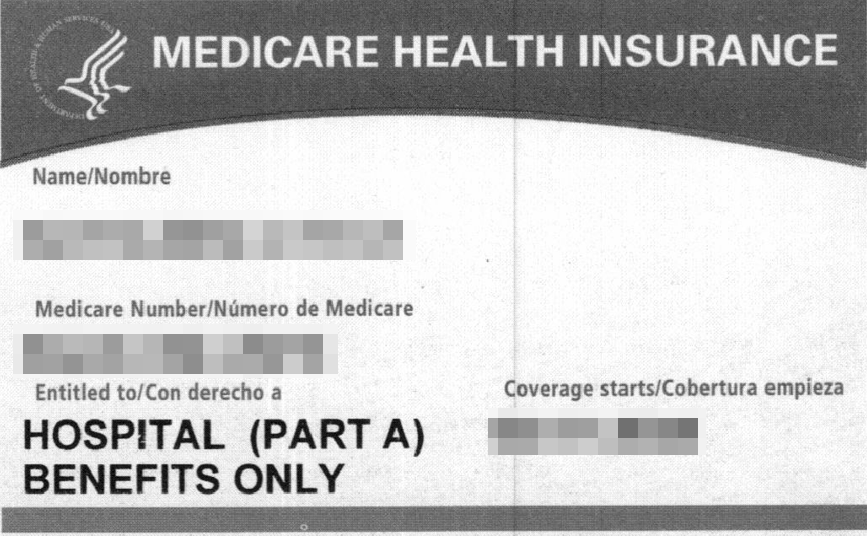
DO NOT enter into Expanse. Ask the patient if they have other medical coverage.
This is a Medicare Part A ONLY - Not to be billed for outpatient/ambulatory services
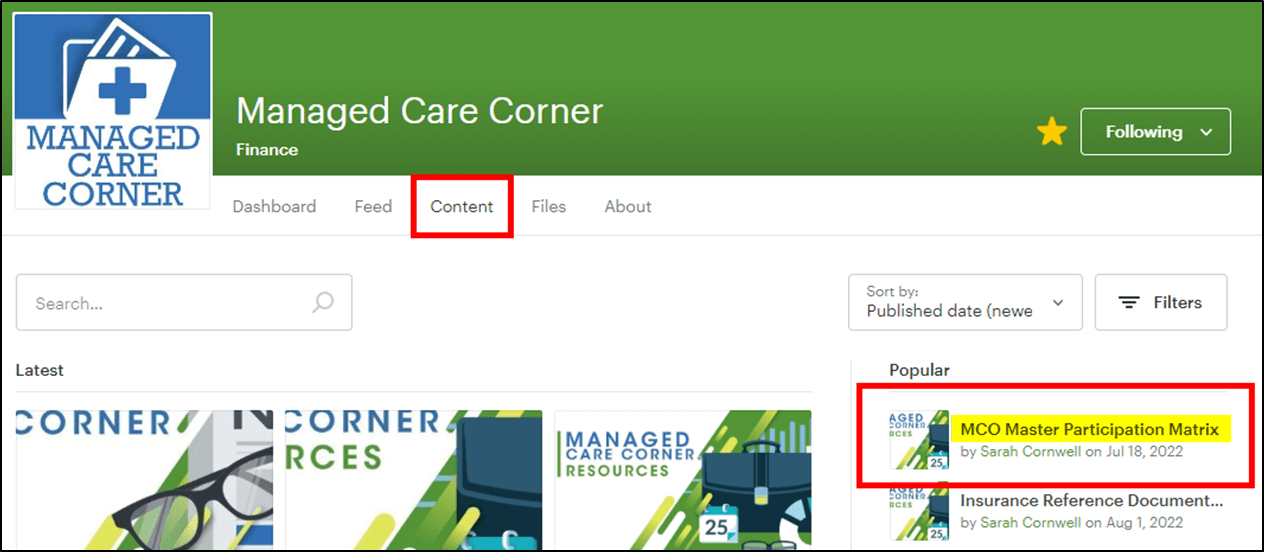
When should you reference the Master Matrix AND where is it located?
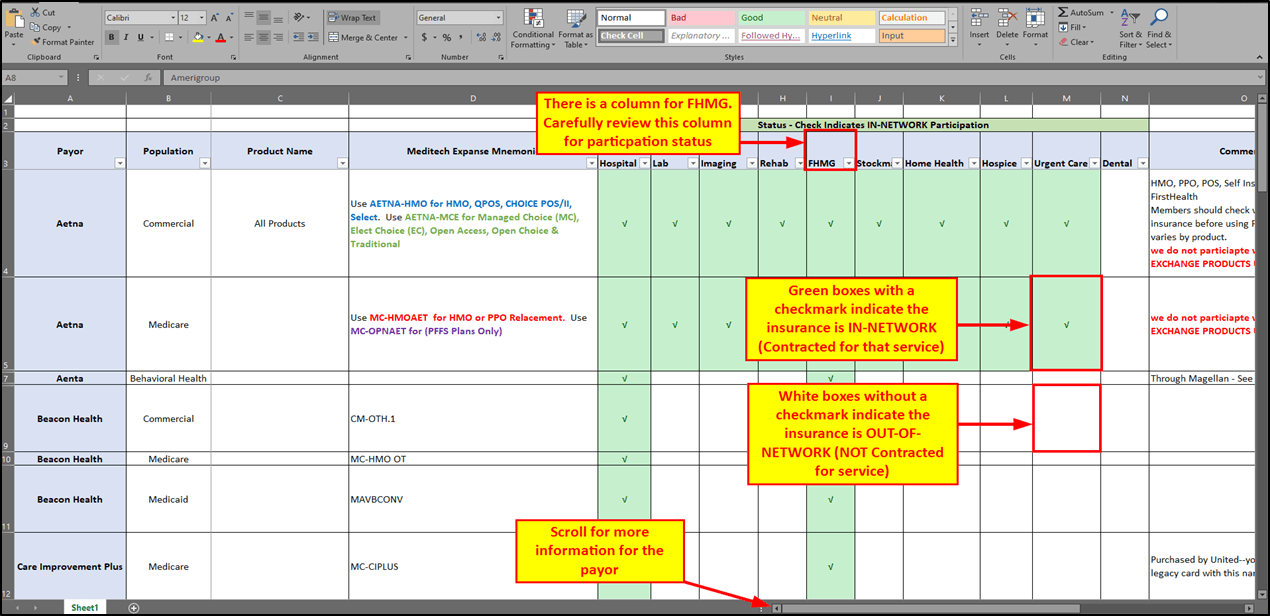
When looking for the insurance network participation status
It’s located on the Managed Care Corner via the FH Intranet.
Is Frederick Health contracted with Out Of State
Medicaid's?
NO. We are only contracted with MARYLAND Medicaid
What is the correct Expanse Name or Mnemonic for this Insurance card?
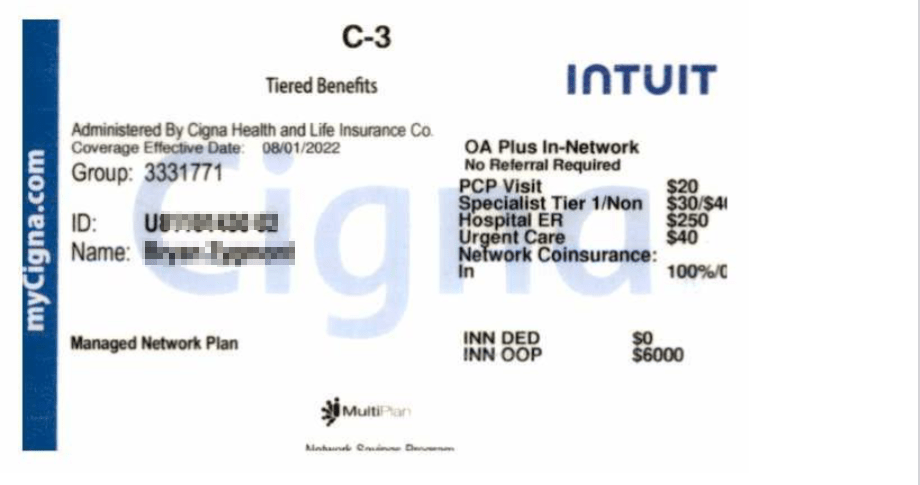
Cigna Healthcare - CIG-MD-HM
Identifier: OA Plus In network
Carefirst/Blue Cross Blue Shield member ID numbers always begin with a ___ prefix
Letter Prefix
Leaving out the letter prefix for a Carefirst/Blue Cross Blue Shield card can result in a denied claim.
What is the correct Expanse Name or Mnemonic for this Insurance card?
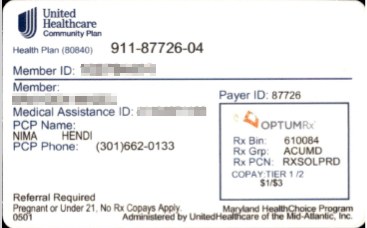
United Community Plan - MA-HMOUHC
All Medicaid Plans require a PCP selection but only 2 plans require a specialist referral. What 2 plans require a referral
Priority Partners and UHC Community Plan
What are the identifiers for a Medicare Advantage (aka Part C or Replacement) insurance?
-Medicare Rx logo
-'Medicare' and/or 'Advantage' on the card
To add a WC or auto insurance to the patient's chart, what must the patient supply?
The claim number. Without the claim number, staff will override and keep the account as Self-Pay.
FHMG is currently enforcing the No Surprises Act by providing Self Pay patients with a ___________ 3 days prior to the visit
Good Faith Estimate
What is the correct Expanse Name or Mnemonic for this Insurance card?
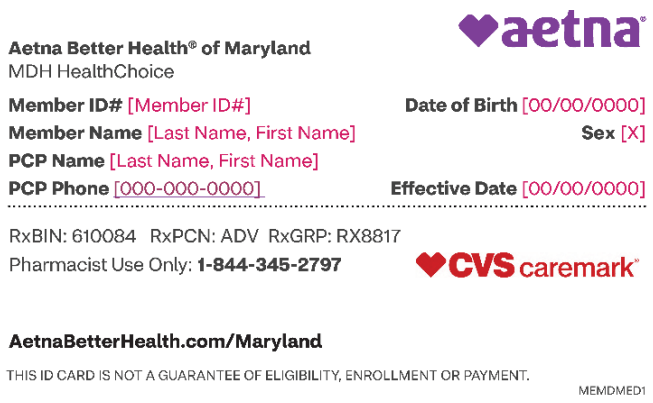
Aetna Better Health of MD - MA-HMAETMD
NON-CONTRACTED - Direct to an in-network provider
Identifiers: Aetna Better Health Logo on the top left of the card
What is the correct Expanse Name or Mnemonic for this Insurance card?
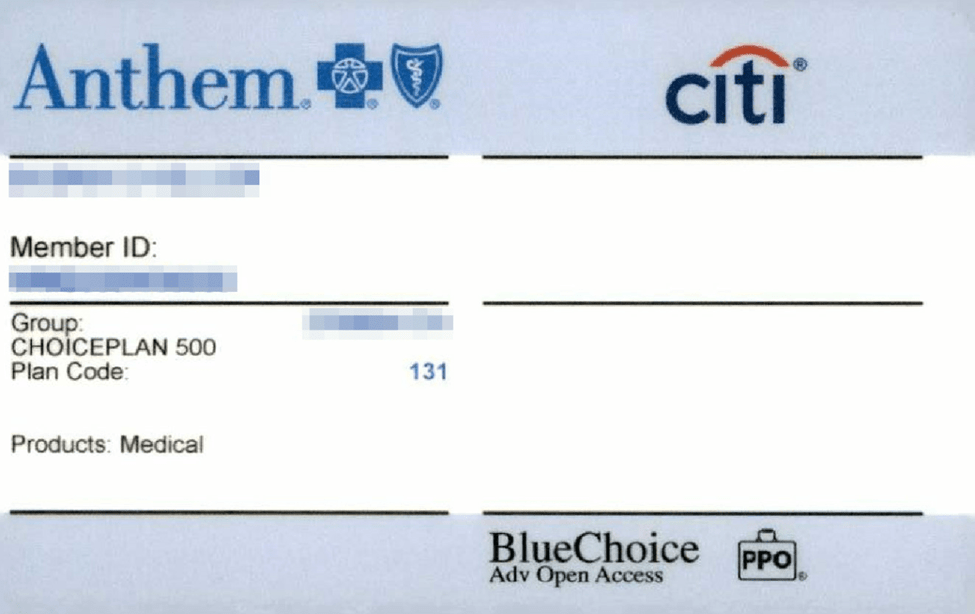
BC Blue Cross Bluecard - BC-OTH.1
Identifiers: Anthem, non-local plan # (131)
What is the correct Expanse Name or Mnemonic for this Insurance card?
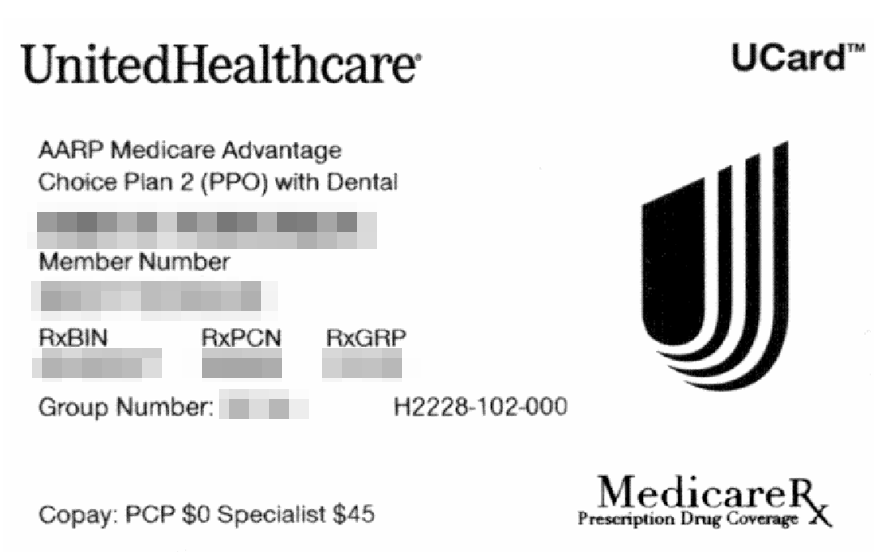
MC United Medicare PPO - MC-PPOUHC
Identifiers: AARP followed by "Medicare Advantage"
True or False: Patients with a non-contracted Medicaid can opt to be self-pay to receive services at our facilities.
FALSE
Staff must direct patients to an In Network provider - Medicaid does not have out of network benefits
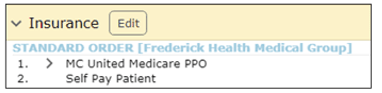
True or False: When a patient has a Medicare Advantage insurance, you must delete their Medicare AB from their chart.
TRUE
Medicare Advantage insurances replace traditional Medicare AB. Staff must remove Medicare AB from the chart for correct billing.
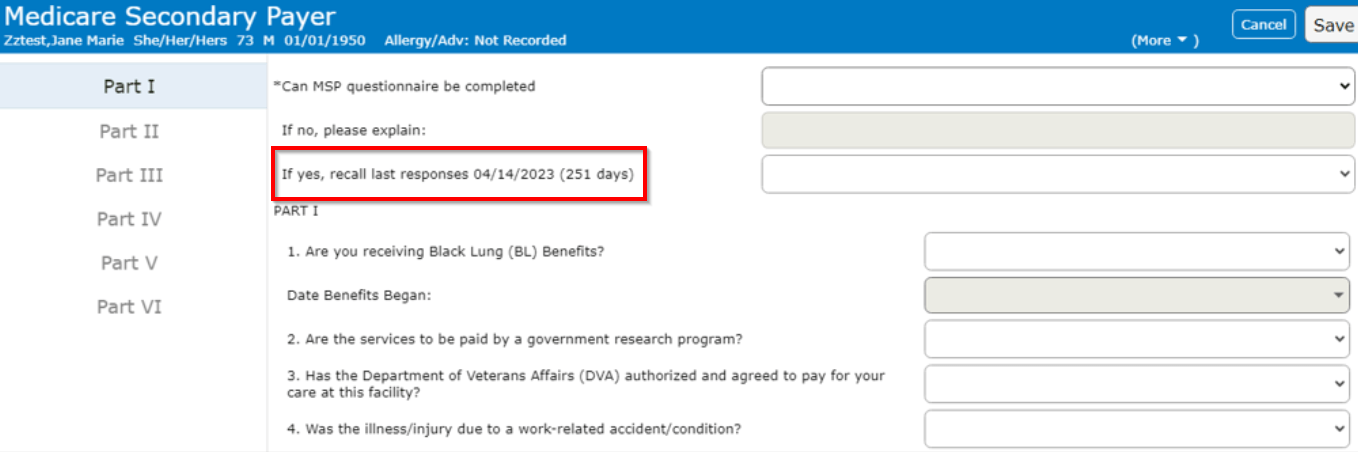
For patients with Medicare:
When completing the MSP questionnaire, you can demo recall the responses within a certain timeframe. What is the timeframe?
Within the last 90 days
If the last MSP responses are older than 91 days, you must interview the patient for updated responses.
Where in the patients chart can you find the Financial Assistance Validity dates?
Customer Defined tab

What is the correct Expanse Name or Mnemonic for this Insurance card?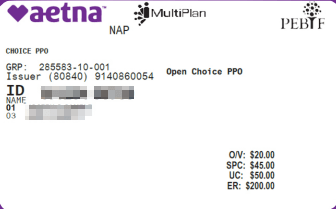
Aetna-MCE
Identifier: Open Choice / PPO
What is the correct Expanse Name or Mnemonic for this Insurance card?

CareFirst Commun Hlth Plan MD - MA-HMOCFHP
Identifier: CareFirst Community HP logo at the top left of the card
What is the correct Expanse Name or Mnemonic for this Insurance card?
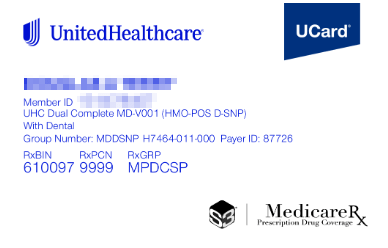
UHC Dual MC Advantage - MC-DUALUHC
Identifier: Medicare RX logo at the bottom right & Dual Complete listed under the member ID number
Maryland offers 9 Medicaid MCO plans,
Which are non-contracted?
•Aetna Better Health
•JAI Medical Systems
•Kaiser Permanente
•Medstar Family Choice
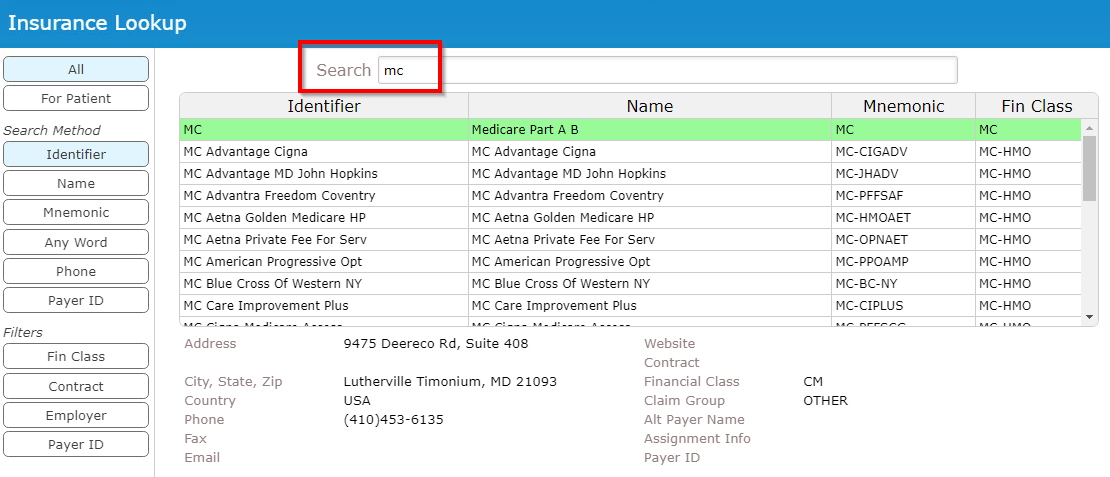
When entering a Medicare Advantage insurance, what 2 letters should you search in Expanse?
MC
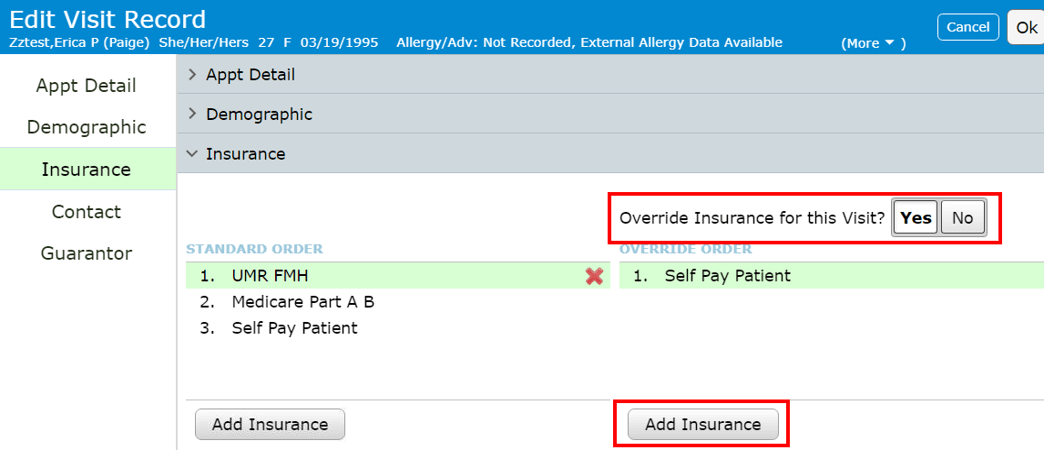
Patient presents the following Insurance cards at check in - What mnemonic do you enter into Expanse
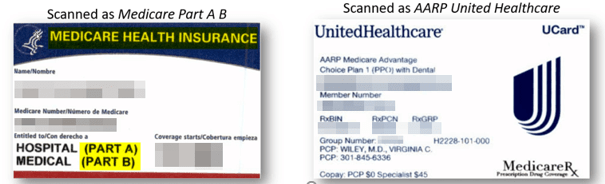
Medicare UHC PPO - MC-PPOUHC
If a patient has CareFirst Primary with a $30 Copay and FA 80% Secondary, How much money am I collecting from the patient?
$6.00

What is the correct Expanse Name or Mnemonic for this Insurance card?
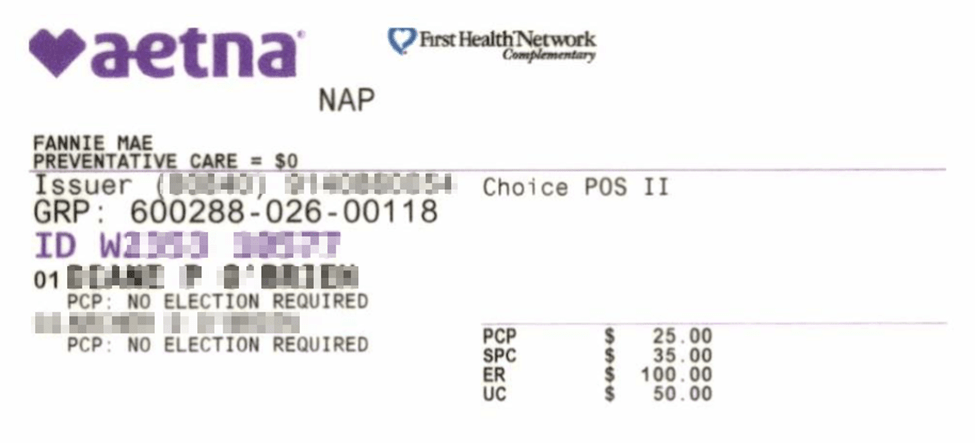
Aetna HMO QPOS
Identifiers: "Choice POS II" top right
What is the correct Expanse Name or Mnemonic for this Insurance card?
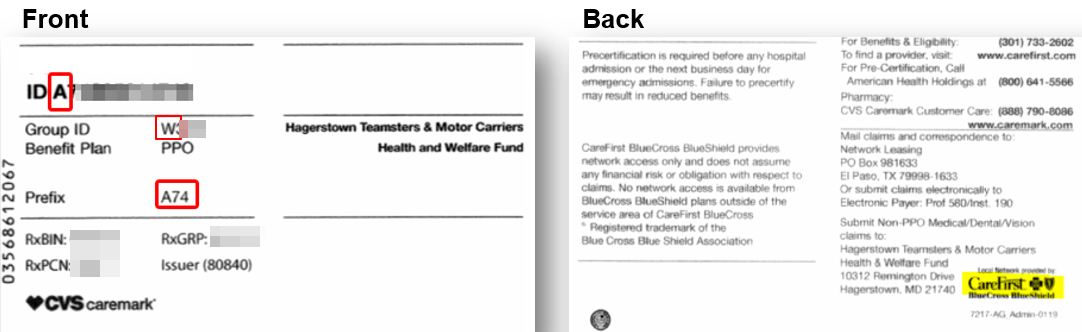
BCBS NCAS BC - NCAS-BC
Identifiers: 'A' member ID prefix, 'W' group number prefix, union top right
What is the correct Expanse Name or Mnemonic for this Insurance card?
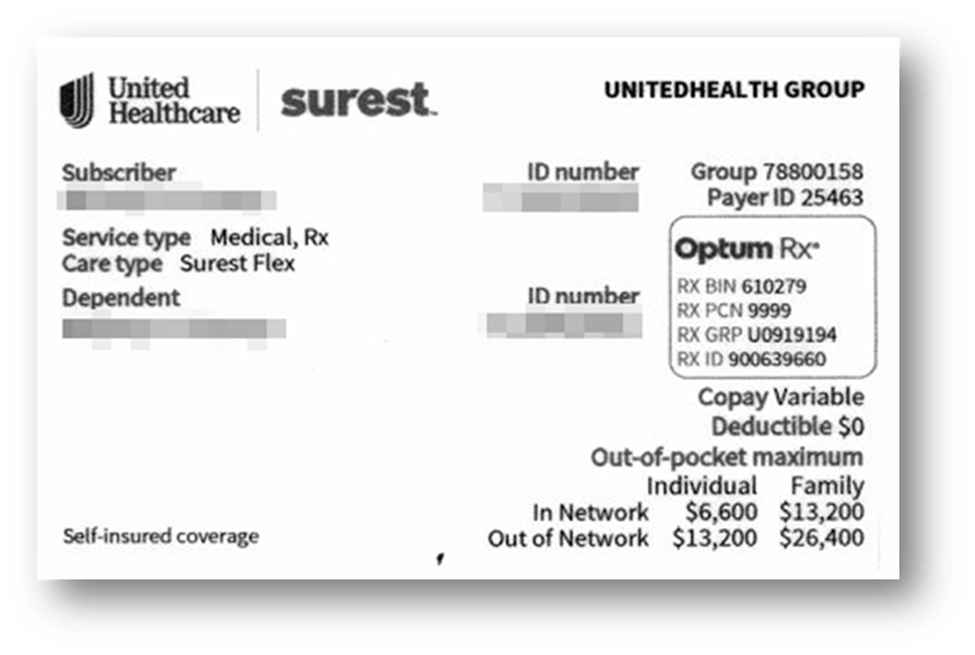
Commercial OTH 1 - CM-OTH.1
Identifiers: United HealthCare Logo on the Card along with the Surest Logo
True or False: The patient is always their own subscriber for Medicaid payers, even if they are a minor.
TRUE. The patient is always the subscriber on Medicaid plans
What is the correct Expanse Name or Mnemonic for this Insurance card?
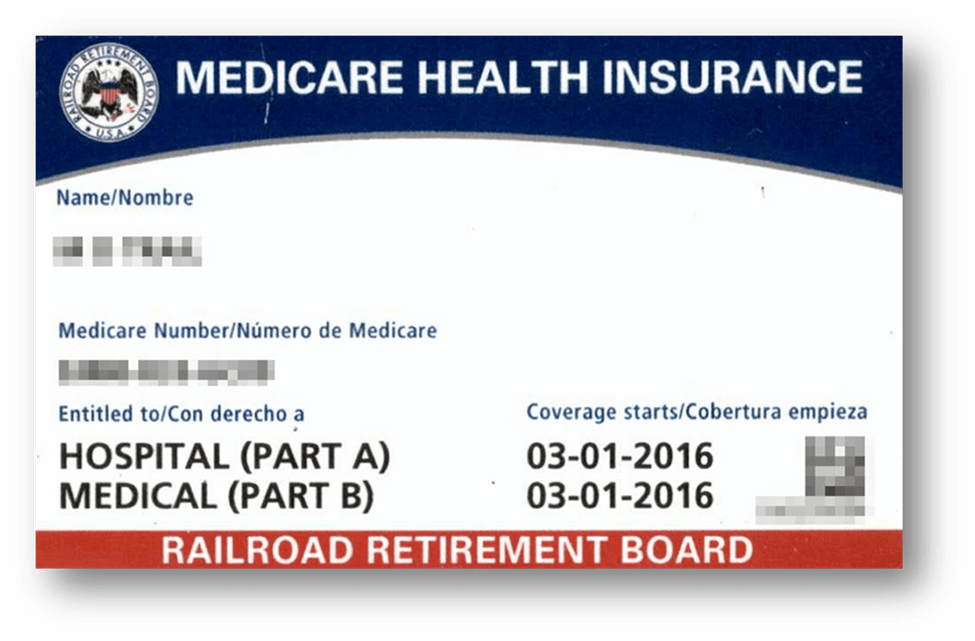
Medicare Railroad - MC-RRMG
Identifiers: "Railroad Retirement Board" banner along the bottom
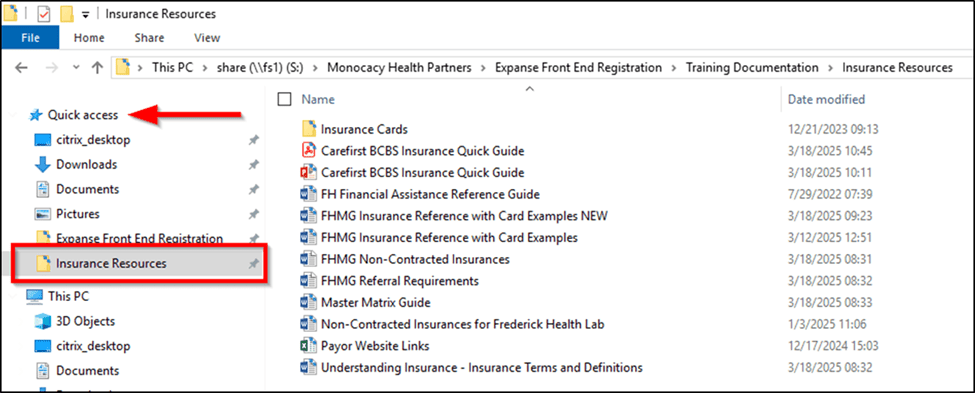
You all have resources printed from today’s date, but how often should you check for updated information?
Once a month, at the minimum
Ensure to pin the Insurance Resources folder for Quick Access to these resources.
What 4 scenarios are claim codes required for?
- Patients with any BCBS/Carefirst insurance (11)
- Automobile Insurance (2)
- Workman’s Compensation (4)
- Patients presenting with an injury (ex: fall, sprain, burn) (5)