This is a type of leukemia associated with the t(15:17) translocation
Acute promyelocytic leukemia
A 37-year-old woman presents with episodic palpitations, diaphoresis, and severe hypertension. Her urine shows elevated levels of normetanephrine and metanephrine. She is found to have a mutation in the RET proto-oncogene. Which of the following best explains the cellular origin of her tumor and the mechanism of her symptoms?
A) Chromaffin cells derived from neural crest; increased catecholamine release
B) Zona glomerulosa cells; increased aldosterone synthesis
C) Follicular thyroid cells; increased thyroxine secretion
D) Adrenal cortical cells; increased cortisol production
E) Anterior pituitary cells; increased ACTH secretion
Answer:
A) Chromaffin cells derived from neural crest; increased catecholamine release
Explanation:
Pheochromocytomas arise from chromaffin cells in the adrenal medulla (neural crest origin) and cause symptoms via episodic catecholamine (epinephrine, norepinephrine) release.
Name the Charcot triad and associated disease
A 68-year-old man with advanced COPD is admitted for pneumonia. He previously completed an advance directive refusing intubation but now has altered mental status. His daughter insists on full resuscitation. Which action is most appropriate?
A) Follow the daughter’s request as the current decision-maker
B) Defer to the advance directive completed while the patient was competent
C) Initiate intubation pending ethics committee review
D) Request a psychiatric consult for the daughter
Answer: B) Defer to the advance directive completed while the patient was competent
Explanation: Competently executed advance directives legally override surrogate decisions unless new evidence suggests the patient changed their wishes.
A 25-year-old woman presents with unilateral vision loss and pain with eye movement. MRI reveals a demyelinating lesion in the optic nerve. Which histopathological finding is most characteristic of this condition?
A) Amyloid plaques
B) Neurofibrillary tangles
C) Perivascular lymphocytic infiltration
D) Lewy bodies
Answer: C) Perivascular lymphocytic infiltration
Explanation: Optic neuritis in MS involves perivascular T-cell and macrophage infiltration causing demyelination. Amyloid plaques (A) are seen in Alzheimer’s, neurofibrillary tangles (B) in tauopathies, and Lewy bodies (D) in Parkinson’s.
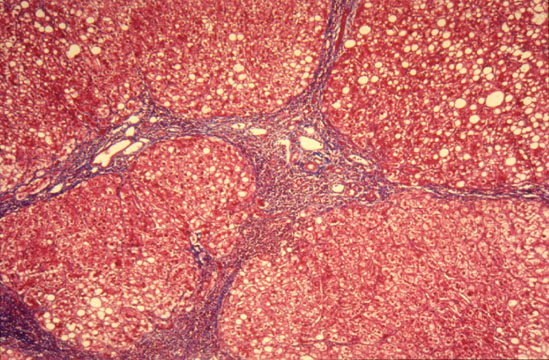 Condition in the liver that has a variety of causes and leads to this specific histological finding. Name the disease, one cause, and the name of the finding.
Condition in the liver that has a variety of causes and leads to this specific histological finding. Name the disease, one cause, and the name of the finding.
Cirrhosis, hepatitis, fibrosis
A 29-year-old man with chronic hepatitis B develops a liver mass. Biopsy confirms hepatocellular carcinoma. Which of the following best describes the pathophysiologic process by which hepatitis B virus increases the risk of cancer in this patient?
A) Integration of viral DNA
B) Direct cytotoxicity of hepatocytes by viral proteases
C) Autoimmune destruction of bile ducts
D) Overproduction of viral RNA leading to steatosis
E) Hepatic iron overload due to viral-induced hepcidin suppression
Answer:
A) Integration of viral DNA into host genome
Explanation:
HBV can integrate its DNA into the host genome, leading to insertional mutagenesis and increased risk of hepatocellular carcinoma.
what disease is characterized by NO suppression of cortisol production at low levels but suppression at high levels
Cushing disease
A 56-year-old man is admitted for mild community-acquired pneumonia. He is clinically stable, afebrile, and improving on antibiotics. His physician continues to order daily complete blood counts (CBC) and basic metabolic panels (BMP) each morning. After a week, his hemoglobin drops from 14 g/dL to 11 g/dL, and he expresses concern about feeling more tired. According to the Choosing Wisely initiative, what is the most appropriate action regarding his blood work?
A) Continue daily blood tests to monitor for unexpected complications
B) Discontinue routine daily blood tests unless clinically indicated
C) Switch to weekly blood tests for all hospitalized patients
D) Increase blood draws to include liver function tests
E) Transfuse packed red blood cells for the drop in hemoglobin
B) Discontinue routine daily blood tests unless clinically indicated
Explanation:
The Choosing Wisely initiative recommends against routine daily lab testing in stable hospitalized patients due to risks such as iatrogenic anemia and unnecessary healthcare costs. Blood tests should be ordered based on clinical indications, not as a standing daily order.
A 30-year-old man has two episodes of neurological deficits (optic neuritis and leg weakness) separated by 6 months, with full recovery after each. MRI shows periventricular and spinal cord lesions. Which MS subtype is most likely?
A) Primary progressive
B) Relapsing-remitting
C) Secondary progressive
D) Clinically isolated syndrome
Answer: B) Relapsing-remitting
Explanation: RRMS is defined by relapses with recovery. CIS (D) refers to a first episode without meeting MS criteria.
This condition is associated with metaplasia from one type of epithelium to another. Name the condition and the transition
Barrett's esophagus
Stratified squamous epithelium --> nonciliated columnar epithelium
A 72-year-old woman with a history of gallstones develops fever, jaundice, and confusion. Blood cultures grow Klebsiella pneumoniae. Which of the following best explains the pathogenesis of her condition?
A) Retrograde bacterial migration due to increased intrabiliary pressure from obstruction
B) Viral infection of hepatocytes causing ductal necrosis
C) Autoimmune T-cell mediated destruction of intrahepatic ducts
D) Ischemic injury to the gallbladder wall
E) Hematogenous spread of bacteria from the portal vein
Answer:
A) Retrograde bacterial migration due to increased intrabiliary pressure from obstruction
Explanation:
Obstruction (often from stones) increases pressure, allowing bacteria from the gut to ascend into the biliary tree, causing infection and sepsis.
Which blood cancer is associated with children, B symptoms, and pancytopenia? Name the cancer and the most common translocation
Acute Lymphoblastic Leukemia
t(12:21) translocation with B-cell ALL
A 47-year-old man with type 2 diabetes is prescribed a new GLP-1 agonist but is unable to afford the monthly cost. He has no prescription drug coverage and has already attempted to obtain the medication through his local pharmacy discount program without success. Which of the following is the most appropriate next step to help this patient obtain his medication?
A) Refer him to a pharmaceutical company’s patient assistance program
B) Advise him to purchase the medication from an online international pharmacy
C) Prescribe a less effective but cheaper alternative
D) Suggest he apply for Medicaid
E) Recommend he stop the medication due to cost concerns
Answer:
A) Refer him to a pharmaceutical company’s patient assistance program
Explanation:
Patient assistance programs (PAPs) are designed to help uninsured or underinsured patients obtain necessary medications at low or no cost, often through pharmaceutical manufacturers. This is the most appropriate and immediate option for patients struggling with medication affordability.
A 29-year-old woman presents with episodes of numbness and tingling in her right arm and left leg that resolve spontaneously. She also reports blurred vision in her right eye that lasted for several days and then improved. Neurologic examination is normal. MRI of the brain reveals multiple lesions in the periventricular white matter, some of which are oriented perpendicular to the lateral ventricles. Cerebrospinal fluid analysis shows an elevated IgG index and the presence of oligoclonal bands not found in the serum. Which of the following MRI findings is most specific for the diagnosis of multiple sclerosis?
A) Multiple small infarcts in the basal ganglia
B) Ovoid periventricular lesions radiating outward from the ventricles
C) Diffuse cortical atrophy
D) Ring-enhancing lesion in the temporal lobe
E) Symmetric hyperintensities in the thalamus
Answer:
B) Ovoid periventricular lesions radiating outward from the ventricles
Explanation:
These are known as Dawson’s fingers, which are highly specific for MS and represent demyelination along small veins in the periventricular white matter. The other options are not specific for MS.

These bodies represent dying hepatocytes due to apoptosis in a type of viral hepatitis. Name the bodies and the hepatitis.
Councilman bodies, hepatitis A
A 41-year-old man from rural Brazil presents with progressive dysphagia to both solids and liquids. Esophageal manometry shows increased lower esophageal sphincter (LES) pressure and absent peristalsis. Which of the following is the most likely underlying cause of his condition?
A) Destruction of myenteric plexus by Trypanosoma cruzi infection
B) Autoimmune targeting of parietal cells
C) Hyperplasia of smooth muscle in the LES
D) Chronic gastroesophageal reflux
E) Squamous cell carcinoma of the esophagus
Answer:
A) Destruction of myenteric plexus by Trypanosoma cruzi infection
Explanation:
Chagas disease (endemic in rural Brazil) causes secondary achalasia by destroying the myenteric plexus, leading to impaired LES relaxation and dysmotility.
5. Acute Stroke (Mechanistic Reasoning)
A 70-year-old man with a history of atrial fibrillation suddenly develops right-sided hemiplegia and aphasia. CT angiography reveals an occlusion in the left middle cerebral artery. Which of the following best explains the pathophysiology of his acute neurologic deficit?
A) Embolic occlusion of a cerebral artery by a thrombus originating in the left atrium
B) Intracerebral hemorrhage due to chronic hypertension
C) Microaneurysm rupture in the basal ganglia
D) Hypoxic-ischemic encephalopathy from global cerebral hypoperfusion
E) Vasospasm secondary to subarachnoid hemorrhage
Answer:
A) Embolic occlusion of a cerebral artery by a thrombus originating in the left atrium
Explanation:
Atrial fibrillation predisposes to thrombus formation in the left atrium, which can embolize to cerebral arteries, causing an acute ischemic stroke.
Which bleeding disorder is associated with normal platelet count, increased bleeding time, normal PT, possibly inc aPTT?
100 bonus points to name the results of one additional test that can be performed to diagnose this disease
Von Willebrand Disease
Bonus: ristocetin cofactor assay --> no agglutination
A 50-year-old woman with gastrointestinal bleeding requires a blood transfusion. She is concerned about the risk of contracting an infection from the transfusion. As her physician, you want to ensure she provides informed consent. Which of the following is the most appropriate way to address her concern during the consent process?
A) Assure her that modern blood screening has eliminated all risk of infectious disease transmission
B) Explain that, while the risk is extremely low due to rigorous screening, there remains a small chance of infection such as hepatitis B, hepatitis C, or HIV
C) Tell her that only non-infectious complications, such as allergic reactions, are possible with transfusion
D) Advise her that refusing transfusion is not an option if her hemoglobin drops below 7 g/dL
E) Reassure her that antibiotics are always given with transfusions to prevent infection
Answer:
B) Explain that, while the risk is extremely low due to rigorous screening, there remains a small chance of infection such as hepatitis B, hepatitis C, or HIV
Explanation:
Informed consent for blood transfusion requires disclosure of both the benefits and the potential risks, including the very small but real risk of infectious disease transmission, despite modern screening. Overstating safety or omitting this information would be inappropriate.
A 42-year-old woman with a 12-year history of relapsing-remitting multiple sclerosis now reports gradually worsening lower limb weakness and difficulty with balance for the past year, without any clear relapses. MRI of the brain shows extensive areas of hypointensity on T1-weighted images ("black holes") but no new gadolinium-enhancing lesions. Which of the following best explains this patient’s current disease progression?
A) Acute inflammatory demyelination
B) Chronic axonal degeneration
C) Amyloid plaque deposition
D) Acute ischemic infarction
E) Peripheral nerve demyelination
Answer:
B) Chronic axonal degeneration
Explanation:
Progressive worsening in MS, especially in the absence of new relapses or enhancing lesions, is due to chronic axonal degeneration and neurodegeneration, as evidenced by T1 "black holes" on MRI.
%2Fcase%2Fdetail_images%2Fc8710_detail.jpg&w=1920&q=75)
This tumor has polygonal or spindle cells arranged in small nests. Name that tumor.
100 Bonus Points if you know the name of the small nests
Pheochromocytoma
Bonus: Zellballen nests
A 65-year-old woman with a history of poorly controlled hypertension and diabetes mellitus is brought to the emergency department after being found unresponsive. On arrival, her blood pressure is 210/110 mmHg. Neurologic examination reveals left-sided hemiplegia and gaze deviation to the right. Non-contrast CT of the head shows a hyperdense area in the right basal ganglia with surrounding hypodensity and midline shift. Which of the following best explains the primary pathophysiologic mechanism leading to her current condition?
A) Lipohyalinosis and rupture of small penetrating arteries
B) Embolic occlusion of the right middle cerebral artery
C) Global cerebral hypoperfusion due to cardiac arrest
D) Vasospasm following subarachnoid hemorrhage
E) Amyloid deposition in cortical blood vessels
Answer:
A) Lipohyalinosis and rupture of small penetrating arteries
Explanation:
Chronic hypertension leads to hyaline arteriolosclerosis (lipohyalinosis) of small penetrating arteries, especially in the basal ganglia, thalamus, and pons. This predisposes to intracerebral hemorrhage (as seen on CT), resulting in acute neurologic deficits and mass effect. The clinical context and imaging findings are classic for hypertensive hemorrhagic stroke.
1. adenocarcinoma is in the lower 1/3 while SCC is upper 2/3
2. adenocarcinoma most common in america, SCC most common worldwide
3. adenocarcinoma associated with barrett's
A 64-year-old Black man presents to the emergency department with sudden right-sided weakness and aphasia that started 1 hour ago. He is diagnosed with acute ischemic stroke. Compared to his White counterparts, which of the following disparities is he most likely to experience regarding his acute stroke care and secondary prevention, and what is the most effective strategy to address this disparity?
A) Increased likelihood of receiving endovascular therapy; address with more public stroke awareness campaigns
B) Delayed receipt of thrombolytic therapy; address with regional stroke systems and anti-bias training for emergency staff
C) Higher rates of post-stroke rehabilitation; address with increased funding for tertiary care hospitals
D) Lower risk of recurrent stroke; address with culturally tailored community programs
E) More frequent prescription of statins at discharge; address with language translation services
B) Delayed receipt of thrombolytic therapy; address with regional stroke systems and anti-bias training for emergency staff
Explanation:
Black and Hispanic patients are less likely to receive timely acute stroke interventions such as thrombolysis or endovascular therapy, often due to systemic inequities, hospital resources, and implicit bias. Effective strategies include establishing regional stroke systems to ensure equitable access to specialized care and providing anti-bias training for emergency department staff to improve triage and treatment times.
A 35-year-old with MS reports electric shock-like sensations down the spine upon neck flexion. Which spinal tract is most likely affected?
A) Spinothalamic tract
B) Dorsal columns
C) Corticospinal tract
D) Spinocerebellar tract
Answer: B) Dorsal columns
Explanation: Lhermitte’s sign (neck flexion-induced shocks) arises from demyelination in the dorsal columns. Spinothalamic (A) lesions cause pain/temperature loss; corticospinal (C) lesions cause spasticity.