The three basic components of pacemakers
What is:
1. the pulse generator, which houses the battery (lithium, lasts ~4-10yrs)
2. the electronic circuitry
3. the lead system (connect the generator to the endocardium; single or multiple and bipolar or unipolar) 
Describe one benefit and disadvantage of unipolar leads and one benefit and disadvantage of bipolar leads
Unipolar configuration
- is small and less prone to fracturing.
- not compatible with ICD systems and is prone to oversensing of myopotentials and electromagnetic interference.
Bipolar configuration:
- is compatible with ICDs
- is larger and more prone to lead fracturing
What conditions can lead to increase in frequency of ICD shocks? (list 3)
- ischemia (with or without infarction)
- hypokalemia
- hypomagnesemia
- pro-arrythmic effects administered to decrease the frequency of ventricular tachyarrythmias (ie., amiodarone, sotalol)
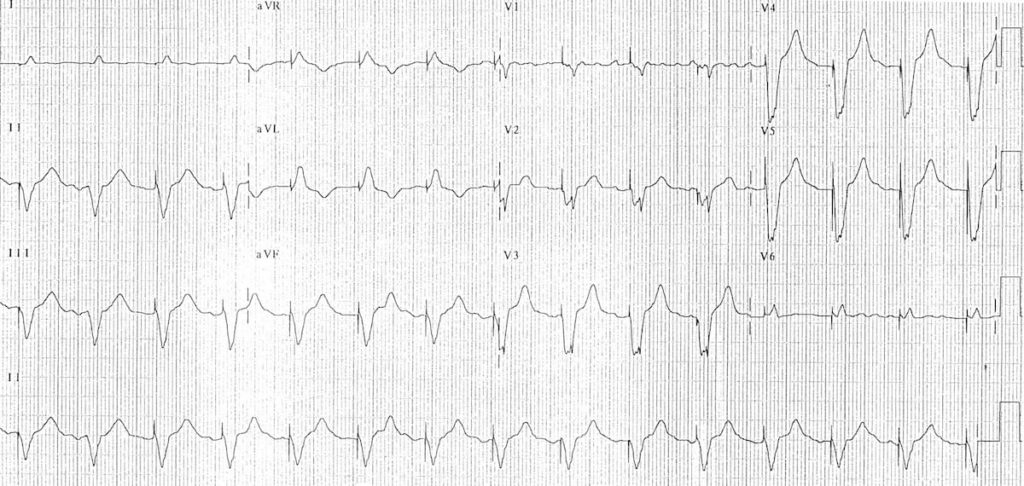 What kind of pacing is occurring? How can you determine a pacing spike (provide 1 feature).
What kind of pacing is occurring? How can you determine a pacing spike (provide 1 feature).
Ventricular.
No atrial pacing spikes.
Features of pacer spikes:
- Vertical spikes of short duration, usually 2 ms.
- May be difficult to see in all leads.
- Amplitude depends on position and type of lead.
- Bipolar leads result in a much smaller pacing spike than unipolar leads.
- Epicardially placed leads result in smaller pacing spikes than endocardially placed leads.
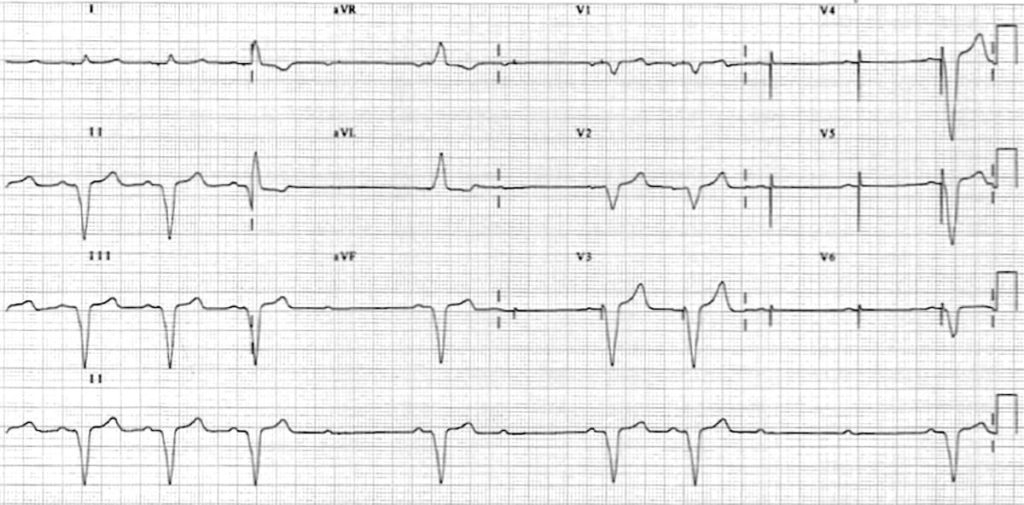 The pacing setting and malfunction occurring is:
The pacing setting and malfunction occurring is:
Ventricular paced rhythm with intermittent failure to capture:
- Atrial sensing appears to be intact — ventricular pacing spikes follow each P wave, most easily seen in V3-6 (tiny pacing spikes are also visible in I, aVR and V1).
- There is presumably an underlying complete heart block or high-grade 2nd degree AV block, as the native P waves do not capture the ventricles.
The 5 Letters on a Pacemaker represent
What is
Letter 1: Chamber Paced (A, V, D, 0=none)
Letter 2: Chamber Sensed (A, V, D, 0)
Letter 3: Sensing Response (T = triggered (not used), I = Inhibited, D= (A and V inhibited), 0 = none
Letter 4: Programmability (P= simple, M= multiprogrammable, R = Rate adaptive, C= Communicating, 0)
Letter 5: Anti-tachycardia fx (P= Pacing, S= Shock, D = Dual (shock pace) )
This most commonly occurs in VVI or DDI pacing. Occurs in ~ 20% of pts.
Includes: new or worsening of the symptoms that prompted initial pacemaker, including syncope/pre-syncope, weakness, lethargy, chest fullness, or pain, cough, uncomfortable pulsations in the neck or abdomen, RUQ pain, and other nonspecific sx.
Bonus 200 pts to describe the pathophysiology.
What is "Pacemaker Syndrome".
caused by loss of AV synchrony and by the presence of ventriculoatrial conduction. with VVI, ventricle is depolarized first resulting on ventricular contraction. If sinus node fx is still in tact, the atria can be depolarized by a sinus impulse and contract when the tricuspis and mitral valves are closed. this asynchrony results in an increase in jugular and pulm pressures and may produce sx of CHF. additionally, atrial distension can result in reflexive vasodepression. In it's most severe form, it results in elevated BNP and diuresis.
Class I indications for Implantable Cardioverter-Defibrillator Therapy include
What is:
1. Cardiac arrest resulting from VT or VF not caused by transient or reversible event
2. Spontaneous sustained VT
3. Nonsustained VT with CAD, prior MI, LV Dysfx, and inducible VF or sustained VT at electrophysiologic study that is not suppressible by a class I antiarrhythmic drug
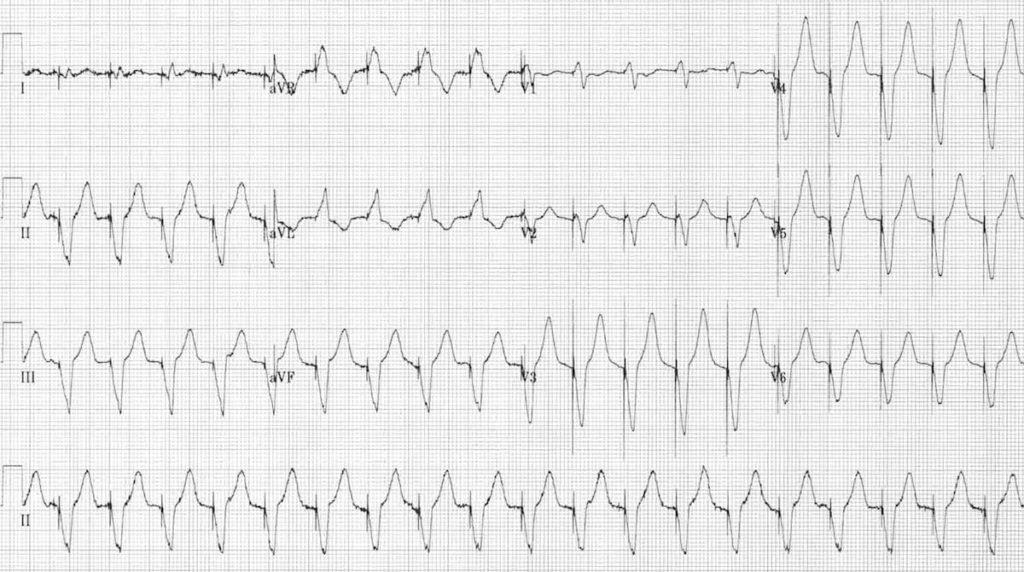
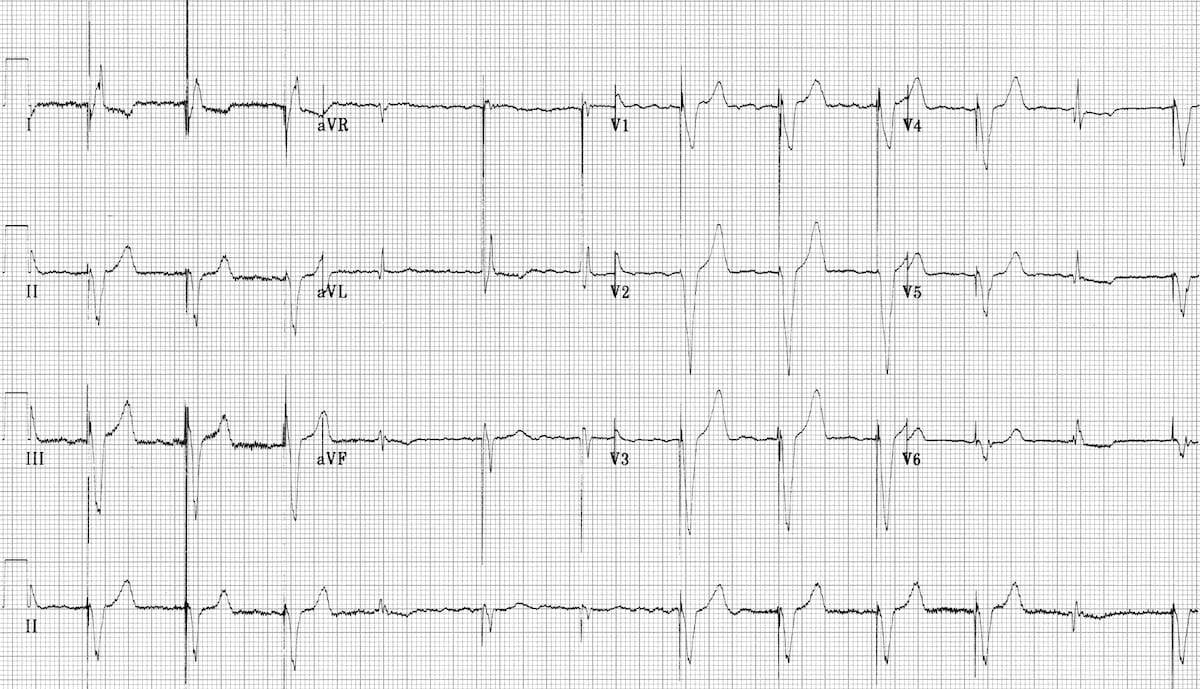 What is the predominant chamber paced?
What is the predominant chamber paced?
The 5th, 6th and 11th complexes are narrower with a different morphology - What are these beats called?
- Overall: Ventricular - LBBB morphology, thus R ventricular pacing
- fusion beats produced when the ventricle is simultaneously activated by both paced and supraventricular (native) impulses. You can see how the pacing spike is shortened and the QRS duration narrowed by the co-incident native impulse.
- The 4th complex is probably a supraventricular capture beat, although there may still be some hybridisation with a pacing spike.
What is the diagnosis and is his presentation related to the pacemaker?
90 M, hx of CAD and CHF with CRT, on spironolactone, with few days of weakness
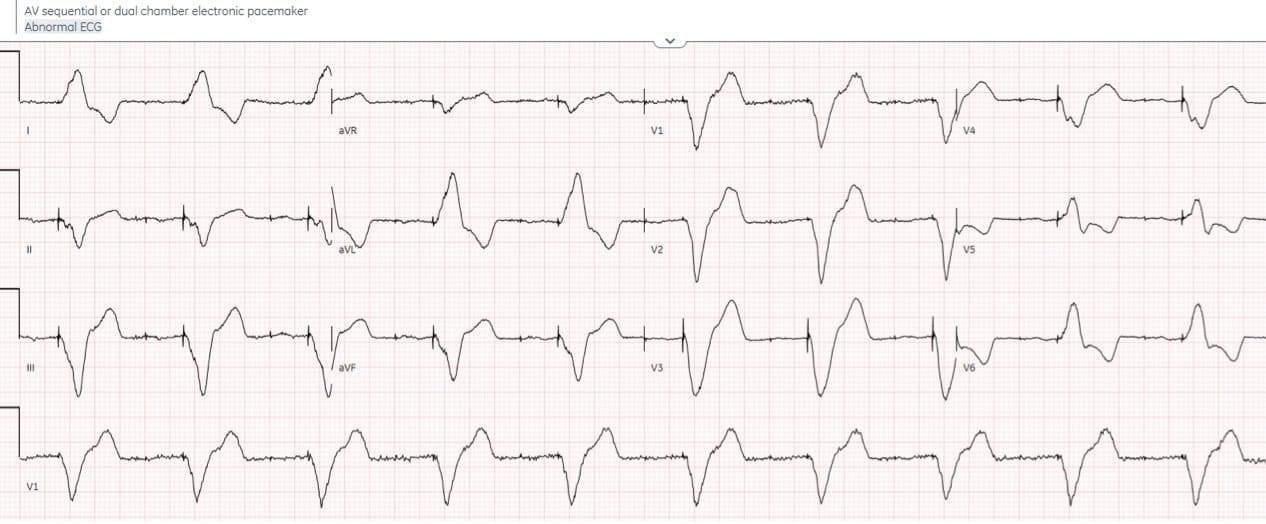
- H: atrial and ventricular paced with appropriate sensing and capture
- E: prolonged PR, LBBB morphology with excessively prolonged QRS
- A: left axis
- R: delayed R wave progression
- T: normal voltages
- S: appropriate discordance
Impression: atrial/ventricular paced with prolonged PR/QRS in patient with weakness on spironolactone. Potassium 7.1. After calcium and reversal of hyperkalemia, QRS returned to normal width
A common pacemaker setting is: DDD. These letters represent ____. List it's indications, advantages and disadvantages.
Dual paced, Dual sensed, and dual sensing response (A and V inhibited).
Indications: complete HB.
Advantages: Atrial tracking restores normal physiology.
Disadvantages: no rate responsiveness; requires two leads and advanced programming
- Atrial pacing occurs if no native atrial activity for set time.
- Ventricular pacing occurs if no native ventricle activity for set time following atrial activity.
- Atrial channel function is suspend during a fixed periods following atrial and ventricular activity to prevent sensing ventricular activity or retrograde p waves as native atrial activity.
Describe the 4 overarching causes of Pacemaker Malfunction, and 1 specific cause for each include:
1. Failure to Capture
- lead disconnection, break, or displacement; exit block (aka failure of lead in contat to stimulate endocardium to depolarize), battery depletion
2. Undersensing - lead displacement, inadequate endocardial lead contact, low-voltage intracardiac P waves and QRS complexes, lead fracture
3. Oversensing - sensing extracardiac signals: myopotentials, shivering, electrocautery
4. Inappropriate Rate - battery depletion, ventriculoatrial conduction with pacemaker-mediated tachycardia, 1:1 response to atrial dysrhythmias
List 5 Causes of ICD Malfunction (or of simply increased or abrupt change in shock frequency)
Box 70.4
- increased frequency of VF or VT (consider ischemia, electrolyte abn, or drug effects)
- displacement or break in ventricular lead
- recurrent NSVT
- sensing and shock of supraventricular tachyarrythmias
- oversensing of T waves
- sensing noncardiac signals
- recurrent VT with low shock strength (lead problem, change defib threshold)
- hemodynamically significant SVT
- inadequate backup pacing for bradyarrhythmias (spontaneous or drug-induced)
- assume malfunction but probably caused by VF that failed to respond to programmed shock parameters
 What kind of pacing is this
What kind of pacing is this
Atrial paced rhythm with 1st degree AV block:
- There are regular pacing spikes at 90 bpm.
- Each pacing spike is followed by a P wave, indicating 100% atrial capture.
- P waves are conducted to the ventricles with a prolonged PR interval (280 ms).
 Is this a pacemaker malfunction?
Is this a pacemaker malfunction?
Not necessarily.
There is a rapid ventricular-paced rhythm (120 bpm) with no evidence of preceding atrial activity (except for the first complex). The differential diagnosis of this rhythm includes:
- Pacemaker-mediated tachycardia (with retrograde P waves buried in the QRS complexes /T waves).
- Sensor-induced tachycardia.
- Could potentially be normal in the presence of an appropriate physiological stimulus (e.g. exercise).
PMT aka endless-loop tachycardia or pacemaker circus movement tachycardia.
- PMT is a re-entry tachycardia in which the pacemaker forms the antegrade pathway with retrograde conduction occurring via the AV node
- Caused by retrograde p waves being sensed as native atrial activity with subsequent ventricular pacing
- The paced ventricular complex results in further retrograde conduction with retrograde p-wave generation thus forming a continuous cycle
- Results in a paced tachycardia with the maximum rate limited by the pacemaker programming
- Can be terminated by slowing AV conduction e.g. adenosine or activation of magnet mode
- Newer pacemakers contain programmed algorithms designed to terminate PMT
Biventricular Pacing is also known as ___________, it is indicated for ___________________.
Bonus 200 if team can name the NYHA classes and criteria for biventricular pacing candidacy:
Cardiac Resynchronization therapy.
Systolic HF patients with LVEF <35% and LBBB in which there's ventricular dyssynchrony.
Bonus 200: Includes pts with:
1) NYHA Class II, III, IV HF with LV dysfx and LBBB or
2) NYHA Class I, II, III HF with LV dysfx and AV block
Your patient had an ICD/pacemaker inserted 1 month ago. He presents to your ED like this:
 What is the etiology of this presentation and what is the treatment?
What is the etiology of this presentation and what is the treatment?
Superior Vena Cava Syndrome.
Anticoagulation with Heparin/ LMWH ie., Enoxaparin, or warfarin with tx 3-6 mos.
Incidence of thrombosis with PPMs ranges 30-50% with ~1/3 having complete venous occlusion. Can involve axillary, subclavian, and innominate veins or the SVC. bc of extensive collaterals, only 0.5-3.5% of pts dev sx of acute thrombosis. rarely SVC syndrome.
Describe two ways ICD's interrupt VT.
1. Low-energy shocks (optimally, the required shock strength for cardioversion is less than half the maximum output (~30J) of the device). Will deliver up to 6 in refractory.
2. Antitachycardia pacing aka "overdrive pacing" - pace faster than the tachycardia and terminate the re-entrant VT

Atrial paced rhythm with Wenckebach conduction:
- There are regular atrial pacing spikes at 90 bpm; each one is followed by a small P wave indicating 100% atrial capture.
- However, not every P wave results in a QRS complex — the PR interval progressively lengthens, culminating in failure of AV conduction (“dropped QRS complexes”).
- There is a co-existent 2nd degree AV block with Mobitz I conduction (Wenckebach phenomenon).
- The Mobitz I is due to the patient being paced at a rate faster than his AV node can handle — at his own intrinsic rate of 50-60 bpm he had only a 1st degree AV block.
- Simply, the AV nodal dysfx becomes more apparent when paced beyond its intrinsic rate but is typically not clinically important provided no cardiac decomp.
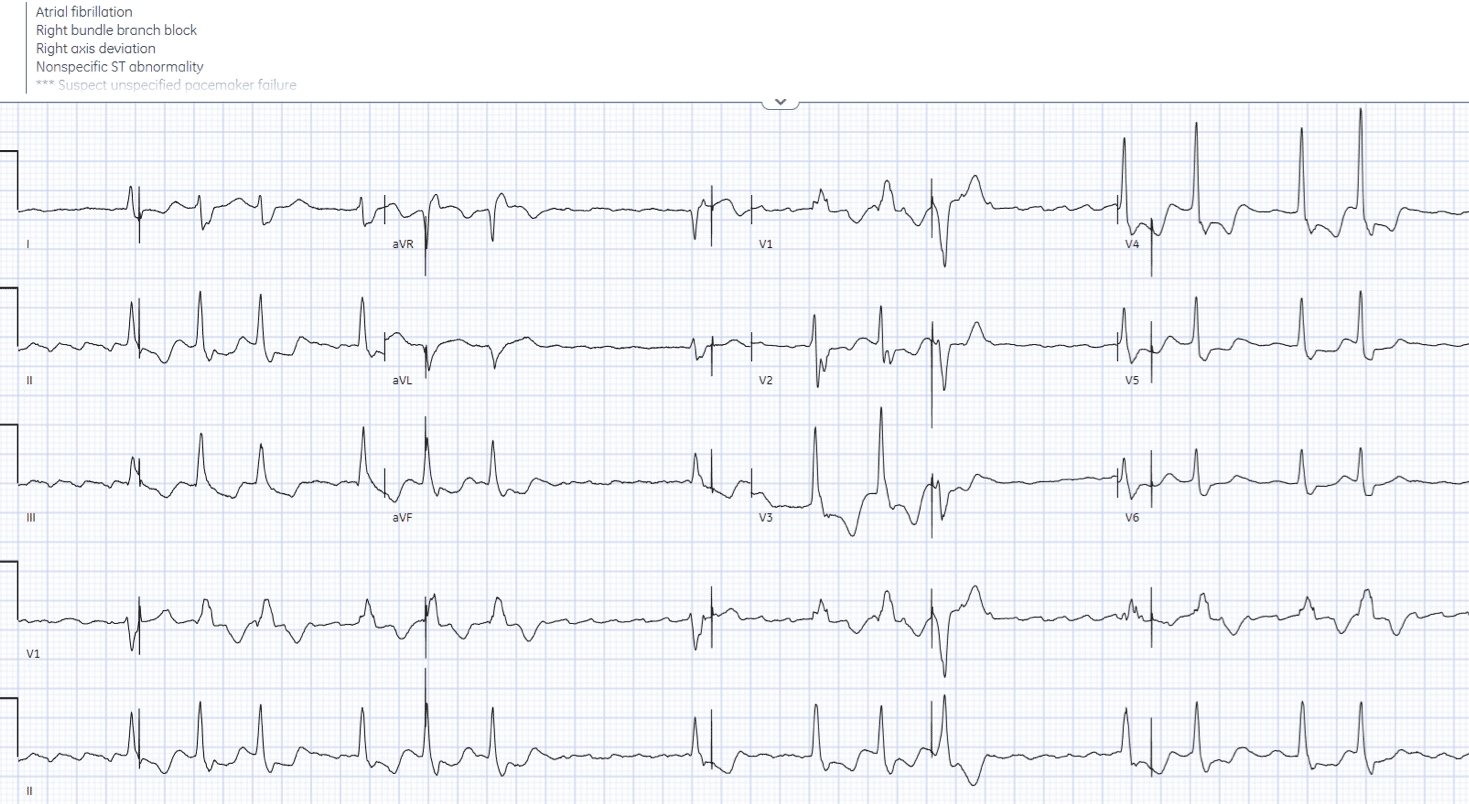 85 year old, history of Afib and MI, DDD pacemaker for AV block, with palpitations.
85 year old, history of Afib and MI, DDD pacemaker for AV block, with palpitations.
Dx and is it related to the pacemaker - if so what is the malfunction?
pacemaker electrical complication – failure to sense.
- H: atrial flutter with variable block, intermittent inappropriate pacing (failure to sense), last spike happens during the T wave
- E: RBBB
- A: right axis
- R: early R wave from RBBB
- T: normal voltages
- S: secondary ST changes
Impression: failure to sense leading to inappropriate pacing. Developed R-on-T triggering ventricular arrhythmia, cardioverted.
Box 70.1
Three of five of the Class I indications for Permanent Pacing in Adults include:
What is
1. 3rd degree and advanced 2nd degree AV block associated with either: i)sx brady (including HF) or ventricular dysrhythmia presumed to be a result of AV block, ii) sx brady 2nd to drugs required for dysrhythmia mgmt, iii) periods of asystole > 3 seconds or an escape rate of < 40 bpm or an escape rhythm originating below the AV node in an awake, asx pt in sinus iv) awake asymtomatic pts with afib and bradycardia with a documented pause of >/= to 5 seconds v) after catheter ablation of the AV node vi) postoperative AV block not expected to resolve vii) neuromusc. disease with AV block (ie., muscular dystrophies
2. Sx brady from 2nd degree AV block regardless of type or site of block
3. Asx, persistent 3rd degree AV block with awake ventricular rate > 40 bpm w/ cardiomegaly or LV dysfx or if block is below level of AV node
4. Chronic Bifascular or trifascicular block with intermittent 3rd degree AV block or type II 2nd degree AV block
5. 2nd or 3rd degree AV block with exercise in the absence of MI
What are the most common organisms isolated in local wound infx and systemically, and what empiric abx should be initiated.
How is this then managed?
Bonus 200: What is the incidence of pocket infection and bacteremia associated with PPM/ICD insertion.
S. aureus and S. epidermidis are isolated in 60-70% of cases. G-ve infx is rare.
Start with CTX/Vancomycin.
If +ve blood cx, the pulse generator and leads are typically removed, have temporary TVP, and IV abx for 4-6 weeks. Then PPM and lead are subsequently reimplanted.
Bonus: 2% for wound and subcutaneous infections, 1% for bacteremia with sepsis. However, 20-25% of those with a wound infection have positive blood cultures.
What is magnet mode and what does it do for pacemakers and ICDs?
Pacemakers: usually initiates asynchronous pacing AOO, VOO, DOO with backup rate pre-programmed.
ICDs: defibrillator activation
 Mode and underlying rhythm
Mode and underlying rhythm
- Atrial fibrillation with DDD pacing and occasional ventricular ectopics.
- There is an irregularly irregular rhythm with multiple atrial and ventricular pacing spikes.
- The majority of the QRS complexes are broad (120ms) and preceded by ventricular pacing spikes.
- The LBBB morphology is consistent with a ventricular pacing electrode located in the right ventricle.
- Beat 1 is narrow — this appears to be a native ventricular complex triggered by an atrial pacing spike. This indicates that AV conduction is intact to some degree (i.e. 3rd degree AV block cannot be present).
- Beat 9 is broad with a completely different morphology and axis to the rest of the strip — this is a ventricular ectopic beat.
- Beats 3, 6, 8, 10 and 12 are preceded by both atrial and ventricular pacing spikes — sequential A-V pacing.
- Beats 2, 4, 5, 7 and 11 are preceded by ventricular pacing spikes only. The absence of atrial pacing spikes suggests that the pacemaker is responding to native supraventriclar impulses.
- Given the absence of discernible P waves and the very irregular rhythm, it is likely that the underlying native rhythm is atrial fibrillation.
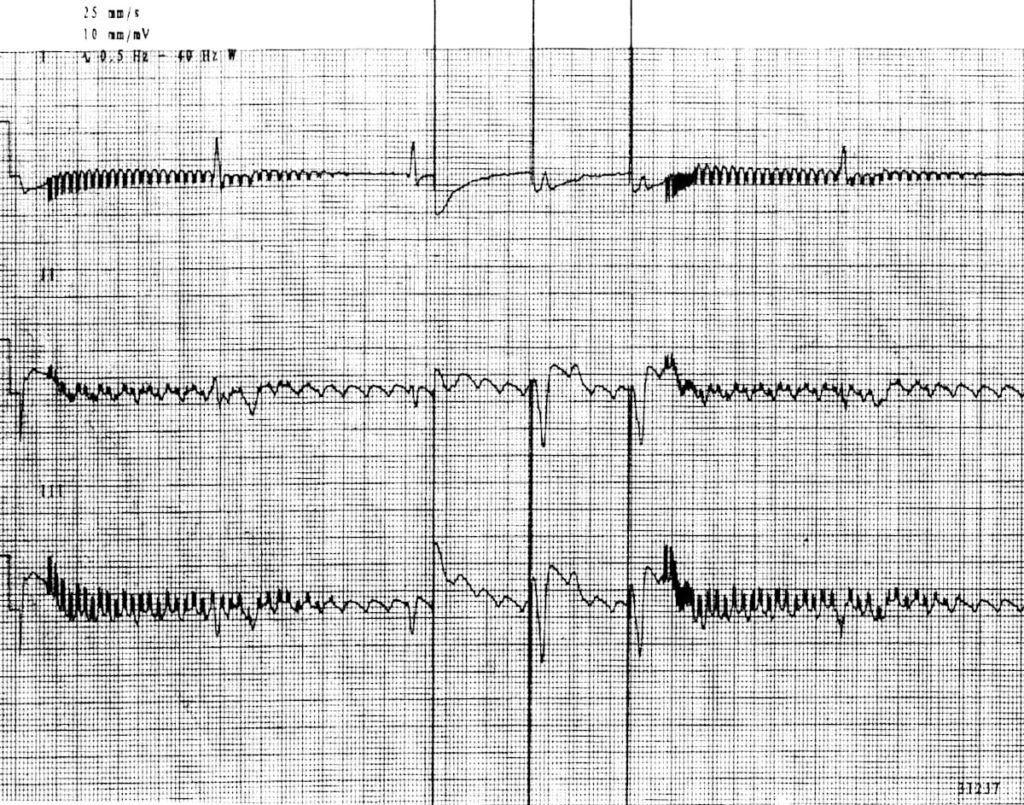 What is the diagnosis, etiology, and what is the intervention?
What is the diagnosis, etiology, and what is the intervention?
Runaway pacemaker.
Pathologic finding in older generation pacemakers from low battery voltage (hence low amplitude).
- The pacemaker delivers paroxysms of pacing spikes at 200 bpm, which may provoke ventricular fibrillation
- Paradoxically, there may be failure to capture — causing bradycardia — because the pacing spikes are very low in amplitude (due to the depleted battery voltage) and because at very high rates the ventricle may become refractory to stimulation
- Intervention: Application of magnet and new PPM.
- This specific one:
- The underlying rhythm is atrial flutter with 3rd degree AV block and ventricular escape rhythm at 30 bpm. Failed capture at first V00 pacer spike in middle.