A 30-year-old man is hospitalized for sudden onset of severe left biceps swelling and pain beginning 36 hours ago, which has rapidly progressed in the past 6 hours. He also reports fever and chills. Medical history is significant for daily subcutaneous (“skin popping”) heroin use into the left biceps. He takes no medications.
On physical examination, temperature is 38.7 °C (101.7 °F), blood pressure is 110/60 mm Hg, pulse rate is 110/min, and respiration rate is 24/min. The left biceps area is exquisitely tender, with associated edema, warmth, and overlying ecchymotic bullous lesions; crepitus and induration are appreciated with palpation.
CT imaging reveals gas in deep tissues.
Piperacillin-tazobactam and vancomycin are initiated, and the patient is taken for surgical debridement where necrotizing fasciitis and myonecrosis are confirmed; subsequent cultures identify Clostridium perfringens.
What is the most appropriate antibiotic treatment?
Penicillin plus clindamycin
Ceftazidime plus doxycycline
Ciprofloxacin plus doxycycline
Current antibiotics
A 35-year-old man is evaluated for recurrent sinus infections. He indicates experiencing sinus infections lasting more than 2 weeks requiring antibiotics one to two times per year for the past 10 years. He reports frequent episodes of bronchitis and has been hospitalized twice for pneumonia. Two years ago, he was diagnosed with giardiasis. He takes no medications.
On physical examination, vital signs are normal. The examination is unremarkable.
Laboratory studies show a quantitative IgG level of less than 500 mg/dL (5 g/L) and a normal complete blood count with differential.
What is the most appropriate management?
Serologic response to pneumococcal and tetanus vaccination
CD4 T-cell subset measurement
Booster measles vaccination
IgG subset (IgG 1-4 levels) measurement
Trimethoprim-sulfamethoxazole prophylaxis
A 24-year-old woman is hospitalized for increasing shortness of breath, fatigue, productive cough, and pleuritic chest pain of 2 weeks' duration; she has also been experiencing fever and chills for the past month. She has rheumatoid arthritis diagnosed 4 years ago. She lives in northern Georgia. Her medications are methotrexate, etanercept, low-dose prednisone, and ibuprofen as needed.
On physical examination, temperature is 39.2 °C (102.6 °F), blood pressure is 125/60 mm Hg, pulse rate is 128/min, and respiration rate is 26/min. Bilateral crackles are heard in the lungs. Abdominal examination reveals hepatosplenomegaly. Minimal synovitis is present in the wrists and metacarpophalangeal joints bilaterally.
Laboratory studies show a hemoglobin level of 7.5 g/dL (75 g/L), leukocyte count of 4500/µL (4.5 × 109/L), and platelet count of 50,000/µL (50 × 109/L).
Chest radiograph shows bilateral reticulonodular infiltrates.
Blood cultures are negative. Peripheral blood smear is shown.

The Histoplasma urinary antigen assay is positive.
What is the most appropriate treatment?
Liposomal amphotericin B
Fluconazole
Itraconazole
Posaconazole
An 81-year-old man is evaluated in the emergency department for confusion, fever, and shaking chills overnight. He has had increasing difficulty in fully emptying his bladder, urinary frequency, and dysuria for the past 3 days. He received a 7-day course of ciprofloxacin 1 month ago for cystitis with documented pyuria and bacteriuria. Medical history is also significant for benign prostatic hyperplasia.
On physical examination, he is disoriented to the date. Temperature is 38.9 °C (102 °F), blood pressure is 96/60 mm Hg, pulse rate is 102/min, and respiration rate is 20/min. The bladder is distended, but no costovertebral angle tenderness is elicited.
A dipstick urinalysis shows 2+ blood; 3+ nitrites; and 3+ leukocyte esterase.
What is the most appropriate intravenous treatment?
Ceftriaxone
Ampicillin
Cefepime and doxycycline
Levofloxacin
A 62-year-old man is evaluated in the emergency department for progressively worsening lower back pain of 3 weeks' duration. He reports no extremity numbness, weakness, or radicular pain. Medical history is notable for hypertension, type 2 diabetes mellitus, and hemodialysis for end-stage kidney disease. Medications are amlodipine, metoprolol, basal and prandial insulin, sevelamer, and a multivitamin.
On physical examination, temperature is 37.8 °C (100.1 °F), blood pressure is 150/90 mm Hg, pulse rate is 72/min, and respiration rate is 16/min. Neurologic examination is normal. A functioning right arm fistula is present. Point tenderness is noted over the lower lumbar spine.
Laboratory studies show a leukocyte count of 14,200/µL (14.2 × 109/L). Two sets of blood cultures obtained yesterday are positive for gram-positive cocci in clusters; preliminary identification is coagulase-positive staphylococci.
MRI of the thoracic and lumbar spine is shown.

What is the most appropriate initial management?
Vancomycin
Bone biopsy
Cefazolin
Vancomycin and cefepime
A 78-year-old man was hospitalized 2 days ago for management of lower back pain that has been worsening over the past 4 weeks and remained uncontrolled with oral pain medications. He reports no radicular symptoms, weakness, or bladder or bowel incontinence. Medical history is notable for benign prostatic hyperplasia treated with tamsulosin.
On physical examination, the patient appears in distress from pain. Temperature is 37.9 °C (100.2 °F), blood pressure is 155/85 mm Hg, pulse rate is 82/min, and respiration rate is 18/min. Tenderness to palpation is elicited over the lower lumbar spine. Lower extremity strength is normal, with intact sensation and normal reflexes.
Laboratory studies show a hemoglobin level of 12.2 g/dL (122 g/L) and leukocyte count of 15,600/µL (15.6 × 109/L).
MRI with contrast reveals evidence of L3-L4 discitis with osteomyelitis involving the contiguous vertebral body end plates at L3 and L4, without evidence of epidural abscess.
Blood and urine cultures are negative at 48 hours.
What is the most appropriate management?
Disk space aspiration/biopsy
Open bone biopsy
Vancomycin
Vancomycin and ceftriaxone
A 24-year-old woman is evaluated for a 6-week history of weight loss, fever, night sweats, and productive cough, with recently increasing malaise and fatigue. She works in a state prison. She takes no medications.
On physical examination, temperature is 38.6 °C (101.5 °F); other vital signs are normal. Pulmonary examination reveals bronchial breath sounds bilaterally over the posterior upper lung lobes.
Chest radiograph shows a small cavity with infiltrates in the right and left upper lobes and hilar lymphadenopathy.
Sputum acid-fast bacilli stain is shown. Sputum culture is pending.
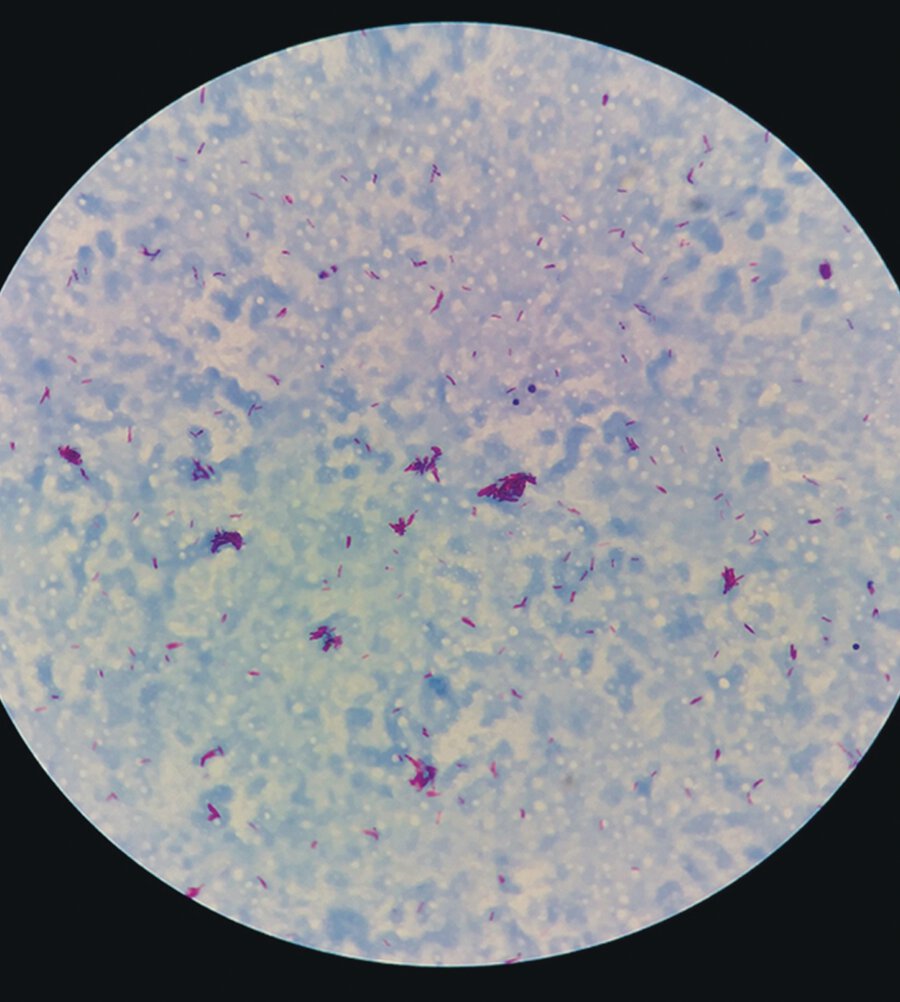
What is the most appropriate initial treatment?
Isoniazid, rifampin, pyrazinamide, and ethambutol
Clarithromycin and ethambutol
Isoniazid
Rifampin, ethambutol, pyrazinamide, and levofloxacin
A 72-year-old man is hospitalized for dyspnea, night sweats, and productive cough; symptoms began 8 months ago. He also reports a 9.1-kg (20 lb) weight loss over the past 12 months. Medical history is notable for COPD. He has a 60-pack-year smoking history. Medications are umeclidinium and vilanterol inhaler once daily.
On physical examination, vital signs are normal. Pulmonary examination reveals diminished breath sounds. The remainder of the examination is normal.
Sputum Gram stain shows abundant polymorphonuclear cells but no organisms. Sputum acid-fast bacilli stains are positive. Nucleic acid amplification testing for Mycobacterium tuberculosis is negative.
A chest radiograph is shown.

What is the most likely causative organism?
Mycobacterium avium complex
Mycobacterium marinum
Mycobacterium tuberculosis
Streptococcus pneumoniae
A 43-year-old man is hospitalized for shortness of breath, tingling in the extremities, and weakness. Three weeks ago, he had watery diarrhea that lasted 5 days. He reports no travel and no sexual contact in the past year. He takes no medications.
On physical examination, temperature is 37.2 °C (98.9 °F), blood pressure is 140/90 mm Hg, pulse rate is 101/min, and respiration rate is 22/min. Oxygen saturation is 93% breathing ambient air. Neurologic examination reveals no movement in the lower extremities and only 3/5 upper extremity strength bilaterally. Diminished or absent deep tendon reflexes are present throughout. Sensory examination is intact. Lung sounds are diminished, with poor inspiratory effort.
What is the most likely cause of this patient's neurologic syndrome?
Campylobacter infection
Botulism
West Nile virus infection
Zika virus infection
A 26-year-old woman undergoes consultation to update her vaccinations. She is an elementary school teacher. Medical history is significant for well-controlled HIV diagnosed 6 years ago. Medications are tenofovir alafenamide, emtricitabine, and dolutegravir.
The physical examination is normal.
Her CD4 cell count is 520/µL and has been stable for several years. HIV viral load is undetectable.
Which vaccines is contraindicated in this patient?
No contraindications exist
Human papillomavirus
Inactivated influenza
Measles-mumps-rubella
Varicella
A 46-year-old woman is evaluated in the emergency department for a 2-day history of fever. She is also experiencing tenderness at the laparoscopy site for a cholecystectomy performed 9 days ago. Medical history is otherwise noncontributory, and she takes no medications.
On physical examination, temperature is 38.3 °C (101 °F); the remainder of the vital signs are normal. She has moderate tenderness and fullness in the right upper quadrant with deep palpation. Minimal clear drainage is seen from one of the incision sites, but no erythema or tenderness is noted.
Laboratory studies show a leukocyte count of 14,300/µL (14.3 × 109/L).
What is the most appropriate next step?
Abdominal CT
Cephalexin
Gram stain and culture of incision site drainage
Piperacillin-tazobactam
A 32-year-old woman undergoes consultation for recurrent symptomatic lower urinary tract infections. They have increased in frequency over the past 3 years to a rate of about two times per year. She has been unable to relate onset to any specific activity. Symptoms resolve quickly with initiation of prescribed antibiotics. She is otherwise well.
What is the most appropriate management?
Self-treatment with nitrofurantoin
Daily cranberry tablets
Daily D-mannose supplementation
Nightly prophylaxis with low-dose ciprofloxacin
A 35-year-old man is evaluated for potential anthrax exposure. He was informed that three coworkers with whom he has had no close contact are being evaluated for suspected anthrax. Medical history is notable for a torn Achilles tendon that was repaired 9 months ago. He takes no medications.
On physical examination, vital signs are normal, and the examination is unremarkable.
A chest radiograph is normal.
What is the most appropriate management?
Doxycycline and anthrax vaccination
Ciprofloxacin and raxibacumab
Doxycycline, meropenem, ciprofloxacin, and raxibacumab
Isolation
Clinical observation
A 24-year-old woman is evaluated for HIV pre-exposure prophylaxis. She shares needles and other equipment for injection drug use. She has one sexual partner who is HIV negative; she uses condoms regularly.
Vital signs and physical examination are normal.
Laboratory studies:
Fourth-generation HIV-1/2 antigen/antibody combination assay
Negative
Hepatitis B surface antibody
Positive
Hepatitis B surface antigen
Negative
Hepatitis C antibody
Negative
A urine pregnancy test is negative.
The patient is counseled regarding consistent condom use and use of clean needles and equipment. She is referred to substance abuse treatment.
What is the most appropriate additional management?
Tenofovir disoproxil fumarate and emtricitabine
Tenofovir alafenamide, emtricitabine, and darunavir
Tenofovir alafenamide or tenofovir disoproxil fumarate
No additional management
A 28-year-old man is hospitalized for cough, headaches, nausea, and vomiting of 1 week's duration. Two days ago, he developed a stiff neck. He has otherwise been well and takes no medications.
On physical examination, temperature is 38 °C (100.4 °F), blood pressure is 110/60 mm Hg, pulse rate is 112/min, and respiration rate is 22/min. Nuchal rigidity is present; neurologic examination is normal. Abdominal examination reveals hepatosplenomegaly.
Cerebrospinal fluid studies:
Pressure, opening
240 mm H2O
Leukocyte count
100/µL (100 × 106/L); 80% lymphocytes
Glucose
35 mg/dL (1.9 mmol/L)
Protein
155 mg/dL (1550 mg/L)
HIV antigen/antibody combination immunoassay is negative. Blood cultures are negative. Cryptococcal serum and cerebrospinal fluid antigen test is pending. Cerebrospinal fluid Gram stain findings are shown.

What is the most appropriate treatment?
Liposomal amphotericin B and flucytosine
Acyclovir
Caspofungin
Vancomycin and ceftriaxone