7yo female presents with 3 days of cough, rhinorrhea, and congestion. Mom states she feels warm, and is coughing all the time. Some classmates were sent home with fever this week.
Vitals: 99.2F, HR 91, RR 20, 97%
On exam, ears are normal, pharynx with cobblestoneing, mild nasal turbinate swelling, shotty bilateral anterior cervical adenopathy, lungs are clear, and heart sounds normal.
Viral URI
Treatment?
Sore throat: Cepacol lozenges/Zarbees drops or salt-water gargle
Congestion: Flonase, Ceterizine/Levocitrizine, Netti pot, saline spray, humidified air
Cough: Warm fluids, OTC cough aids, honey, lozenges
Fever: IBU/APAP alternating or take together pending age
38yo female with no PMH, presents for 2 mths of cough. She felt ill at the beginning with cough and congestion. The congestion and body aches has resolved but the cough has persisted. She is tired of coughing and wants to know what is going on. OTC medications aren't helping.
What is this?
Post viral cough syndrome
Can last up to 8-12weeks after infection
Treat with supportive care82yo female with PMH of HTN, CAD, DM, seasonal allergies, and COPD, presents to clinic because her legs have become more swollen recently and started coughing about a week ago. She has difficulty putting on her socks and gets winded easily walking from her bedroom to her kitchen. She takes all her medications as prescribed.
She has a non-productive cough on exam and bilateral pitting edema.
CXR in clinic shows mild perihilar vascular congestion and small left effusion.
What does she have?
New onset heart failure
Cough comes from irritation of the lungs from congestion.
ECHO, GDMT, Diuretics
43yo female with morbid obesity, HTN, DM, and sleep apnea, presents to clinic with a periodic cough for the last 3 months. Her fav foods are fried, drinks 2 cups of coffee every morning, and doesnt like exercise. Her HTN has been controlled on Lisinopril 20mg and Amlodipine 5mg for the last 3 years. She wants to know why she cant stop coughing. Exam is benign.
What is the most likely diagnosis?
GERD
Treatment?
PPI: Omeprazole or Pantoprazole 20mg qD for 8 weeks, then reevaluate
H2 receptor blocker: Famotidine 20mg qD for 8 weeks, then reevaluate
Budesonide + Formoterol
Tiotropium
Symbicort
Spiriva
22yo male with PMH of eczema presents to clinic for productive cough over the last 2 mths since it started getting warm. He has clear drainage from his nose. Patient denies fever, but endorses itchy throat/eyes and fullness in his ears.
What is the best treatment?
Intranasal Glucocorticoids (Allergic rhinitis)
Can take up to 2 weeks to achieve maximal effect
Other option? Antihistamines: 1st gen work better for anticholinergic effect, but, are more sedating
1st gen Brompheniramine, Chlorpheniramine, Clemastine, Doxylamine
2nd gen: Cetirizine, Loratadine, Fexofenadine
48yo male with PMH of 10pack-years, comes to clinic because she hasn't stopped coughing over the lasts year. She remembers having a cold ~2 years ago and started coughing intermittently then. Her coughing starts to limit her with walking stairs. She has tried OTC meds with no relief and is annoyed with the coughing. On exam she has mild expiratory wheeze.
She has no prior spirometry. Her CAT score is 11.
What is 1st line therapy?
LABA+LAMA and PRN Albuterol
- Anoro Elipta, Stiolto
She is class B by gold guidelines.
Remember an LABA+ICS is not treatment for COPD.
3yo male with PMH of autism, presents with sudden onset malaise, poor appetite, and fever. Tmax at home of 103.7F. Mom has been treating with alternating IBU/APAP. Sitting in clinic he is irritable and says he hurts. Mom wants to know if there is a test for his illness
Vitals: T 102.F, HR 123, RR 22, 100%O2, 21.7kg
What is his medication dose?Tamiflu (Oseltamivir) BID x5days
<1yo, 3mg/kg
<15kg: 30mg
15.1-23kg: 45mg
23.1-40kg: 60mg
>40kg: 75mg
14yo male with PMH of asthma, presents complaining of cough when he is outside playing soccer and has to take his albuterol more than he used to. He currently takes a low dose advair. He has no recent illnesses, doesnt take allergy medications. His mom says she can hear him coughing at night sometimes.
On exam he has mild end expiratory wheeze.
What is wrong with him?
Uncontrolled Asthma
Control is determined by:
Day time symptoms, Night time symptoms, Albuterol use, Disability
Omeprazole
Pantoprazole
Famotidine
Prilosec - Omeprazole
Protonix - Pantoprazole
Pepcid - Famotidine
76yo male with PMH of 35pack years and DM, comes to clinic with audible wheezing and increased light green sputum production. He also endorses fever, rhinorrhea, congestion, and body aches. He looks like he is breathing heavy and is speaking in broken sentences.
Vitals: T 99.6F, HR 80, BP 143/87, RR 23, SpO2 91%
How do you treat this illness?
Albuterol and steroids (COPD exacerbation)
16yo male, fully immunized, is brought to clinic by his dad because teachers are complaining his cough is distracting in class. For the past 2 months the patient will cough multiple times intermittently throughout the day, sometimes with mucus production or barky quality.
He has no congestion, rhinorrhea, body achesm fever, sinus pain, or allergies. He has never had asthma or needed an inhaler.
His dad says that his son started doing this toward the beginning of summer after they moved to a new city, but never hears it at night. They have tried OTC meds with no relief.
What is this?
Psychogenic cough, Habit Cough, Somatic Cough Syndrome
A diagnosis of exclusion; refractory to medical management and considered to have a psychiatric or psychological basis.
Treat with CBT
5yo female with no PMH, is brought to UCC on a Saturday by her mother for 3 days of coughing with a barking quality. She also has rhinorrhea, congestion, and noisy breathing. There is no fever the mother has measured.
Vitals: T 99.2F, HR 108, RR 48, 92%O2.
There is clear auditory inspiratory stidor at rest and intercostals and substernal retractions on exam.
What should you do?
CROUP
Decadron 0.6mg/kg PO once, racemic epi, and moitoring.
-If stridor continues, then admit to peds and start O2 for WOB.
-If stridor resolves and RR improves, then can dc home with return precautions
58yo male with PMH of HTN and HLD presents for intermittent cough, morning headache, and chronic fatigue. His wife made him come in; "She told me I have breathing issues". The patient isnt obese, but has a thick neck. Exam is otherwise benign.
What is his STOPBANG score?
STOP-BANG score: >3 = risk and should get sleep study
- Snoring - Apnea - HTN txt - Age >50
- Male - BMI >35kg/m2 - neck circ >40cm
- Tired/Fatigued/Sleepy during day
Omnicef
Vibramycin
Maxipime
Omnicef - Cefdinir
Vibramycin - Doxycycline
Maxipime - Cefepime
46yo male presents to urgent care complaining of a headache, and upper jaw tooth pain for 3 days. He has tried IBU and APAP at home hoping the pain would go away. She has an appt with her dentist next week but doesn't feel like she can wait that long. She had subjective fever, questionable congestion, and cough, but no rhinorrhea or body aches. Transillumination of her right maxillary sinus is abnormal.
How do you treat?
Conservative management (Acute sinusitis)
The abnormal transillumination of her sinus points toward inflammation and fluid build up in the sinus cavity. After only 3 days there it is most likely viral. Cough is response to increased mucus production and post-nasal drip.
What does she have?
Occupational Asthma
Occupational exposures can cause hypersensitivity responses leading to rhinitis and upper airway cough syndrome; as well as asthma HP, chronic beryllium disease, and hard metal disease
Cement, Construction workers, Farming and food industry, Wood industry, Chemicals, Mines
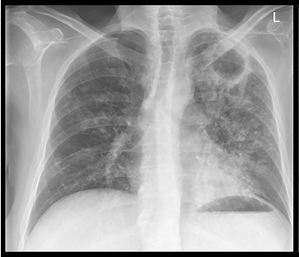
73yo male with no PMH comes to clinic with complaint of fever and SOB/cough. He has intermittent lower right chest pain, and poor appetite for 3 days, but otherwise is okay. Denies N/V/D or abd pain. He is not confused. On exam he is mildly tachycardic, tachypneic, SpO2 is 91%, has no WOB, but does have some RLL consolidation on egophany testing. CXR ordered in clinic.
What is his CURB65? What is treatment dose?
Community Acquired Pneumonia
No comorbidities or risk factors for MRSA or Pseudomonas:
Amoxicillin 1g TID or Doxy 100mg BID or Azithro 500mg x1/250mg x4
With comorbidities:
Augmentin 875/125mg BID or Vantin 200mg BID, Zinacef 500mg BID
PLUS
Azithro 500/250 or Doxy 100mg BID
OR monotherapy with Levaquin 750 qD, Moxi 400mg qD, Gemi 320mg qD
Traditional bug: S pneumo, H flu, M Pneumo, S aureus, Legionella, C Pneumo, M catarrhalis
Use CURB-65 (confusion, uremia, respiratory rate, blood pressure, >65 yo) or Pneumonia Severity Index (PSI) for hospitalization determination
68yo male with PMH of HTN comes in for evaluation of cough for the past 4 months. About 1 year ago he was started on Prinzide and is now taking 40-25mg once per day. His blood pressure has been stable. He has no SOB, chest pain, fever, rhinorrhea, wheeze, or reflux.
How do you treat his cough?
Discontinue ACEi (ACEi Cough)
Discontinuing therapy usually resolves the cough 1 to 4 days after, but it can be prolonged for up to a months
Common side effects: dry cough, hyperkalemia, hypotension, increased BUN and Cr, syncope, angioedema. Patients report dry cough between the one week of initiation and up to six months. Some sources cite up to one year after initiation.
ACE metabolizes bradykinin and other local molecules. Inhibiting ACE in the lung increases the concentration of kinins, causing bronchial irritation.
Acetaminophen + Chlorpheniramine + Dextromethorphan
Coricidin
86yo female with PMH of dementia, DM, HTN, is brought to the ED from her nursing home because she has seem more lethargic than normal. Her aid reported having to change her bed linens more often. Patient looks ill, and coughs during the exam. She is plesantly demented and unable to contribute to the HPI.
Patient is well known in the community for her missionary work when younger.
Vitals: T 102F, HR 101, BP 102/62, RR 20, SpO2 88%
How do you test?, and how do you treat?
Tuberculosis
Sputum collection x3 (q8hr or q24h pending protocol) for AFB smear microscopy and culture
RIPE: Rifampin, Isoniazid, Pyrazinamide, Ethambutol
TB treatment regimens consists of two phases: an intensive phase (administration of four drugs for two months) followed by a continuation phase (administration of two or three drugs for two to seven months
--> UPTODATE HAS DOSING
18mo male is brought to UCC by his nanny for excessive coughing. The patient's parents are on an anniversary cruise and cannot be reached. The nanny states for the last 3 days the toddler has been coughing non-stop and seems to lose his breath at the end. He had a fever 2 weeks ago. This morning he couldnt keep down breakfast.
The nanny thinks he is UTD on vaccines but the parents are ecclectic and no records can be found.
The patient has a harsh cough during exam and has a sharp inhale after coughing profusely. Lung sounds are course, and he has classic URI findings.
How do you treat?
Azithromycin 10mg/kg q24h for 5 days, max 500mg per dose.
Clarithromycin x7 days
Bactrim x14days
4yo male with no PMH, is in the ED with CC of "it sounds like he cant breath". Child is adopted, immunization hx is unknown. Mom says he has had trouble drinking for last few hours.
Patient is sitting on the stretcher drooling slightly, has moderate inspiratory stridor, is tachycardic, tachypneic, and has some retractions. Periodically he clears his throat and coughs. Nothing is visible in his mouth.
What urgently needs to happen?
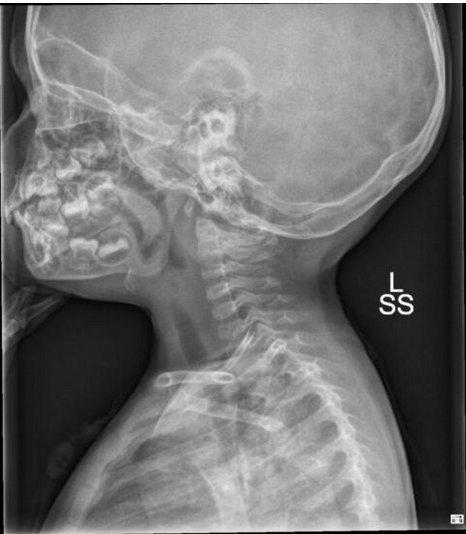
Acute Epiglottitis
Intubation in the OR, ENT consult, PICU admission, antibiotics
88yo male with PMH of Graves is brought to the clinic by his daughter/caregiver saying that he seems to cough or gag after every meal. Daughter states he eats without difficulty but will spend the next hour acting like something is stuck in his throat. He can drink a glass of water after and still have coughing. On exam pharynx is clear, lungs are clear, and thyroid size is normal.
Vitals: T 101F, HR 96, BP 98/58, 94%O2
You order a CXR due to his vitals.
What do you do for this man
Admit to hospital and treat for symptomatic aspiraton PNA
Usually, will need a video fluorographic swallowing study (barium swallow), manometry, or endoscopy.
Swallowing disorders are common in the elderly These disorders can occur due to structural or functional problems
Oral/Pharyngeal phase: coughing/choking with swallowing, difficulty initiating swallowing, change in voice, nasal regurg
Esophageal phase: globus sensation, oral/pharynx regurg
Either phase: food sticking in throat, drooling, weight loss, change in dietary habits, recurrent pna
Zestril
Diovan
Hyzaar
Zestril - Lisinopril
Diovan - Valsartan
Hyzaar - Losartan-HCTZ