Describe the flexor zones
 1) distal to FDS insertion on middle phalanx
1) distal to FDS insertion on middle phalanx
2) FDS insertion-A1 pulley
3) A1 pulley-distal edge of transverse carpal ligament
4) carpal tunnel
5)proximal to proximal aspect of transverse carpal ligament
T1- distal to thumb IP joint, T2- thumb A1 pulley to IP joint T3-thenar eminence
Ideally, how far from each flexor tendon edge should your suture bite be?
1cm
What physical exam signs can indicate a flexor tendon injury? name two possible findings
1. loss of active flexion
2. loss of normal finger cascade
3. no passive movement on squeeze compression of forearm bulk
4. loss of tenodesis effect
You should repair a flexor tendon if the laceration is greater than __% of the tendon width
60%
if less than that, not worth the risk of disrupting blood supply
Name the flexor compartments and what muscles are in them
Intermediate: FDS
Deep: FDP, FPL
Which FDS tendons are superficial vs deep in relation to each other?
FDS tendons of middle and ring are dorsal to FDS tendons of small and index
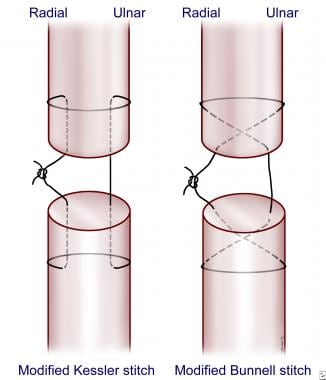
The strength of tendon repair is proportional to _____
The strength of the tendon repair is proportional to the number of core strands that cross the tendon gap.
recommended: 4-6
When is tendon repair with a graft indicated? What tendon is commonly used?
If the ends of the tendon are degenerated, if the injury is >3 weeks old, if primary repair fails (ruptures or too many adhesions)
palmaris longus most common, or plantaris or toe extensor
When shouldn't you repair a tendon primarily?
1. lack of stable soft tissue coverage
2. gross contamination
3. human bite as mechanism
note: all flexor tendons should be repaired in the OR (contrary to extensor tendons which can be repaired at bedside)
Name the 4 kanaval signs.
bonus 50 points: which is the most informative of these?
1. Finger held in flexion
2. Pain with passive extension of digit at DIP (most informative)
3. Tenderness along flexor sheath
4. Fusiform swelling of digit

FDS divides into two slips at the A1 pulley and come together at __________ at the distal end of the proximal phalanx
camper's chiasm
When (time-line) is a tendon repair most vulnerable and when is it back at full strength?
Weakest days 5-21 (day 10 most common for rupture), strength of repair is dependent on the suture
Back at full strength in 3 months
What are "no mans land" injuries and what is their significance?
Bonus 100 points: where did the name for this type of injury come from?
zone 2 injuries- they affect FDS and FDP, and its common for adhesions to form here and restrict movement. Nowadays we repair both tendons, used to only encourage repair of FDP
Bonus answer: Bunell's WW2 experience in France- no mans land is the strip of devastated land between two army trenches
After a tendon repair, the wrist should be splinted in 20 degrees ___, mp joints in ______ and all digits should be held in ____ to avoid contractures
20 degrees flexion, MP joints 60 degree flexion, all digits should be held in full extension to avoid contractures
which pulley is most important for thumb flexion?
oblique pulley (over proxima phalanx)
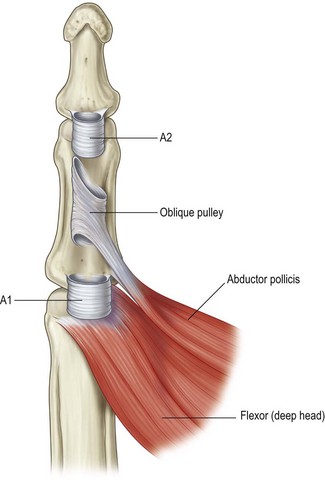
Describe the difference between annular and cruciform pulleys
Annular- have 3 layers, strong, major in preventing bowstringing of tendons during flexion
Cruciform- thin and collapsable, connect the annular pulleys, allow for flexion without deforming the annular pulleys
How soon after a tendon repair should you start early motion?
Important to start active motion by days 3-5 (if start between day 5 and 28, increased risk of tendon rupture)
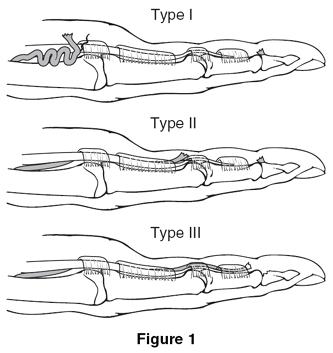
Describe the first 3 leddy and packer classifications of jersey finger injuries
Jersey finger: Closed FDP avulsion
1: FDP tendon retracted into palm (urgent surgical reattachment, vinculae to FDP are ruptured and if you wait >3 weeks repair will fail due to poor blood supply- Michigan manual says 1 week tho)
2: FDP tendon retracted to proximal phalanx and held at FDS decussation (long vinculae intact, can wait up to 3 months and reattachment will likely have successful repair)
3: Large bony avulsion holds tendon at A4 pulley, preventing retraction past DIP joint (k wire or screw)
When is tenolysis indicated?
when adhesions limit motion and there is a discrepancy between active and passive ROM that doesn't improve over a 3 month period
What are tendons made of?
Tyle 1 collagen, water, elastin, ground substance like glycoproteins
What are the three layers of annular pulleys?
middle layer- collagen, resists palmar translation of tendons
outer layer- facilitates nutrition for tendon
Describe the stages of tendon healing and their timeline
Days 1-3ish: inflammation- cytokines, phagocytes
Day 5ish-28: fibroblasts make collagen, realigns and thickens (boosted by early active motion)
Days 28-3 months: Remodeling
Describe both stages of a two stage tendon graft for flexor tendon repair and how long do you wait between the stages?
stage 1: silicone rod inserted through pulley system to recreate a smooth tunnel for future tendon graft. Can attach the rod to stump of FDP and leave other end free in palm or wrist. Repair A2 and A4 if needed.
8-12 weeks later (all the while doing passive ROM)
stage 2: expose the rod at both ends, attach a harvested graft to distal end of the rod and pull it through the newly formed tunnel.
What is the Quadregia effect
Incomplete flexion of FDPs of un-injured long, ring, or small fingers when the shortened FDP reaches max flexion too early (due to their shared common muscle origin)
 Happens if, during flexor tendon repair, you advance FDP more than 1cm or if scar tissue develops
Happens if, during flexor tendon repair, you advance FDP more than 1cm or if scar tissue develops