A 42-year-old woman presents with abdominal pain for the last 2 days. She describes the pain as crampy and intermittent in the epigastric area, and she tells you that it is particularly worse after meals. She has a history of Roux-en-Y gastric bypass surgery that occurred 2 years ago.
Upon physical examination, she is afebrile. Her abdomen is soft and nontender with no masses.
Laboratory studies are shown below in the Table.
Laboratory studyValueNormal rangeWBC count7,700/µL3,200-9,800/µLHemoglobin13.2 g/dL11-14 g/dLPlatelets215,000/µL150,000-450,00/µLAlbumin4.3 g/dL3.5-5.5 g/dLAST334 U/L5-52 U/LALT282 U/L7-46 U/LAlkaline phosphatase115 U/L40-100 U/LTotal bilirubin1.7 mg/dL0.2-1.5 mg/dLAmylase42 U/L30-110 U/LLipase24 U/L13-141 U/L
ALT, alanine transaminase; AST aspartate aminotransferase; WBC, white blood cell.
Ultrasonography of the abdomen demonstrates a normal-appearing liver, mild distension of the gallbladder with several stones in the fundus of the gallbladder, and no apparent wall thickening or pericholecystic fluid. The common bile duct is dilated to 1.3 cm.
What is the next most appropriate step in the management of this patient's condition?
a)Manometry of the sphincter of Oddi
b)Surgical referral for cholecystectomy
c)Upper endoscopy with balloon dilation
d)Magnetic resonance cholangiopancreatography (MRCP)
e)Modified endoscopic retrograde cholangiopancreatography (ERCP
e) Educational Objective:
Recognize clinical scenarios in which endoscopic retrograde cholangiopancreatography is appropriate.
Key Point:
In patients likely to be diagnosed with and require treatment for biliary obstruction, ERCP is the preferred method. However, the procedure needs to be modified in order to account for the modified stomach (the procedure is still referred to as an ERCP).
Explanation:
Gallstone formation is common after rapid weight loss, as seen after bariatric surgery. These stones are composed of cholesterol, and, although the exact mechanism is not fully understood, there may be increased biliary stasis due to reduced caloric intake, or saturation of bile with cholesterol due to increased cholesterol mobilization. This patient has elevated transaminases and common bile duct dilation consistent with stones, sludge, or an anatomic obstruction of the common bile duct. Thus, ERCP will aid in both the diagnosis and treatment of a biliary obstruction. Of note, given the patient’s history of prior Roux-en-Y gastric bypass, ERCP may require surgical consultation to endoscopically or laparoscopically access the biliopancreatic limb. Several methods exist to assess the biliary systems via a modified ERCP; if interested, follow this link to an excellent discussion.
MRCP may also aid in diagnosis, but it does not offer a therapeutic option. Upper endoscopy may be useful to assess for peptic ulcer disease or evidence of an anastomotic stricture, but this patient does not demonstrate symptoms of obstruction or ulcer. Sphincter of Oddi dysfunction can also cause an elevation of transaminases and bile duct dilation, but the presence of a stone or sludge should be ruled out first. There is no gallbladder wall thickening or pericholecystic fluid to suggest acute cholecystitis, so immediate surgical referral for cholecystectomy is not the most appropriate next step.
A 56-year-old woman presents with chest pain radiating to the jaw, and she is feeling nauseous and is sweating. In the diagnostic interview she states that her daughter suddenly died the previous day, and her symptoms began to appear shortly after she had the news. Results on electrocardiography (ECG) show a pronounced ST-segment elevation; cardiac biomarkers are pending. Which condition(s) should be suspected?
A) MI
B) MYOCARDITIS
C) STRESS INDUCED CARDIOMYOPATHY OR MI
C) STRESS INDUCED CARDIOMYOPATHY
(C) Educational Objective:
Recognize the importance of ruling out acute myocardial infarction before diagnosing stress-induced cardiomyopathy.
Key Point:
While stress-induced cardiomyopathy, also known as Tako-Tsubo cardiomyopathy, can mimic the symptoms and some ECG findings of myocardial infarction, its diagnosis requires the absence of obstructive coronary disease, specific regional wall motion abnormalities in the left ventricle, and other distinguishing features. An acute myocardial infarction should always be ruled out first given its immediate life-threatening implications.
Explanation:
Stress-induced cardiomyopathy (also known as Tako-Tsubo cardiomyopathy) may indeed be the final diagnosis; however, acute myocardial infarction must be ruled out before this diagnosis can be made with certainty. This condition may occur in postmenopausal women and is commonly--but not always--triggered by a stressful life event, such as the death of a family member.
In stress-induced cardiomyopathy, ECG abnormalities and clinical manifestations are usually out of proportion to the degree of cardiac biomarker elevation. Given that patients with criteria are brought to the cath lab before the biomarker results are available, this feature can often only be appreciated in hindsight.
The full diagnostic criteria for stress-induced cardiomyopathy specified by the Mayo Clinic are:
- New ECG abnormalities (either ST-segment elevation and/or T wave inversion) or modest elevation in cardiac troponin
- Absence of obstructive coronary disease or angiographic evidence of acute plaque rupture (this requires a cardiac catheterization)
- Transient hypokinesis, akinesis or dyskinesis of the left ventricular mid segments with or without apical involvement. The regional wall motion abnormalities typically extend beyond a single epicardial coronary distribution. A stressful trigger is often--but not always—present (will partially be visible during the cardiac cath with details later visible on echocardiogram)
- Absence of pheochromocytoma or myocarditis (history of above patient does not match this)
While hunting for deer in the woods of southern Illinois, a 46-year-old man was bitten on his left hand by a raccoon that was acting unusually tame. The man was not vaccinated against rabies. On examination, several bite marks are clearly visible. What is the first step which needs to be taken as part of postexposure rabies prophylaxis?
A) administration of human diploid cell vaccine (HDCV) in tissues around the bite sites
B) IV ceftriaxone and vancomycin
C) thorough cleansing of the bites with water and povidone-iodine solution
D) administration of purified chick embryo cell vaccine (PCECV) in tissues around the bite site
E) irrigation of the bites with human rabies immune globulin (HRIG)
C) thorough cleansing of the bites with water and povidone-iodine solution
he first important step in postexposure rabies prophylaxis is to deeply and thoroughly cleanse the wound(s), including the base of deep puncture wounds, regardless of vaccination status. Irrigation with water for around 15 minutes is recommended followed by cleansing with povidone-iodine solution because it inactivates the rabies virus. Wound cleansing with a viricidal agent, such as povidone-iodine solution, has been shown to prevent up to a third of rabies infections. However, a recent study showed that less than 20% of victims of animal-bites had their wounds properly cleansed.
Following thorough wound cleansing, this patients requires both active and passive postexposure prophylaxis. For HRIG, the Advisory Committee on Immunization Practices (ACIP) updated its recommendations on rabies postexposure prophylaxis in 2010, but the recommendations regarding HRIG remain unchanged. ACIP currently recommends that a single dose of HRIG be administered to all unvaccinated persons. If anatomically feasible, most of this dose should be infiltrated around and into any wounds. Any remaining volume should be intramuscularly injected into the deltoid muscle in adults and into the quadriceps muscle in children (there have been some reported failures after gluteal administration). It is worth noting that any remaining HRIG dose should be injected at a site distant from the site of the first vaccine administration because the immunoglobulin inactivates the vaccine (for this reason, it is also important to use two different syringes for injecting HRIG and the vaccine). Subsequent doses of the vaccine can be administered in the same anatomic location in which the remaining HRIG dose was administered on day 0. Individuals who have been previously vaccinated against rabies should not receive human immune globulin.
For unvaccinated patients with a possible exposure to rabies, ACIP had previously recommended a five-dose rabies vaccination regimen with HDCV or PCECV. The 2011 update reduced the number of vaccine doses to four. Previously vaccinated patients only require two doses. See the table below for details.
A 52-year-old man with severe emphysema is admitted to the hospital with an exacerbation. On hospitalization day 2, his clinical condition worsens with increasing oxygen requirements and significant tachypnea, requiring transfer to the intensive care unit and intubation.
He is started on broad-spectrum antibiotics and initially improves. However, by hospitalization day 7, his white blood cell count is increased to 19,000/µL. Repeat blood cultures do not have any growth by 72 hours, and there is no evidence of urinary or Clostridioides difficile infection. Doppler ultrasonography of the lower extremities does not demonstrate deep venous thrombosis.
Right-upper quadrant ultrasonographic findings demonstrate a thickened, distended gallbladder with no sludge or stones and mild pericholecystic fluid. The common bile duct measures 4 mm. The patient remains on norepinephrine for blood pressure support.
What is the next step in the management of this patient's condition?
A)cholecystostomy
B)endoscopic retrograde cholangiopancreatography (ERCP)
C)continuation of broad-spectrum antibiotics and observation
D)hepatobiliary (HIDA) scan
A)
Educational Objective:
Assess, diagnose, and treat patients with acalculous cholecystitis.
Key Point:
Patients who are critically ill with a high suspicion of acalculous cholecystitis should undergo percutaneous cholecystostomy to improve their clinical status.
Explanation:
Based on his clinical parameters and gallbladder appearance on ultrasonography, this patient likely has acalculous cholecystitis (AC), which is a necroinflammatory disease of the gallbladder. AC is associated with a high mortality rate among those who are critically ill. The pathogenesis is likely multi-factorial and includes gallbladder stasis, ischemia, and acute inflammation. Predisposing factors may include comorbidities such as coronary disease and diabetes, as well as acute events such as major trauma, sepsis, or TPN.
The definitive therapy of AC is a cholecystectomy. However, in patients who are hemodynamically unstable on vasopressors, a percutaneous cholecystostomy is a lower-risk intervention that can improve the patient’s clinical status and hence this is the management of choice for this patient. He would require cholecystectomy despite his poor hemodynamic status if there was any evidence of necrosis, perforation, or emphysematous cholecystitis on ultrasound.
There are small case reports of endoscopic drainage of the gallbladder, but this method is still investigational. HIDA scan can be useful in confirming the diagnosis of AC; however, patients who are critically ill with a high suspicion for AC should move on to definitive therapy rather than further diagnostic testing.
A 37-year-old man presents to the emergency department (ED) with alcohol intoxication and psychiatric disturbances consistent with a psychotic episode. He has a history of alcohol and drug abuse as well as schizophrenia, and he has a history of attempted suicide 2 years ago. Upon questioning, the patient states he has suicidal ideation.
Which of the following factors in the patient's presentation or history is the strongest predictor of his imminent suicide risk?
A) schizophrenia in the context of alcohol abuse
B) the imminent risk cannot be assessed in an intoxicated patient who is cognitively not able to participate in their care plan.
C) schizophrenia
D) alcohol abuse
(B) Educational Objective:
Recognize pitfalls when assessing suicide risk.
Key Point:
To assess imminent suicide risk, patients must be capable of cognitively participating in their evaluation. A patient who is intoxicated does not qualify as cognitively capable of participation. No data exist to support a particular blood alcohol level at which a patient can undergo a psychiatric evaluation.
Explanation:
An article published in 2016 that is focused on emergency medicine care of suicidal patients summarizes the currently best available approach to suicide risk assessment in the ED.
The starting point is to ensure that the patient expressing suicidal ideation is cognitively able to participate in an assessment of their CURRENT suicidal risk. Current risk is FIRST OF ALL determined by active suicidal ideation; if acute suicidal ideation present, then historical factors will potentiate the active risk. However, the presence of acute suicidal ideation cannot be determined in an intoxicated patient.
Those intoxicated with alcohol or drugs are considered incapable of meaningful participation and should be observed and then have their cognitive capacity reassessed before the ED physician attempts to assess their risk for suicide.
Once a patient is judged to be cognitively able to participate in a suicide risk assessment, 2 questions must be answered in the ED:
- Does the patient need a formal psychiatric evaluation prior to disposition?
- This question can be answered with an assessment tool developed in 2016 by a consensus panel specifically for suicide risk assessment in the ED. This tool can be found in Figure 1 of the original article. Most patients who present with suicidal ideation will "fail" this questionnaire, which leads to asking the second question.
If this first assessment toll yields the answer "yes" to this first question (does the patient need a formal psychiatric evaluation prior to disposition?), then the next question is:
- Does this patient need psychiatric admission, or can he/she be discharged after psychiatric evaluation in the ED?
- Ideally, the psychiatrist on call will answer this question. However, if no psychiatrist is available, then ED physicians can use an assessment tool to conduct a formally endorsed, mini-assessment to determine whether a psychiatric admission is required or whether discharge is appropriate. This tool creates a matrix of 3 key areas to consider:
- Risk factors (acute psychiatric exacerbation is the most significant risk)
- Patient suicidality (eg, active attempt, specific plan)
- Protective factors (eg, good social support system)
- Follow this link to Figure 2 in the same article previously mentioned to view the second tool. In general, patients with both moderate- and high-risk profiles are admitted to the hospital.
- Ideally, the psychiatrist on call will answer this question. However, if no psychiatrist is available, then ED physicians can use an assessment tool to conduct a formally endorsed, mini-assessment to determine whether a psychiatric admission is required or whether discharge is appropriate. This tool creates a matrix of 3 key areas to consider:
Experts warn that assessing suicide risk remains an inaccurate science. They also emphasize that most acute suicide crises are short-lived and that the best care of a current crisis still cannot prevent future attempts, and that is true whether or not a patient is admitted to the hospital.
A 44-year-old man who was in good health complains of new onset diaphoresis and chest pain that is relieved when he leans forward.
Further workup is negative for myocardial infarction.
You suspect that he has acute pericarditis. Common causes of acute pericarditis include which of the following?
A) autoimmune diseases
B) cerebrovascular accident
C) Leishmania donovani infection
D) Histoplasma capsulatum infection
A) autoimmune diseases
Autoimmune diseases, such as lupus, can cause acute pericarditis. Viral infections (Coxsackie A and B viruses; more frequent in children), idiopathic causes, myocardial infarction, tuberculosis, and trauma can also lead to acute pericarditis. Cerebrovascular accidents and Leishmania donovani and Histoplasma capsulatum infections do not generally cause acute pericarditis.
A 15-year-old boy complains of 5 days of sore throat, fever, and fatigue. Rapid streptococcal testing is performed, the result of which is negative. However, the result from monospot testing is positive.
The patient is on the basketball team at his school.
On physical examination, he has pharyngitis and cervical lymphadenopathy but has no difficulty with breathing.
Which of the following is correct regarding appropriate treatment for this teenager?
A) Exclude him from sports for 8 weeks to lower his risk of splenic rupture.
B) Treat his mononucleosis with acetaminophen or ibuprofen as needed.
C) Treat him with valacyclovir to decrease the duration of his illness.
D) Treat him with prednisone to decrease the duration of his illness.
B) Treat his mononucleosis with acetaminophen or ibuprofen as needed.
Care for mononucleosis is supportive, with steroids reserved for patients who present with swelling that threatens their airway patency.
Explanation:
Mononucleosis presents with fever, lymphadenopathy, and pharyngitis. It is caused by Epstein–Barr virus infection. The treatment is largely symptomatic.
Steroids and antivirals are ineffective in uncomplicated mononucleosis. However, steroids and consultation with an otolaryngologist should be urgently obtained in cases of swelling that threatens airway patency.
Splenic rupture is a risk of mononucleosis, and it is most common in the first 2 weeks of the illness. Patients are advised to abstain from vigorous exercise for 3 to 4 weeks, not 8 weeks, to reduce the risk of splenic rupture.
Atrial fibrillation (AF) is a commonly encountered dysrhythmia; so, when a patient in AF presents to a health care professional, he or she needs to initially determine whether the patient's overall condition is stable or unstable. Determining whether the AF is chronic or of new onset is also important.
The differential diagnosis for causes of new-onset AF is broad and includes a number of potentially life-threatening conditions. Underlying conditions that may cause AF include myocardial ischemia, hypoxia, chronic pulmonary disease, valvular heart disease (especially mitral valve), hypertensive heart disease, thyrotoxicosis, pulmonary embolus, electrolyte disturbances, myocarditis/pericarditis, hypertrophic cardiomyopathy, and intoxicants (eg, ethanol, cocaine, amphetamines).
Which of the following is the most appropriate intervention for new-onset AF associated with an alcohol binge, also known as the "holiday heart" syndrome?
A) Check serum magnesium level and give magnesium sulfate supplementation if serum level is low.
B) cardiovert all patients with < 24-hour history of new-onset AF.
C) Load the patient with intravenous phenytoin 17 mg/kg at a rate < 25 mg/minute.
D) Provide intravenous hydration, ensuring that thiamine is administered before giving dextrose-containing fluids.
E) Administer intravenous sodium bicarbonate 1 mEq/kg.
D) Provide intravenous hydration, ensuring that thiamine is administered before giving dextrose-containing fluids.
Educational Objective:
Identify the appropriate interventions for patients presenting with "holiday heart" syndrome after an alcohol binge.
Explanation:
"Holiday heart" syndrome should come to mind in the differential diagnosis when a patient presents to you with new-onset AF and ethanol abuse. Rehydration with intravenous fluids, preceded by thiamine administration, followed by dextrose-containing fluids if needed, along with correction of potassium and magnesium deficiencies, will often resolve the dysrhythmia.
Most of these individuals have whole-body magnesium deficiencies, even though their serum magnesium level may be normal. Unless significant renal insufficiency is present, empiric supplementation with magnesium sulfate is appropriate, and measurement of a serum magnesium level adds little to the patient's care except additional expense.
Cardioversion is usually not indicated in this situation because patients are not typically unstable. Indeed, cardioversion may be relatively ineffective due to the fluid and electrolyte disturbances present. Empiric use of sodium bicarbonate is not indicated, nor is intravenous phenytoin.
A 3-month-old boy born with HIV infection is referred to you because he requires antiretroviral therapy (ART). His mother did not seek prenatal care, so ART was not administered during the pregnancy. The child was recently placed in foster care and has not yet received any substantial medical care to address his HIV infection.
Laboratory testing is significant for an HIV-RNA of 90,000 copies/mL and a CD4 cell count of 350 cells/µL.
Which of the following is the preferred regimen based on the age of this patient?
A) abacavir (ABC)/lamivudine (3TC)/lopinavir (LPV)/ritonavir (r)
B) dolutegravir (DTG)/tenofovir (TDF)/emtricitabine (FTC)
C) atazanavir (ATV)/lamivudine (3TC)/didanosine (DDI)
D) elvitegravir (EVG)/cobicistat (COBI)/tenofovir (TDF)/emtricitabine (FTC)
A) abacavir (ABC)/lamivudine (3TC)/lopinavir (LPV)/ritonavir (r)
Current guidelines from the World Health Organization and the US Department of Health and Human Services recommend starting ART in all HIV-positive patients, including children and adolescents. Certain regimens are recommended for each age group, mostly based on the adverse-event profile of the drug combination. ABC plus 3TC in combination with LPV/r is the recommended dual nucleoside reverse transcriptase inhibitors (NRTIs) and protease inhibitor (PI), respectively, for children aged 3 months or older, and it would be appropriate for the patient in this case. The majority of the ABC/3TC formulation is not protein bound in the plasma, leaving 83% free. In addition, the ABC/3TC formulation readily penetrates the central nervous system. Patients should be tested for HLA-B*5701, because individuals with that HLA type present are predisposed to develop a hypersensitivity drug reaction to ABC. Overall, ABC has minimal adverse events and drug reactions, reacting with none of the ART medications; however, there are drug–drug reactions with methadone and ethanol. 3TC also lacks significant toxicities, although cases of lactic acidosis have been rarely observed. Of note, 3TC is associated with the formation of M184V mutations in the virus, specifically limiting the efficacy of 3TC and FTC. LPV is always combined with RTV, which is a PI that has the strongest inhibitory properties of the liver cytochrome enzyme CYP3A4, because the majority of LPV is protein bound (99%). Because PIs may induce or inhibit CYP3A4 or other cytochrome liver enzymes, they are not generally administered together except in specific formulations.
A single-tablet formulation of EVG/COBI/TDF/FTC is based on an integrase strand transfer inhibitor combined with 2 NRTIs, as well as an inducer of CYP3A (COBI). EVG/COBI/TDF/FTC is the preferred initial regimen in young adults 12 years of age or older. The formulation has been shown to have low toxicity, low rates of resistance, and substantial effectiveness toward HIV-1 infection. EVG is highly protein bound in the plasma (> 99%) and is processed in the liver by the cytochrome pathway. COBI is added to the formulation to inhibit CYP3A4 and, thus, increase plasma levels of EVG. Of note, TDF is renally excreted and associated with renal disease; therefore, renal function testing should be performed during each visit. Contraindications include inducers of CYP3A4, such as rifampin, as they will result in decreased concentrations of the non–protein-bound form of the drug in the plasma.
A 39-year-old man is evaluated for several months of progressive fatigue, a 10-pound weight loss, and dark urine output for the past 2 weeks. He is not on any medications, does not smoke, and enjoys a couple of beers every day. He has had no operations. A review of systems does not uncover any other symptoms.
On physical examination, he is noted to have slight scleral icterus and a mildly prominent liver edge. He does not appear to have any other stigmata of long-term liver disease. He is not currently on any medications other than methotrexate and folic acid.
Laboratory testing is performed, and the results are shown in the Table.
Laboratory study Value Normal range
WBC count 7700/µL 4,500-10,000/µL
Hemoglobin 11.8 g/dL 11-14 g/dL
Platelets 150,000/µL 150,000-450,00/µL
Albumin 3.6 g/dL 3.5-5.5 g/dL
AST 78 U/L 5-52 U/L
ALT 92 U/L 7-46 U/L
Alkaline phosphatase 275 U/L 40-100 U/L
Total bilirubin 4.8 mg/dL 0.2-1.5 mg/dL
INR 1.3 0.8-1.2
ALT, alanine transaminase; AST aspartate aminotransferase; INR, international normalized ratio; WBC, white blood cell.
Given these findings, magnetic resonance cholangiopancreatography is ordered. The results demonstrate a hypertrophied caudate lobe with mild intrahepatic biliary ductal dilatation with several areas of ductal narrowing. No other masses are seen. Liver biopsy is performed and is notable for epithelial cell necrosis, ductopenia, and concentric fibrosis around the bile ducts.
Other than initiating treatment with ursodeoxycholic acid (UDCA), what else should be recommended at this time?
A) Prophylactic cholecystectomy
B) Colonoscopy
C) D-penicillamine therapy
D) Endoscopic retrograde cholangiopancreatography (ERCP) for biliary stenting
B) Colonoscopy
Educational Objective:
Describe the conditions associated with primary sclerosing cholangitis.
Key Point:
Inflammatory bowel disease is found in 75% of patients with primary sclerosing cholangitis. There is also an increased risk of colon cancer.
Explanation:
The patient above has radiographic, laboratory, histologic, and clinical findings consistent with primary sclerosing cholangitis (PSC), which is a long-term, autoimmune inflammatory disease that leads to inflammation and scarring of both intra- and extrahepatic bile ducts. Males are twice as commonly affected as females. Approximately 50% of patients with PSC will develop cholangiocarcinoma within 2 years of diagnosis. The prevalence of PSC is unknown, but approximately 75% of patients with PSC have concurrent inflammatory bowel disease (usually ulcerative colitis [UC]). Not only do these patients have a high incidence of UC, but they also have a risk for colon cancer higher than the average population with UC. For these reasons, all patients newly diagnosed with PSC should be offered a colonoscopic evaluation. Although PSC is associated with gallbladder disease, there is no indication for cholecystectomy at this time. Neither high-dose steroids nor D-penicillamine has been shown to be effective therapies for PSC. ERCP with stenting can be considered in cases of dominant large duct strictures, but not with predominantly small to medium duct disease.
PSC is a long-term, cholestatic liver disease that can shorten life and may require liver transplantation. The cause is unknown, although it is commonly associated with colitis. There is no approved or proven therapy, although UDCA is sometimes used on an empiric basis. Complications, including portal hypertension, fat-soluble vitamin deficiency, metabolic bone diseases, and the development of cancers of the bile duct or colon, can occur.
An 87-year-old man with pneumonia and significant shortness of breath arrives from a nursing home at the emergency department. His accompanying records contain a physician's orders for life-sustaining treatment (POLST), which he signed 4 years ago. The form indicates he does not want to be intubated. The patient is mentally alert and oriented and able to communicate. He is obviously struggling, and respiratory failure is likely to develop within the next few hours.
What is the medically correct approach to this situation?
A) The POLST form is invalid because it is older than 12 months.
B) The patient’s surrogate decision maker should be contacted to confirm the content of the POLST form before withholding life-saving treatments.
C) Provide comfort measures but do not intubate the patient based on the preferences indicated on the POLST form.
D) Allow the patient to voice any changes in treatment preferences, which will override those indicated on the POLST form.
D)
A patient with intact decision-making capacity has the authority to override ANY previous advance planning documents. Clinicians should give patients who have decision-making capacity an opportunity to voice any changes in their treatment preferences that deviate from their POLST form or any other advance directive form, such as a “do not attempt resuscitation” (DNAR) form. Neither POLST forms nor DNAR forms expire.
Review:
- Two Categories of End-Of-Life Care Forms: End-of-life care documents can be separated into those that are standing (portable) physician orders and those that are patient wishes not linked to a physician order.
- Portable Physician Order Documents:
- POLST, DNAR, and DNI are all examples of end-of-life portable physician orders.
- In some states, the POLST form is known by other names, such as medical orders for scope of treatment (MOST), medical orders for life-sustaining treatment (MOLST), physician orders for scope of treatment (POST), or transportable physician orders for patient preferences (TPOPP).
- These forms are only intended for patients with terminal, life-limiting illnesses (there are some exceptions).
- These forms require a physician signature on a state-approved form.
- These forms are binding for both physician and nonphysician caretakers unless overridden by the patient him/herself (assuming competent decision making).
- In an emergency situation, any procedures normally required by law of emergency personnel (e.g. CPR) are overridden by the treatment preferences indicated on an end-of-life portable physician order form.
- POLST, DNAR, and DNI are all examples of end-of-life portable physician orders.
- Patient Wishes Documents:
- Advance directives and living wills are examples of forms that document patient wishes without doctor orders.
- These forms are available to patients at any point in their lives.
- These forms do not contain binding physician orders; nonphysician caretakers must follow their respective institution’s medical protocols rather than a patient’s advance directive wishes until a physician provides an individualized medical order to follow the advance directive.
- Physicians can consider a patient’s advance directive as they make treatment decisions (often in discussion with an appointed representative); however, this does not free the treating physician from the duty to decide on a case-by-case basis between 2 conflicting ethical principles, ie, tending to the patient’s body vs the patient’s will as expressed in the advanced directive.
- Portable Physician Order Documents:
A 68-year-old man complains that his chronic, irregular heartbeat has been more bothersome in the last 24 hours. He states that he is compliant with taking his digoxin.
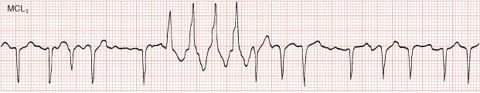
Initial findings on electrocardiography (ECG) shows atrial fibrillation (AF) with a ventricular rate of 89 beats/minute (see Figure). During the patient's workup, a nurse alerts you to a sudden run of fast beats on the patient's monitor.
What is the most prudent reaction to the rhythm shown in this image?
a)Avoid atrioventricular-nodal blockers in this patient.
b)Give amiodarone if the run of fast beats becomes sustained.
c)Check a digoxin level.
d)No change in the patient's workup.
e)Start an intravenous lidocaine drip if the patient has > 6 consecutive beats of the same fast rhythm.
d)No change in the patient's workup.
The rhythm strip shows AF with Ashman phenomenon. Ashman phenomenon is easily confused with a run of premature ventricular contractions, a mistake that can lead to significant treatment errors. The right bundle branch block (RBBB) morphology of the aberrant beats preceded by a long-short cycle of AF beats gives away the diagnosis of Ashman phenomenon. Ashman phenomenon does not require any treatment.
Ashman phenomenon consists of an intermittent bundle branch block after a long–short cycle sequence in a patient with AF. Ashman phenomenon is the result of the heart's beat-by-beat variation in the duration of its refractory period: the longer the immediately preceding cycle, the longer the subsequent refractory period. Therefore, abrupt prolongation of an immediately preceding cycle, followed by an early next beat (the classic long–short cycle pattern of Ashman phenomenon) can lead to a situation where the early next beat encounters a still partly refractory heart from the preceding long cycle beat. This can trigger a run of aberrant RBBB beats. The so-called Ashman beats usually have an RBBB morphology because, in the healthy heart, the right bundle is the last infranodal system to completely repolarize. Only the RBBB of the first QRS reflects the Ashman phenomenon. The aberration is then briefly perpetuated for a variable number of beats by concealed trans-septal activation from the left bundle to the right bundle, with a brief block to the anterograde conduction of the next few sinus impulses in the right bundle.
The run of aberrant beats in Ashman phenomenon is also occasionally misinterpreted as containing delta waves, leading to an erroneous diagnosis of an accessory pathway (ie, Wolf-Parkinson-White syndrome) with an intermittent, antidromic re-entry rhythm (the run of fast beats). This misinterpretation leads to the unnecessary avoidance of atrioventricular-nodal-blocking agents. These agents could induce ventricular fibrillation in a patient who truly has an accessory bypass tract but do not need to be avoided in a patient with Ashman phenomenon. Incidentally, the patient's history of taking digoxin is another clue that the presence of a concealed accessory pathway is unlikely because digoxin is contraindicated in patients with pre-excitation syndromes.
Digitalis toxicity can present with many rhythms, but Ashman phenomenon is not one of them.
A 61-year-old man has been hiking on the Appalachian trail northbound from Georgia through North Carolina, Tennessee, Virginia, and West Virginia for the last month. Five days ago he developed fever, chills, headache, myalgia, nausea, vomiting, and diarrhea. After admission, he became hypotensive and went into respiratory failure.
Laboratory findings include a white blood cell count of 27,300/mm3, a hemoglobin level of 20.0 g/L, a platelet count of 65,000/mm3, and a creatinine level of 6.8 mg/dL. A chest X-ray revealed bilateral diffuse infiltrates.
The most likely source of this infection is which of the following?
A) arthropod bite
B) contact with water contaminated with animal urine
C) contact with bat droppings
D) inhalation of contaminated dust
E) contact with rodent excreta
E)
Correct!
This patient has Hantavirus pulmonary syndrome (HPS) caused by the Sin Nombre virus. Human infection occurs when a person inhales droplets of urine, saliva, or respiratory secretions from rodents. Ingesting food contaminated with rodent secretions or the contamination of cutaneous injuries have also been described.
Other hemorrhagic fevers, such as yellow and dengue fevers, may be transmitted via mosquitoes, but they will not be acquired in North America. Leptospirosis is transmitted by contact with water contaminated with animal urine, and it is common among athletes and adventure travelers. Histoplasmosis may be acquired by contact with bat droppings. Q fever and coccidioidomycosis can occur after a person inhales contaminated dust.
Sin Nombre is the prevalent virus that causes HPS in North America, whereas the Andes virus is more common in South America. The disease usually presents with a prodrome of fever and unspecific symptoms. It is then followed by rapidly progressive, noncardiogenic pulmonary edema and marked hemoconcentration, with a hemoglobin level around 20 mg/dL.
A 16-year-old boy who has just moved into your school district from Central America comes to you for medical clearance prior to playing football at his high school. Other than "typical" childhood diseases, his medical history is unremarkable. He is physically active, with no history of dyspnea on exertion and no history of cyanosis.
On physical examination, you detect a widely split second heart sound without respiratory variation and a soft systolic ejection murmur (grade 2/6) in the pulmonary area at the upper left sternal border. (Assume that these findings represent the most common asymptomatic type of congenital heart disease [CHD] in adults.)
What would you expect to find on electrocardiography (ECG) in this asymptomatic youth?
a)left-axis deviation and first-degree atrioventricular block
b)RSR' pattern, incomplete right bundle branch block, ± right-axis deviation
c)right ventricular hypertrophy
d)Leftward frontal plane P wave axis
b)RSR' pattern, incomplete right bundle branch block, ± right-axis deviation
Key Points:
ASD is commonly associated with an RSR’ pattern consistent with enlargement of the right ventricular outflow tract.
Explanation:
Atrial septal defect (ASD) is the most common type of CHD encountered in adults, accounting for up to 15% of all adult cases of CHD. Overall, ASD is the third most common type of CHD, occurring as an isolated anomaly in 5% to 10% of all congenital heart defects. About 30% to 50% of children with congenital heart defects have an ASD as part of their cardiac defect. The incidence is higher in females; combined with the common ostium secundum defects, the female to male ratio is 2:1.
In a patient without cyanosis, clubbing, or edema, it is reasonable to conclude that any right-to-left shunt is hemodynamically insignificant. Hence, the findings on ECG are minimal. The findings described are representative of an ostium secundum defect, which is the most common ASD. Patients with an ostium primum defect typically have right bundle branch block with left axis deviation. In patients with a moderate or large secundum ASD, the presence of an RSR' pattern on EKG predicts the need for intervention. This pattern reflects enlargement of the right ventricular outflow tract, which is the last portion of the ventricle to depolarize. The P wave axis is typically normal with secundum ASDs. In comparison, sinus venosus ASDs are often associated with a leftward frontal plan P wave axis (negative in leads III and aVF, positive in lead aVL) due to an ectopic pacemaker from an ASD near the sinus node.
Left-axis deviation and first-degree atrioventricular block are not seen with simple ostium secundum defects. They are more common with ostium primum defects and more complex syndromes. In the absence of a large shunt and pulmonary hypertension, right ventricular hypertrophy does not occur.
A 28-year-old man is referred to you for management of a recent diagnosis of HIV infection. The HIV infection was discovered when he was receiving treatment for hospital-acquired Mycobacterium tuberculosis infection leading to tuberculosis (TB), during which time the patient was prescribed isoniazid, rifampin, ethambutol, and pyrazinamide. The patient has been on the anti-TB regimen for 2 weeks.
He is new to the area and has recently undergone some initial laboratory testing from an infectious disease specialist he saw briefly without follow-up after the drastic improvement of the symptoms of his TB. You are able to view those previous laboratory results, which are as follows:
HIV enzyme-linked immunosorbent assay: Positive
HIV Western blot: Positive
CD4 count: 50 cells/µL
Quantification of HIV RNA: 80,000 copies/mL
HLA-B*570: Negative
Tuberculin skin test: Negative
His current medications consist of combination antiretroviral therapy (ART) (abacavir [ABC]/zidovudine [AZT]/lamivudine [3TC]) in addition to the anti-TB regimen.
The patient’s current available laboratory values using the electronic medical records are as follows:
CD4 count: 250 cells/µL
Quantification of HIV RNA: 10,000 copies/mL
Tuberculin skin test: Positive
On examination, the patient has dyspnea, which he states has been progressively worsening the past few weeks. The patient’s temperature is 39.0 °C, and he mentions that the symptoms initially present during his TB infection are returning.
Which of the following is the most likely mechanism of this phenomenon in this particular patient?
A) He experienced a drug hypersensitivity reaction to ABC in his current ART (ie, ABC/AZT/3TC).
B) The pathophysiology stems from a progressive increase in the proportion of T cells, which are recent thymic emigrants, with subsequent changes in the cytokine microenvironment.
C) The initiation of ART resulted in an unmasking-type TB immune reconstitution inflammatory syndrome (IRIS) because this current infection is currently subclinical.
D) Immune reconstitution inflammatory syndrome (IRIS) occurs in the setting of unmanaged HIV infection with resulting immunosuppression and subsequent antigen accumulation due to impeded phagocytic cell function from insufficient signaling from T cells, coupled with the rapid reversal of this physiologic state started after the initiation of ART and the reinstitution of immune function.
D)
Immune reconstitution inflammatory syndrome (IRIS) occurs in the setting of unmanaged HIV infection with resulting immunosuppression and subsequent antigen accumulation due to impeded phagocytic cell function from insufficient signaling from T cells, coupled with the rapid reversal of this physiologic state started after the initiation of ART and the reinstitution of immune function.
Unmanaged HIV infection with resulting immunosuppression and subsequent antigen accumulation due to impeded phagocytic cell function from insufficient signaling from T cells, coupled with the rapid reversal of this physiologic state after starting ART and reinstitution of immune function, may result in IRIS.
Explanation:
The mechanism of IRIS may differ somewhat depending on the etiology of the infectious agent involved. The general mechanism entails immunosuppression due to HIV infection, particularly when CD4 counts are 50 cells/µL. Initiating ART therapy in patients naïve to ART results in the prompt reinstitution of the immune system and its various mediators, leading to an inflammatory response. This general mechanism may be applied to various opportunistic infections in patients with HIV/AIDS, with the general idea that the pathophysiology will be slightly different. In cases involving Mycobacterium, there are 2 types, referred to as paradoxical TB-IRIS and unmasking TB-IRIS. Because the patient is currently undergoing therapy for TB, in this scenario it is referred to as paradoxical TB-IRIS. The mechanism entails an antigen accumulation due to impeded phagocytic cell function from insufficient T-cell signaling. When ART is initiated, T-cell function may rapidly return, resulting in the overstimulation of phagocytic cells that mount an exaggerated response toward the accumulation of antigen--thereby causing the release of a large amount of inflammatory mediators (ie, chemokines), which may mimic the initial infection with TB. TB-IRIS should be on the forefront of the clinician’s mind, because it may occur in up to 48% of patients started on ART midway through a TB regimen. TB-IRIS may be challenging to diagnose, although a careful history goes a long way. Characteristics such as a negative tuberculin skin test, which converts to positive after ART; improvement of TB symptoms during the course of the TB regimen with deterioration and return of infectious complications at approximately 1 week after the introduction of ART; CD4 count of no more than 50 cells/µL with a high viral load; and a dramatic response to ART are all characteristics worth noting. Therapy for IRIS consists of the administration of nonsteroidal anti-inflammatory drugs or steroids.