lasts longer!
Wound care guideline for treatment after placing a wound care consult.

What is skin prep daily and PRN, open to air.
Patient with severe diabetic ulcers.
What is podiatry service.
Day of the week that staff update pressure injury pictures in the media.
What is Wednesday.
4 eyes in 4 hours.
What is 2 RN skin check completed and documented on admission to any unit, transfer to any unit, and after a procedure.
A Braden scale indicating high risk.
What is 18 or less.
Your patient is admitted with this and states they have had it for 2+ years. Upon assessment there is scant purulent drainage, and the wound bed is pale with a callous. Using the wound care guidelines you recommendation would include these items.
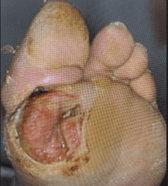
What is a podiatry consult and for the interim, lightly pack with Vashe or Dakins solution moistened kerlix; change twice daily.
Venous stasis ulcers that are deteriorating since admission 6 days ago despite following the wound care guidelines.
Wound care and consider vascular consult.
An item that should be present in the media photo when uploading to the chart.
What is a ruler with the patient's name and birthdate on it.
Risk notification of wounds on admission, transfer, new wound or if a wound deteriorates
What is Safety Net.
All heels should be this.
What is offloaded.
Recommendations using wound care guidelines for no drainage and dry wound bed.

What non-adherent petrolatum gauze or Medihoney.
Patient has a rash that covers their chest, arms and back.
What is notify the covering provider and possible Dermatology Consult
Criteria for Wound Care consult.
What is Stage 3/stage 4 PI, unstageable PI, evolving DTIs on sacrum, stable diabetic foot wounds, new ostomy patients, complex fistulas, full thickness wounds and xylazine wounds with large areas of necrosis/malodorous.
An important assessment strategy when assessing a vulnerable area at risk.
What is good lighting.
This area is nonblanchable.

Stage 1 pressure injury.
Describe the wound edges.
What is macerated and epibole (rolled).
Patient has an extensive wound over their sacrum.
What is Wound care.
Important aspects of a wound assessment.
What is palpation, signs of infection (erythema, induration, crepitus), pain associated with wound area.
Hospital acquired injuries are considered these two things.
What is a never event and a nursing sensitive indicator.
Sacral and gluteal cleft with diffuse blanchable erythema and partial thickness tissue breakdown.
What is moisture damage.
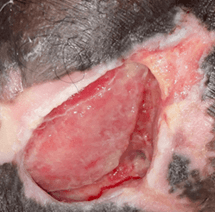
Goal of wound care and consult recommendation for a wound base that is gray and black with surrounding erythema.

What is debridement of dead tissue.
Options include topical treatment for debridement and/or surgical consult for debridement.
Newly dehisced surgical wound.
Contact covering provider, surgical service if applicable.
Chart flow when finding or assessing a wound.
What is a properly identified photo, an LDA created/updated, orders for treatment using the guidelines, and possibly a wound care consult placed.
Head to toe assessment should focus on these areas.
What is bony prominences ie occiput, elbows, sacrum/coccyx, heels, etc.
Oncoming report to next shift description for this wound.

Stage 4 pressure injury. Report wound characteristics such as tissue color, odor, and the presence of necrosis.