The hallmark tenet of a diagnosis of multiple sclerosis
What is dissemination in space and time?
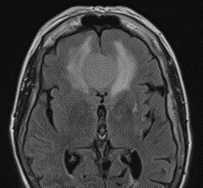
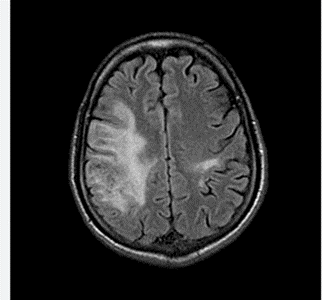
The type of edema seen on this MRI Flair scan of a mass in the right frontal lobe
What is vasogenic edema? Edema in which there is disruption of the blood brain barrier. Extracellular edema, affects white matter due to leakage of fluid from capillaries. On CT scans the grey-white differeniation is maintaind; edema involves white matter. On MRI studies, this shows up as hyperintensity on T2 and FLAIR that does not diffusion restrict
Different from cytotoxic edema in which the blood brain barrier is intact. Most commonly seen in ischemic lesions. Result of intracellular injury--cannot maintain ATP Na/K pumps, Na and Chloride accumulates in the cell and draws water in, cells swell and reduces extracellular volume, affects grey matter and white matter as well. Best seen on diffusion weighted imaging
The neurologist who coined the term asterixis with colleague Raymond Adams in the 1940s.
Who is Joseph Foley. Dr. Foley is the father and founder of the neurological division at University Hospitals; under Dr. Foley he built a division of neurology within the Department of Medicine. Story goes that he consulted a Jesuit Scholar from Boston College. Dr. Foley and Father Cadigan drank metaxa (Greek spirit, a wine with botanicals) and came up with the term an (negative) - iso (equal), and sterixis (solidity of firmness). Anisoterixis was too many syllables, and thus shortened it to asterixis.
The syndrome characterized by altered consciousness, eye movement restrictions and abnormalities and ataxic gait and related to ETOH use
What is Wernicke's Syndrome? Carl Wernicke first described this in 1881, sudden onset illness in those using ETOH.
What vessel size type is affected in giant cell arteritis? (i.e. small, medium, large....)
What are medium and large sized vessels. In the head and neck, can include superficial temporal artery, occipital artery, post auricular, facial arteries; blood vessels of the eye and optic nerve, vasculitis leading to stroke
The syndrome name for an acquired demyelinating neuropathy charachterized by opthalmoplegia, ataxia and areflexia?
What is Miller-Fisher Syndrome. Associated with ganglioside GQ1b antibody, present in 80% of those with this condition.
Bickerstaff brainstem encephalitis can overlap with some symptoms, also associated with GQ1b, includes altered conciousness, extensor plantar response and hyperreflexia due to CNS involvement.
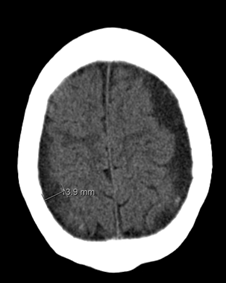
The hematoma seen in this CT Head without contrast is between which two layers?
What are the arachnoid and dura mater? Seen on this study are bilateral subdural hematomas. Blood collects between the dura and the arachnoid mater. Risk factors include head injury, atrophy, anticoagulation, CSF leaks, ETOH use, high-impact sports, diabetes mellitus, thrombocytopenia, epilepsy, arachnoid cysts, cardiovascular disease. Annual incidence is 1-5.3 cases per 100,000 population.
The neurologist who coined a type of meningitis after his own last name with the following charachteristics: recurrent or chronic aspectic meningitis. Most common virus to do this is HSV, especially HSV 2.
Who is Pierre Mollaret. First described in 1944. The most common virus is HSV, but can be other viral causes as well including VZV. EBV, coxsackie, echovirus. Of note, PCR testing can be negative though the symptoms of meningitis are present and severe. Acyclovir is treatment of choice. Can resolve after 3 to 5 years, but some have a much longer disease course. Indomethacin 25 mg TID, can result in faster recovery.
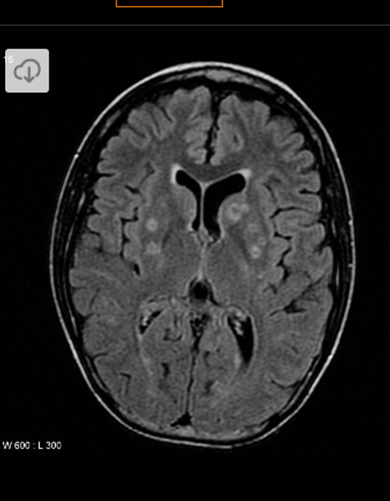
A patient presents with altered mental status, fever, and change in speech. As part of work-up they are found to be leukopenic with WBC 2. You see several ring enhancing lesions above. Concern develops that patient has undiagnosed HIV and testing confirms this suspicion. What is the likely etiology of the ring-enhancing lesion above? It is not CNS lymphoma or cryptococcus.
What is Toxoplasmosis gondii? A intracellaluar protozoan parasite. Infection--ingest food or water contaminated by oocytes excreted by cats or improperly cooked eat. The tachyzoites multiple, invade cells and disseminate via blood and lymph system. If immunocompetent, can have a chronic, quiescent life-long infection without eradication.
In HIV, opportunistic infections occur when CD4 T-cell count is low.
It is estimated that 1/3rd of the global population has latent toxo.
In HIV patients--can present as encephalitis, chorioretinitis, pneumonitis, or disseminated diseaes. Predilection for the basal ganglia, frontal lobe, parietal lobe.
Symptoms can include fever, neuropsych symptoms, hallucinations, stroke-like symptoms.
Differential in an immunocompromised patient includes CNS lymphoma, PML, TB, focal cryptococcus, CMV, and bacterial brain abscess.
What is the most common neurologic symptom of giant cell arteritis?
Headache. Remember that the headache can be temporal, but not always. An occipital headache or a pain in a different area does not mean it is not GCA!
The demyelinating condition that can often present with a longitudinally extensive spinal cord lesion, aka a severe transverse myelitis
What is NMO or NMO spectrum conditions
Most meningiomas are considered benign in pathology. However a percentage of them are malignant. What is the percentage of all meningiomas that is considered atypical and/or malignant?
What is 10-15%? Most meningiomas are benign in pathology about 85-90% of the time. 10-15% are atypical meningiomas or malignant.
Of note the word benign here refers to the histopath and does not mean a benign mengioma will not cause compression or a neurologic deficit or symptoms by way of its growth or compression.
About 3% of those over the age of 60 have a meningioma.
As with other tumors, there is a grading system for meningiomas based on their pathology. Grades are between 1 through 3.
Grade 1 -- most common, slow growth, log grade tumor cell type
Grade 2-mid-grade, atypical meningiomas. They have a higher chance of growing back after removal. Choroid meningioma and clear cell meningioma are part of this category.
Grade 3--fast growing, anaplastic malignant tumors--high grade. Papillary and rhaboid meningiomas are types.
The syndrome named after the person who spoke these words. "How the theater of the mind could be generated by the machinery of the brain."
What is Charles Bonnet Syndrome. Charles Bonnet, a lawyer with a strong hobby in studying natural science, described this condition based on observations of his own 87 year old grandfather, who had vision loss due to cataracts.
A simplistic explanation of Charles Bonnet Syndrome is that as vision is lost, the visual system cannot process new images correctly. However the visual processing portions of the brain are still working and will create visual hallucinations.
The essential vitamin that has a half-life of 18 days. Its deficiency is associated with beriberi.
What is thiamine? Needed for thiamine pyrophosphate, cofactor of citric acid cycle and needed for sugar breakdown. Citric acid cycle is necessary for carbohydrate, lipid, amino acid metabolism. Thus if thiamine deficient, one would inhibit many molecules including neurotransmitters glutamic acid and GABA. Thiamine is also involved in neuromodulation. Thiamine deficiency is thought to be major contributor to Wernickes in those with poor nutrition including ETOH abuse.
In contrast, the half-life of B12 is years (2-5 years in some studies). One area that B12 is stored is in the liver.
The approximate percentage of cocaine that has been found to have adulterant levamisole?
What is above 70% according to studies from early 2000s. More recent articles from 2021, suggest that the percentage is ~ 87%. Leviamisole used for cancer and Rheumatoid arthritis treatment before being pulled off market in 2000 due to side effects. Used in veterinary med as antihelminthic agent. Levamisole-laced cociane can lead to neutropenia, agranulocytosis, arthralgias, retiform purpura, and skin necrosis--look for purple ears and nose. In the brain, can be associated with toxic leukoencephalopathy.
The brain region that if hurt can be involved in severe nausea, can be preferentially involved in NMO
What is the area postrema
What type of brain cell is the target of the condition that is most likely represented by the below images? 
What are astrocytes. Inflammation in NMO spectrum disorders primarily seem to target astrocytes. AQP4 is a water channel that is present in the foot processes of astrocytes. It is concentrated in the spinal cord gray mater, periaqueductal and periventrical areas.
The "classic" name of a rapidly progressive neurodegenerative condition, caused by the abnormal isoform of prion protein
What is Creutzfeldt-Jakob disease (CJD). In the US it is estimated to be one case per million. Most will die within 1 year of onset of symptoms. In about 85% of cases, this occurs as sporadic disease without any family history or known genetics. In about 5-15% they develop CJD due to mutations in the prior protein gene. The disease was first described in the 1920s by the German neurologists Hans Gerhard Creutzfeldt and Alfons Maria Jakob.
Clues towards this diagnosis can be a rapidly progressive neurodegenerative condition, startle myoclonus, periodic sharp waves on EEG.
To diagnose, testing is done of CSF fluid and through the national prion center which is outside the door of our adult EMU, they arrange for autopsies to confirm tissue diagnosis.
We are careful not to confuse classic CJD with variant CJD. Variant CJD initially described in 1996 in the UK, with strong evidence supporting that the agent responsible for prion disease in cows (Mad Cow disease) is the same agent responsible for vCJD in humans.

The most common vitamin deficiency associated with the MRI Findings in this picture
What is B12 deficiency? Leading to subacute combined degeneration of the dorsal columns and lateral columns due to demyelination. Symptoms can include sensory deficits, paresthesias, weakness, ataxia, gait changes. Can lead to spasticity and plegia in severe cases.
We get cobalamin from meat, fish, dairy and eggs and fortified cereals. Richest sources are clams and animal liver. History taking should focus on diet, GI symptoms and history, autoimmune disease, and drug-induced causes including gastric acid suppressants, metformin, and nitrous oxide abuse. Lesser causes in the US are tapeworm infections and genetic causes.
The percent range of those with GCA have PMR?
What is about 60% (58%). PMR affects proximal, axial joints, with elevated ESR as well. Responds to low dose steroids. PMR prevalence is 1 in 133. ~ 15-20% with PMR develop GCA. ~ 60% of individuals with GCA, have PMR.
A chronic motor only demyelinating acquired condition that involves classically conduction blocks that can be asymmetric in presentation
What is Multifocal Motor Neuropathy
The above is a pictorial of IgG. It is the only Ig that has the ability to exchange its arms as shown above. We talked about IgG. This question is twofold:
1.) What is the IgG type of MUSK myasthenia gravis--Is it IgG1, IgG2, IgG3, or IgG4?
2.) What is the half-life of all IgG?
1.) What is IgG4 for Musk Myasthenia Gravis. This is important to know because an IgG4 mediated disease can be treated with medications such as Rituximab. Further, in AchR positive MG, the destruction is caused in part by activating the complement cascade. In MUSK MG, the destruction is not caused by the complement cascade. It is caused by blocking assembly of agrin-LRP4-Musk complex, results in slow dissembly of the AchR clusters--leads to less miniature endplate potential and EPP, leads to failed muslca action potential and weakness.
AchR MG is caused by IgG1 and IgG3.
2.) Half life of IgG is 21 days. This is due to the FcRn system which essentially helps to recycle IgG. When IgG is bound to FcRn, it is protected from being degraded by lysosomes.
For comparison, the half-life of
IgA and IgM- 4 to 6 days
IgE - 2 to 3 days (can be up to 9 to 12 weeks if bound to a particular receptor)
What is the eponym of JC Virus? Aka..what is the full name of JC?
Who is John Cunningham? JC virus is also known as human polyomavirus 2. Virus was named after the patient in whom this virus was first identified in 1971.
The above is an MRI of PML in a HIV positive patient. It is caused by JC Virus which causes a lytic infection of what brain cell?
What are oligodendrocytes? PML is a potentially fatal brain demyelinating disorder from JC Virus. It is a lytic infection of oligodendrocytes (and astrocytes).
For those with JC Virus, often it remains asymptomatic and quiescent in the kidneys, bone marrow and lymph tissues.
When immunocompromised, virus gets reactivated and may migrate to the brain, where genetic changes to the virus can occur.
The most common opthalmic manifestation of systemic sarcoidosis?
What is anterior uveitis. The exact incidence is widely variable depending on studies, some citing 10-50%.