What is the numerical definition of hypotension?
BP < 90/60
...but clinical context is important! Think symptoms, baseline BP, trend, etc
What are some physical exam findings for hypotension? At least 3
Neuro: AMS
Cardiac: tachycardia, poor capillary refill, dry axilla
GI: postprandial cramping
Extremities: dry skin, cool extremities, pale, dry mucous membranes
Name the 4 classes of shock
1. Obstructive
2. Cardiogenic
3. Hypovolemic
4. Distributive
A 42-year-old male presents to the emergency department with a 3-day history of vomiting and profuse watery diarrhea. He has been unable to keep any fluids down due to repeated vomiting. Over the past 24 hours, he has noticed that his urine output has decreased, and he feels more weak and lightheaded.
Vitals: HR 110, BP 90/60
Labs: Na 132, K 3.2, Cl 98, bicarb 20, Cr 1.2
Physical Exam: alert, dry mucous membranes, tachycardic, diffuse abdominal exam
What is the primary cause of his hypotension?
Hypovolemia likely 2/2 GI losses (vomiting diarrhea)
Will often see electrolyte abnormalities like a metabolic acidosis (low bicarb), low Na, low K, low Cl.
Tx: IV fluids, electrolyte repletion
What is this position called?
Trendelenburg
It increases pre-load by increasing venous return to the heart.
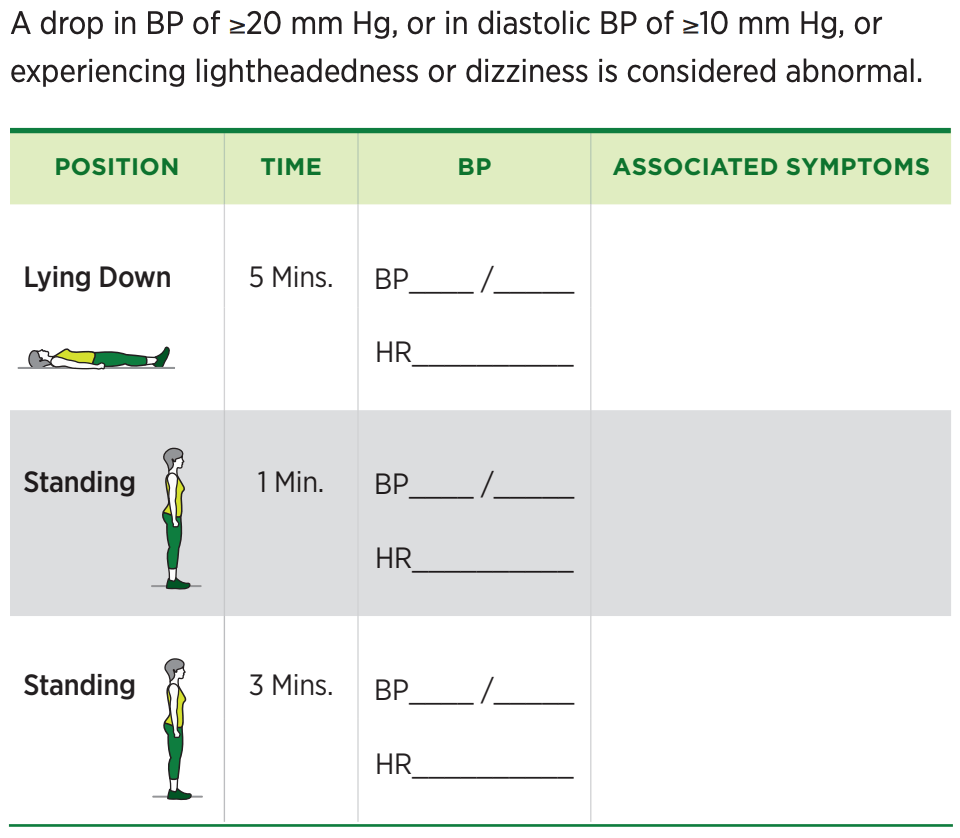
What is the BP definition of orthostatic hypotension?
What are some lab findings in a patient with hypotension?
Elevated lactate (>2)
Increasing LFTs (first to show)
AKI
Low Hgb if bleeding
Low K, Cl with GI losses
Hemoconcentration (increased Hgb, platelets, WBC)
What are examples of distributive shock? At least 2
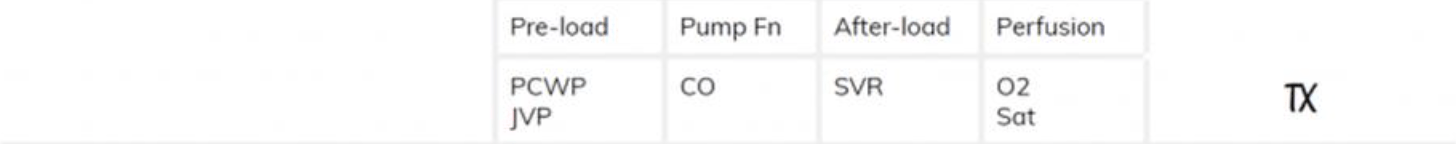
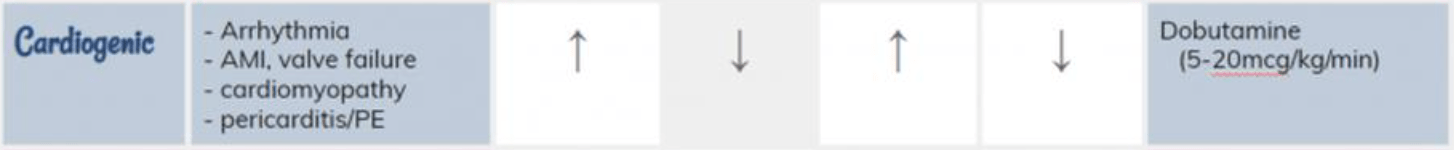
In distributive shock, what happens to the preload, cardiac output, afterload (SVR)?
- Septic, neurogenic, anaphylaxis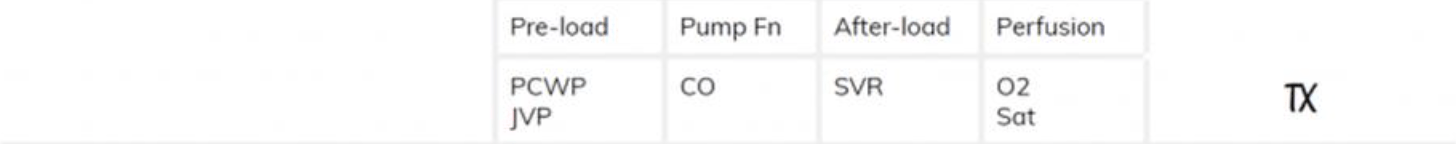

A 65-year-old male PMH T2 diabetes, HTN, and CKD presents to the emergency department with a 2-day history of fever, chills, and productive cough. He also reports increasing shortness of breath and fatigue over the past 24 hours. The patient has not been eating or drinking well, and his urine output has decreased.
Vitals: 102.5°F, HR 120, BP 90/60, RR 24, O2 90% on RA
Labs: WBC 18, Lactate 6, Cr 2.5
Imaging: CXR lobar consolidation
Septic shock 2/2 pneumonia.
Note the AKI (Cr 2.5), elevated lactate (poor organ perfusion), WBC 18, CXR findings
Tx: IVF, antibiotics
Which steroid is recommended in the management of Adrenal Insufficiency?
IV hydrocortisone
What is the BP cutoff in the SIRS criteria? In qSOFA?
SIRS: NO BP COMPONENT
qSOFA: SBP < 100
qSOFA has higher specificity while SIRS has higher sensitivity to shock. SIRS identifies signs of shock earlier than qSOFA, but qSOFA is a better predictor of organ dysfunction & mortality.
Describe the role of A1, B1, and B2 on blood pressure regulation.

What are examples of hypovolemic shock? At least 2
In hypovolemic shock, what happens to the preload, cardiac output, afterload (SVR)?
- Bleed, dehydration, burns, third spacing, protein loss, vomiting, diarrhea

A 72-year-old female with PMH HTN, Type 2 DM presents to the emergency department with complaints of dizziness, fatigue, and lightheadedness upon standing. She states that her symptoms started 2 days ago, progressively worsening, and has been feeling increasingly weak. Her daughter brought her in after she noticed her mother appeared confused and more lethargic than usual. Was just discharged one week ago for HF exacerbation and started on Lasix.
Vitals: HR 95, BP 90/60 otherwise normal
Labs: normal
Physical Exam: pleasantly confused, dry membranes, + orthostatics
Hypotension from medication confusion.
It is SO important to do a med rec with a patient and their family and ask them how frequently they were taking the medication, what dose they have at home, and when their last dose was.
You respond to an RRT for hypotension in a patient with cirrhosis. You determine they are not in shock or unstable, what fluid would you recommend for volume resuscitation and why?
Albumin to increase oncotic pressure
What is the IVF resuscitation rate in sepsis?
30 cc/kg
Ex: 100kg patient = 3L IVF
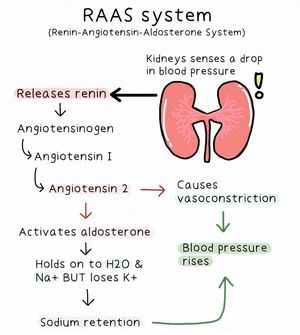
Draw/describe the RAAS pathway, and describe how aldosterone and angiotensin 2 increase BP.
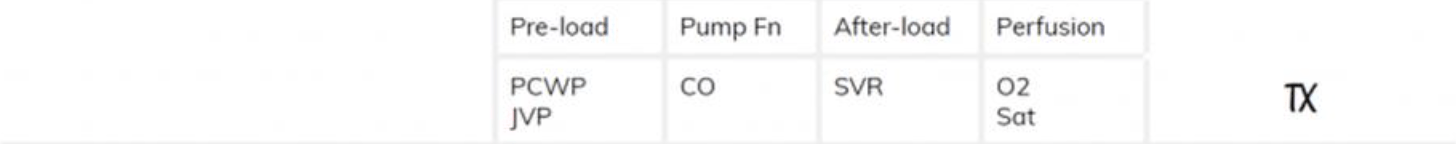
What are examples of cardiogenic shock? At least 2
In cardiogenic shock, what happens to the preload, cardiac output, afterload (SVR)?
- MI, arrhythmia, valve disorders, pericardial effusion, pericarditis
A 24-year-old female with no PMH presents to the emergency department after fainting at work. She reports feeling lightheaded and nauseous for a few minutes before suddenly losing consciousness while standing in line at the coffee machine. Her co-workers found her lying on the floor, and she regained consciousness within a minute. She denies any chest pain, shortness of breath, or headache. She felt weak and slightly dizzy but did not sustain any injury from the fall.
Vitals: BP 90/60 otherwise normal
Labs: normal
Physical Exam: alert, normal rate/rhythm, clear breath sounds, abdomen soft nontender nondistended, good capillary refill
Hypotension from vasovagal syncope.
Keys: preceding lightheadedness, nausea, symptoms. Often from standing too long or emotional stress.
Tx: symptomatic
Explain how norepinephrine works and what shock is it used for?
Septic shock
A1 and B1 agonist (vasoconstriction helps counteract the vasodilation)
First line, AKA "levo"
What is the 30 day hospital mortality for septic shock?
~40%

Spell out the name of this device. Starts with an S...
Sphygmomanometer
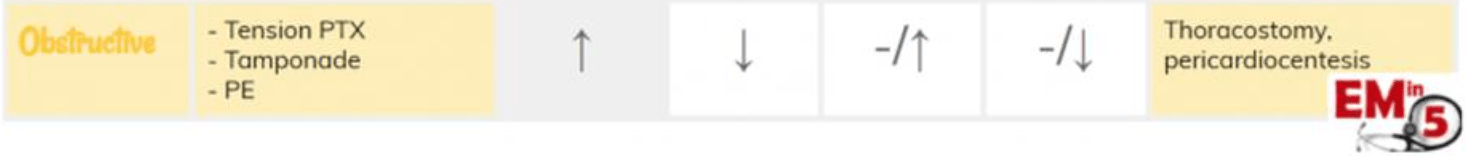
What are examples of obstructive shock? At least 2
In obstructive shock, what happens to the preload, cardiac output, afterload (SVR)?
- PE, tension pneumothorax, constrictive pericarditis, tamponade, SVC syndrome
A 58-year-old female with PMH HTN and T2 DM is admitted to the hospital with community-acquired pneumonia. She is started on empiric antibiotics. Her vital signs are stable on admission, and she is initially treated with fluids and fever-reducing medications.
On day 3 of hospitalization, the patient develops fever, tachycardia, and hypotension despite adequate fluid resuscitation and antibiotics. She is becoming more lethargic and reports feeling weak and nauseous. Her blood pressure is 85/50 mmHg, and she is now requiring increased oxygen support.
Labs: Na 130, K 5.6, Cl 100, bicarb 18, glucose 140, Cr 1
Acute adrenal insufficiency leading to hypotension.
Can often be triggered by infection, stress, prolonged hospitalization. Would expect low cortisol (<3), low Na, and high K.
Treatment: IV steroids
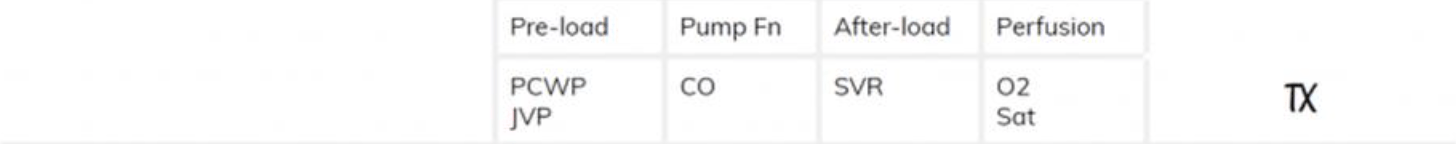
Explain how milrinone and/or dobutamine work. What shock type do they treat?
Cardiogenic shock
Milrinone: PDE3 inhibitor that inhibits cAMP breakdown --> increases intracellular Ca --> increases myocardial contractility. Also has significant vasodilatory effects (more than dobutamine)
Dobutamine: B1>B2, increases contractility