What population is most at risk of developing DKA?
Adolescent and young adult type 1 diabetics.
What does HHNKS stand for?
Hyperosmolar hyperglycemic nonketotic syndrome
Bonus Q: Who is more at risk of developing HHNKS?
What is a serious side effect of giving insulin too fast for DKA?
Cerebral edema. This is especially prevalent for younger ages.
T/F: A1C levels are an accurate way to measure long-term glycemic control for all races and ethnicities.
False!
What are some potential causes of hypoglycemia?
-overdose of insulin
-delayed/omitted meals
-increased exercise
-alcohol
What class of insulin do insulin pumps utilize?
Fast acting insulin
What causes someone to enter a state of DKA?
They have severe insulin deficiency that leads to severe hyperglycemia.
Why is ketosis not present in HHNKS?
Type 2 diabetics should still have enough insulin to prevent significant lipolysis.
Why could a patient experience GI symptoms and abdominal pain during DKA?
Hyperglycemia and hyperosmolarity can cause delayed gastric emptying (AKA gastroparesis), which can cause anorexia, nausea, and vomiting.
Lowered pH can cause cell injury and the stimulation of pain neurons, thus causing abdominal pain.
What type of lab would you use to determine a patient’s long-term glycemic control?
A1C
For a diabetic currently on insulin therapy, how often should they test their blood glucose level?
2-4 times per day
Bonus Q: How often for a type II diabetic not on insulin therapy?
What are some patient education topics regarding insulin?
-pt should always keep a spare vial of insulin available
-injecting insulin at room temp helps reduce local irritation at the injection site
-store insulin in refrigerator (if won’t be used within a month) and avoid temperature extremes
-insulin can be kept at room temperature if it’s used within a month from 1st opening it
T/F: There is not always a known trigger that causes a patient’s DKA.
True!
Bonus Q: What percent of DKA cases don’t have an obvious trigger?
What are some potential causes/triggers of HHNKS?
-failure to take hyperglycemic agents regularly
-drugs that decrease insulin secretion (diuretics) or increase insulin resistance (corticosteroids)
-acute illness
A patient presents to the ER with a headache and Kussmaul respirations. They report having peed excessively over the past 24 hours and when the labs come back, you find that they have extreme hyperglycemia and elevated potassium levels. What do you suspect the patient has?
Diabetic ketoacidosis (DKA)
Bonus Q: What is the body trying to accomplish through Kussmaul respirations?
What is the example discussed in class of an insulin-antagonist medication that raises blood glucose?
Corticosteroids
Bonus Q: What hormone do corticosteroids mimic?
What is some patient education you could provide to a diabetic about exercise?
-exercise will lower blood glucose levels, as well as improve circulation and increase resting metabolic rate
-it also increases HDL and lowers total cholesterol and triglycerides
-those on insulin therapy should eat a 15 g carb snack before engaging in moderate exercise. Protein will also help to maintain blood glucose.
If a diabetic gets sick, why might they need more insulin than usual?
The increased stress with increase cortisone levels, which is an insulin antagonist.
What are at least 4 clinical manifestations of DKA? (+25 pts for each additional answer)
-severe hyperglycemia
-polyuria (eventually leads to hypovolemia and then shock)
-electrolyte imbalances (K+, Na+)
-CNS alterations (headache, double vision, confusion, loss of consciousness)
-Kussmaul respirations
-acetone breath
-GI & abdominal symptoms (anorexia, nausea, vomiting, abdominal pain)
How are K+ levels affected during HHNKS?
They typically remain normal.
Bonus Q: Which serum electrolyte is typically elevated in HHNKS?
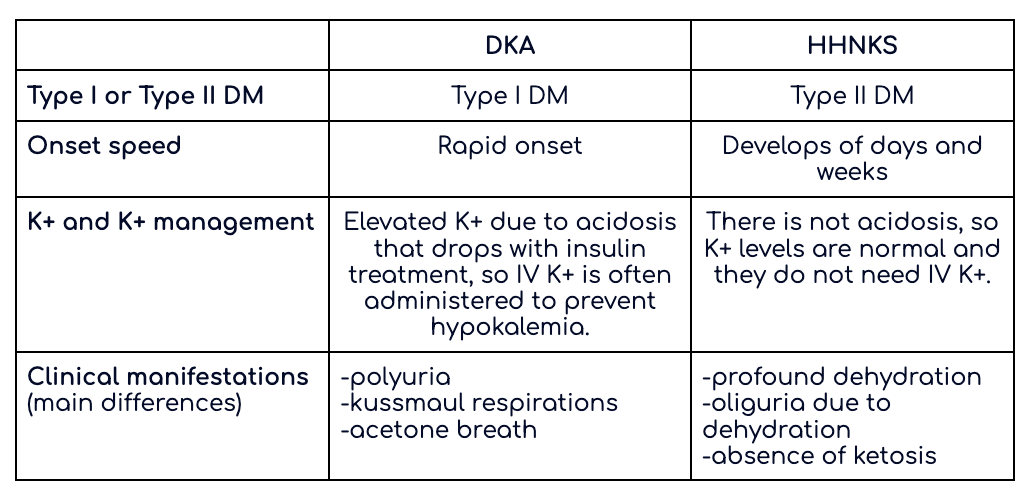
Explain the differences between DKA and HHNKS using this chart:
What does the body break down for energy in the absence of insulin?
Fat.
Bonus Q: What is developed/released as a result of fat breakdown that can cause severe metabolic acidosis?
What are signs of hypoglycemia you should inform your diabetic patient about?
-Fast heartbeat.
-Shaking.
-Sweating.
-Nervousness or anxiety.
-Irritability or confusion.
-Dizziness.
-Hunger.
Bonus Q: What is the pathophys behind many of these symptoms?
What are late clinical manifestations of hypoglycemia?
-headache
-changes in behavior and cognition
-weakness
-dizziness
-visual disturbances (especially in kids)
Bonus Q: If hypoglycemia goes untreated, what will eventually happen?
What are at least 3 potential triggers of DKA?
-omission of multiple insulin doses
-acute illness/infection
-trauma
-physiological or psychological stress
-insulin-antagonist medications (corticosteroids)
Bonus Q: What primary stress hormone is released as a result of physiological or psychological stress and how does it affect blood glucose levels?
List at least 3 clinical manifestations of HHNKS.
-profound dehydration (often more severe than in DKA)
-neurological (neuronal dehydration, ~10% pts present in a coma)
-absence of ketosis
-deep vein thrombosis and formation of thromboembolisms (due to dehydration)
-oliguria and renal failure (dehydration → hypovolemia → ↓ renal blood flow → oliguria → renal failure)
A newly diagnosed type 1 diabetic patient comes to the hospital and is diagnosed with DKA. What is our 1st nursing action after determining their airway and SPO2 are WNL?
Fluid resuscitation (C in ABCs). For DKA, the pt is immediately put on 0.9% NS IV fluid resuscitation, up to 1 L/hr, for 2-3 hours. This is also your first intervention with HHNKS.
Bonus Q: What is our 2nd intervention?
How does acidosis impact K+ levels?
It will raise K+ levels.
Bonus Q: Explain why K+ levels would increase.
What populations are at the highest risk of not properly following their insulin regimes?
-alcoholics
-drug abusers
-individuals without access to health care and/or diabetes education
What is hypoglycemia unawareness and what causes it?
After repeated episodes of hypoglycemia, the autonomic centers in the brain are injured and the diabetic no longer perceives the early sympathetic warning signs of hypoglycemia (shaky, tachycardia).
Bonus Q: What can help restore partial awareness?