This organ secretes both exocrine and endocrine hormones.
What is the pancreas.
What is the common patient presentation of pancreatitis?
Acute onset of severe epigastric or abdominal pain.
50% of patients state it radiates to the back and is relieved by leaning forward
90% present with nausea and vomiting
Severe pancreatitis can present with dyspnea from diaphragmatic inflammation
What are the four possible findings on plain film for Acute Pancreatitis?
What are "sentinel loop, colon cut off, diffuse illeus, and pleural effusion".
- IMPORTANT: The abdominal xray is not diagnostic and is frequently normal. OR it may demonstrate any of the aforementioned.
What is the normal range for Amylase?
What is 60-120 units/dL
What do elevated Amylase levels indicate and when do they rise? What is their half-life?
What is Pancreatitis and or obstruction of the pancreatic duct flow. Levels rise with 6-12 hours and they have a half life of 10 hours.
What are the pancreas exocrine hormones and their function?
- What is Amylase to digest carbohydrates.
- What is Lipase to digest fats.
What does a Physical exam of pancreatitis typically reveal?
Can range from minimal tenderness to severe epigastric tenderness
Can have hypoactive bowel sounds and distention from an ileus
Fever, tachypnea, hypoxemia, and hypotension in severe pancreatitis
Ecchymotic discoloration may be observed in the periumbilical region (Cullon's sign) and on the lower back (Gray Turner's sign)
Rare cases show pancreatic panniculitis
What are the Abdominal ultrasound findings?
What are diffusely enlarged and hypoechoic and peripancreatic fluid appears as an anechoic collection.
- 25 to 35% of patients with acute pancreatitis, bowel gas due to an ileus precludes evaluation of the pancreas or bile duct
What is the normal range for Lipase?
What is 0-160 units/L
What do elevated Lipase levels indicate and when do they rise? What is their duration?
What is elevated lipids are more specific. Pancreatic disease elevations are 5-10x the normal values. Lipase levels rise in 4-8 hours, peak at 24 hours, and return to normal in 8-14 days.
What are the Pancreas endocrine hormones?
What are "insulin, glucagon, somatostatin and pancreatic polypeptide".
What is this: 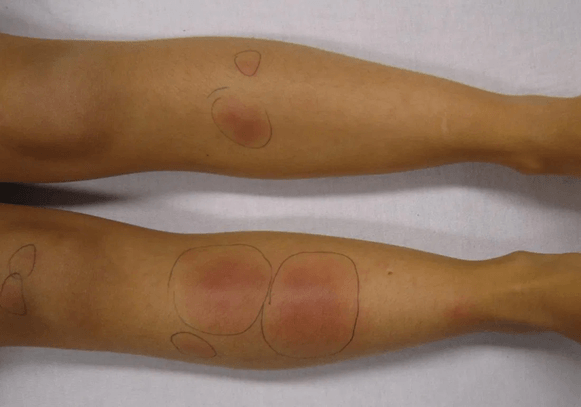
What is Pancreatic panniculitis. 2-3% of all patients get this fat necrosis.
What is the best imaging test for pancreatitis?
What is contrast-enhanced abdominal computed tomography.
This can show:
- focal or diffuse enlargement of the pancreas with heterogeneous enhancement with IV contrast
- Common bile duct stone may be seen
- Pancreatic mass (cancer)
Where is Trypsinogen Activation Peptisede realeased and what does it do?
What is normally produced in the pancreas and released into the small intestine.
Trypsinogen is then converted to trypsin and it breaks down proteins.
What do low levels and/or elevated levels of Trypsinogen Activation Peptide (TAP) tell you?
Low levels: pancreatic insufficiency
Elevated levels: Abnormal production, Acute pancreatitis, Cystic fibrosis (used for screening for this), and Pancreatic cancer
What are the major contributing factors to the common disorders of the pancreas such as pancreatitis and pancreatic cancer?
What are "stemming from gallbladder stones, smoking, high consumption of alcohol, and DM".
What are the four Laboratory values assessed for suspected Pancreatitis?
What are "Amylase, Lipase, Trypsinogen peptide (TAP), and C-reactive protein (CRP)".
What imaging test can you use in acute situations or when patient cannot handle CT contrast as in allergy or renal failure?
What is Magnetic resonance imaging (MRI).
- diffuse or focal enlargement of the pancreas with blurred margins
- this test takes long
What is the normal range for C-Reactive Protein?
What is <10mg/L SI units.
What does C-Reactive Protein indicate and is specific or nonspecific?
What is it as an acute phase reactant protein used to indicate an inflammatory illness. It is nonspecific!
Where is the pancreas located anatomically?
What is sits across the back of the abdomen, behind the stomach. The head of the pancreas is on the right side of the abdomen and is connected to the duodenum.
What are the Imaging results found on Abdominal and Chest xrays for pancreatitis? Think Mild disease, Moderate disease, and Severe disease.
Mild disease: no findings
Moderate disease: localized ileus in a segment of small intestine (sentinel loop)
Severe disease: colon cut off sign: paucity of air in the colon distal to the splenic flexure due to functional spasm of the descending colon
Other findings (1/3 of patients)
- elevation of a hemidiaphragm, pleural effusions, basal atelectasis, pulmonary infiltrates, or acute respiratory distress syndrome
When are elevated levels not due to a pancreatic origin?
What are Penetrating peptic ulcer, duodenal obstruction, bowel perforation, patients with mumps (salivary glands), severe diabetic ketoacidosis, appendicitis, ruptured ectopic pregnancy, ovarian cancer.