A catheter whose tip terminates in a great vessel.
True or False: Morbid obesity is an indication for placement of a urinary catheter
FALSE
Appropriate indications are:
Perioperative use for selected surgical procedures
Urine output monitoring in critically ill patients
Management of acute urinary retention and urinary obstruction
Assistance in pressure ulcer healing for incontinent patients
Comfort during end-of-life care
What PPE is needed to enter the room of a patient with active COVID-19?
In order of application:
Hand Hygiene (wash hands or hand sanitizer
Gown
N95 respirator (appropriately worn, with no other masks, and that you are fit-tested for)
Goggles/face shield
Gloves
How long does a patient have to be in the hospital before a C. diff infection is considered hospital-acquired?
Hospital Day 4
Hospital Day 1 = The calendar date that the patient physically locates to an inpatient location.
If the stool sample is collected on Hospital Day 4 or later, the infection is considered hospital acquired.
This rule also applies to MRSA bloodstream infections, another major metric.
What are indications that a central line dressing needs to be changed?
The dressing is loose, damp, or visibly soiled.
Collection bag should be kept above or below the level of the bladder at all times?
Below
Routine maintenance includes
1. Maintain a sterile, continuously closed drainage system
2. Keep catheter properly secured to prevent movement and urethral traction
3. Maintain unobstructed urine flow
4. Empty collection bag regularly, using a separate collecting container for each patient, and avoid allowing the draining spigot to touch the collecting container
True or False: If you aren't touching the backside of a patient with an active C. diff infection you don't need to wear a gown or gloves.
FALSE
Contact Precautions with Handwashing (NOT hand sanitizer) are required for a patient with an active C. diff infection. This means that BEFORE ENTERING THE PATIENT'S ROOM you must perform hand hygiene (handwashing or hand sanitizer use), don a gown, and gloves.
C. diff bacteria turn into spores upon exit of the body. These spores are very hard to kill (which is why you cannot use hand sanitizer and must wash your hands with soap and water) AND they can spread very easily through the air.
Ultimately, these spores land on surfaces (you, your hands, your gloves, the gown you're absolutely wearing, the floor, beds, EVERYWHERE) where they will survive for YEARS (unless killed with BLEACH wipes), able to infect someone else as soon as they can hop a ride into their unassuming mouth.
How many hand hygiene observations are made on each unit every month?
100
5 Moments for Hand Hygiene
1. Before touching a patient
2. Before clean/aseptic procedures
3. After body fluid exposure risk
4. After touching a patient
5. After touching patient surroundings
How often should central line dressings be changed?
2 days for gauze, 5 days for transparent
What is the most important risk factor for development of infection?
Duration of catheterization
True or False: Since we're all wearing masks all the time, caring for a patient on Droplet Precautions requires no extra steps regarding PPE.
False. As with all transmission-based isolation precautions, the goal is to isolate the organism to the patient currently infected with it. In order to do this, all PPE worn into the room of the patient is considered contaminated and should be discarded either immediately before (gloves, gown) or after (googles/face shield, mask/respirator) leaving the room.
In the context of the current mask mandate, when exiting the room of a patient on Droplet Precautions (rule-out respiratory infection, Influenza [Flu], Rhinovirus) remove your mask, perform hand hygiene, and immediately don a new, clean mask.
What 4 types of surgeries and any associated SSIs (surgical site infections) are reported externally?
Colon, Abdominal hysterectomies (includes laparoscopic, abdominal just refers to what part of the body is entered), Knee, and Hip procedures.
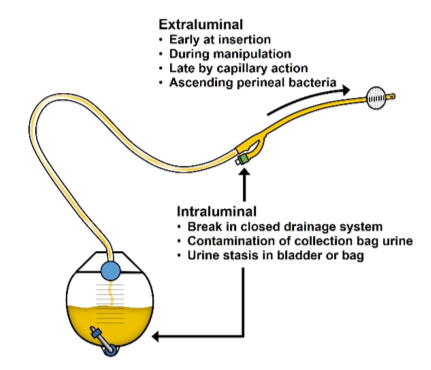
What are the 4 recognized routes for contamination of catheters?
1. skin insertion site
2. catheter hub
3. seeding of the catheter tip from a distant site of infection (through the blood)
4. infusate contamination
Name 1 of the 3 ways bacteria can enter the urinary tract in catheterized patients.
1. Introduction of organisms into the bladder at the time of catheter insertion
2. Periurethral route
3. Intraluminal route
You're about to provide patient-facing care to a patient with a chronic, productive cough, who has tested negative for all respiratory infections. What precautions should you take?
Standard Precautions.
These include: hand hygiene; use of gloves, gown, mask, eye protection, or face shield, depending on the anticipated exposure; and safe injection practices. They are based on the principle that all blood, body fluids, secretions, excretions except sweat, nonintact skin, and mucous membranes may contain transmissible infectious agents. Also, equipment or items in the patient environment likely to have been contaminated with infectious body fluids must be handled in a manner to prevent transmission of infectious agents (e.g., wear gloves for direct contact, contain heavily soiled equipment, properly clean and disinfect or sterilize reusable equipment before use on another patient). The application of Standard Precautions during patient care is determined by the nature of the HCW-patient interaction and the extent of anticipated blood, body fluid, or pathogen exposure.
So for this interaction, even though all infections for which we would apply Transmission-based Precautions have been ruled out, a mask and eye protection would be appropriate simply to protect yourself from whatever is spewed out in that cough.
When MRSA is cultured from this body site it must be reported to NHSN (National Healthcare Safety Network).
Blood. MRSA in the blood is like C. diff in this way. Anytime you see it you have to report it to NHSN.
What are the 5 key components of the central line bundle?
1. Hand hygiene
2. Maximal barrier precautions
3. Chlorhexidine skin antisepsis
4. Optimal catheter site selection, with avoidance of using the femoral vein for central venous access in adult patients
5. Daily review of line necessity, with prompt removal of unnecessary lines
What are the 4 components of care recommended for all patients to prevent or reduce the risk of CAUTIs?
1. Avoid unnecessary urinary catheters
2. Insert urinary catheters using aseptic technique
3. Maintain urinary catheters based on recommended guidelines
4. Review urinary catheter necessity daily and remove promptly
What Transmission-based Precautions should be used for a patient with RSV?
Contact Precautions
Although RSV is a respiratory infection and it may be transmitted by the droplet route, direct contact with infected respiratory secretions is the most important determinant of transmission and consistent adherence to Standard plus Contact Precautions prevents transmission in healthcare settings. RSV has been implicated in transmission through environmental contamination (as has VRE, C. diff, noroviruses and other intestinal tract pathogens). This is why PPE is donned upon room entry and discarded before exiting, to contain the pathogen, RSV, in the room.
True or False: After a period of stability or improvement on a ventilator, if a patient has an indicator of worsening oxygenation the criteria are met for a Ventilator-Associated Condition (VAC).
True
There are 3 types of Ventilator-Associated Events (VAEs):
VAC
Infection-related Ventilator-Associated Complication (IVAC): Meets the requirements for VAC and both:
1) Temp > 100.4 °F or <96.8 °F OR white blood cell count ≥ 12,000 cells/mm3 or ≤ 4,000 cells/mm3
AND
2) A new antimicrobial agent(s) is started and continued for ≥4 days
Possible Ventilator-Associated Pneumonia (PVAP):
Meets IVAC criteria and ONE of the following:
1) Positive culture meeting semi-quantitative thresholds w/o requirement for purulent respiratory secretions from endotracheal aspirate, bronchoalveolar lavage, lung tissue, or protected specimen brush
2) Purulent respiratory secretions PLUS organism identified from same sites as above.
3) Organism identified from pleural fluid; or Lung histopathology showing abscess, evidence of fungi, evidence of infection with viral pathogens based on immunohistochemical assays, cytology, or microscopy; or diagnostic test for Legionella species; or diagnostic test on respiratory secretions for flu, RSV, adenovirus, parainfluenza virus, rhinovirus, human metapneumovirus, coronavirus.