A 46-year-old man who has not seen a health care provider in many years presents for follow-up after a required preemployment electrocardiogram (figure). He has no notable medical history, feels well, and does not use tobacco or alcohol. He takes no medications.
His blood pressure is 190/105 mm Hg, and his heart rate is 75 beats per minute. Cardiac examination reveals a sustained apical impulse and no audible murmurs. His kidney function and serum electrolyte levels are normal.

Which one of the following diagnoses is most likely in this case?
A) Renal artery stenosis
B) Pheochromocytoma
C) Hypertrophic cardiomyopathy
D) Aortic stenosis
E) Primary hypertension
E) Primary hypertension
This asymptomatic patient has primary hypertension, with electrocardiographic evidence of left ventricular hypertrophy (LVH). A sustained apical impulse indicates that LVH is present. The patient’s echocardiogram would be likely to show thickened LV walls and an elevated LV mass index.
A 67-year-old woman with a history of hypertension and stage 3 chronic kidney disease related to lupus nephritis is hospitalized for evaluation of melenic stools that she has had for 2 days. Her current medications are hydrochlorothiazide 25 mg daily and mycophenolate mofetil 750 mg twice daily. Her serum creatinine level, measured 2 months ago, was 1.6 mg/dL (reference range, 0.6–1.1).
Current vital signs include a blood pressure of 100/55 mm Hg and a heart rate of 120 beats per minute. On examination, the patient has dry oral mucosa and flat jugular veins. Rectal examination reveals dark stool that is positive for occult blood. Urine output averages 30 mL per hour for the past 6 hours.
Urinalysis shows <2 red cells per high-power field (0–2); 2 white cells per high-power field (0–2); and 20–30 hyaline casts per low-power field (0–5).
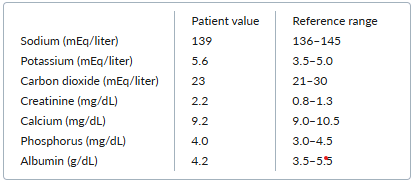
Laboratory testing yields the following results: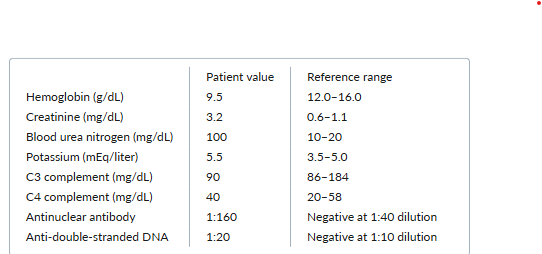
Which one of the following management strategies is most appropriate for this patient’s acute kidney injury?
A. Initiate hemodialysis
B. Start intravenous normal saline
C. Initiate antithymocyte globulin
D. Administer intravenous furosemide
E. Administer intravenous methylprednisolone
A 35-year-old woman with common variable immunodeficiency treated with intravenous immunoglobulin once monthly for 3 months presents with night sweats and a 6.8-kg weight loss during the past few months. A systems review is otherwise unremarkable.
The patient is afebrile but has a chain of enlarged cervical lymph nodes, each 2 to 3 cm in diameter. There is no evidence of lymphadenopathy in other locations.
What is the most likely diagnosis in this case?
A. Tuberculosis
B. Delayed-type hypersensitivity
C. Listeriosis
D. Non-Hodgkin lymphoma
E. Ehrlichiosis
D. Non-Hodgkin lymphoma
Common variable immunodeficiency syndrome is a rare condition that is often initially missed by medical practitioners. Common symptoms include recurrent sinusitis, diarrhea, and pneumonias. Patients with this condition have an increased risk of cancer, particularly non-Hodgkin lymphoma. In one study, the risk of developing non-Hodgkin lymphoma was estimated to be 438 times higher in women with common variable immunodeficiency than in women without it, after adjustment for age.
Immunoglobulin treatment does not appear to alter the risk for non-Hodgkin lymphoma in patients with common variable immunodeficiency syndrome.
A 30 year old woman with type 2 DM and obesity reports pain in the area of the left anterolateral hip and thigh that has been present for a few months but has worsened during the past few weeks. The pain is moderate and burning in character. She states she has sustained no injury to that area. She is able to walk without difficulty.
On examination, her vitals are normal. She has normal lumbar flexion, negative straight leg raise test, and no edema or tenderness on palpation to the left lateral hip or midthigh. On neuro exam, she has normal strength, but a loss of sensation in the left anterolateral thigh.
What is her most likely diagnosis?
Meralgia paresthestica
Symptoms and examination suggest meralgia paresthetica, which is caused by the entrapment of the lateral femoral cutaneous nerve at the inguinal ligament. Risk factors for the condition include obesity, type 2 diabetes, older age, and tight-fitting garments. The lateral femoral cutaneous nerve is a purely sensory nerve that innervates the skin on the anterolateral hip to midthigh.
A 77-year-old man presents with frequent dizziness on standing from a seated position. He has type 2 diabetes, stable coronary artery disease, and benign prostatic hyperplasia. His current medications are finasteride 5 mg daily, doxazosin 2 mg daily, atenolol 50 mg daily, simvastatin 40 mg daily, metformin 1000 mg twice daily, and aspirin 81 mg daily.
His current resting blood pressure is 128/80 mm Hg, and he has a heart rate of 65 beats per minute. After standing for one minute, his blood pressure is 100/60 mm Hg, and he has a heart rate of 72 beats per minute. Examination of the heart and lungs is normal. An electrocardiogram is also normal.
Which one of the following changes in this patient’s medical regimen would be most appropriate?
A) Discontinue doxazosin
B) Initiate fludrocortisone
C) Discontinue atenolol
D) Discontinue finasteride
E) Increase salt and water intake
A) Discontinue doxazosin
Alpha-1-adrenergic antagonists, which relax smooth muscle in the prostate and bladder neck, are often prescribed for patients with benign prostatic hyperplasia; however, orthostatic hypotension is a relatively common side effect with two such agents — doxazosin and terazosin. Several other alpha-blockers (tamsulosin, alfuzosin, and silodosin) are more selective for prostate tissue and are thought to cause less orthostatic hypotension than doxazosin or terazosin. Doxazosin should be discontinued in a man with symptomatic orthostatic hypotension. If the orthostasis resolves and urinary symptoms worsen, a cautious trial of one of the selective agents could be considered.
A 68-year-old woman is evaluated for an elevated serum creatinine level. The finding was detected during an outpatient workup for progressive edema, which began as mild swelling several months ago. Her medical history includes hypertension, hypothyroidism, osteoarthritis, and fibromyalgia. Her medications are hydrochlorothiazide 25 mg daily, amlodipine 5 mg daily, levothyroxine 75 μg daily, and ibuprofen 600 mg twice daily.
On examination, her blood pressure is 133/64 mm Hg, her heart rate is 86 beats per minute, and her respiratory rate is 14 breaths per minute. Her cardiopulmonary examination is normal. Anasarca is present.
On laboratory testing, her serum creatinine level is 1.7 mg/dL (reference range, 0.6–1.1), her albumin level is 2.3 g/dL (3.5–5.5), and her potassium level is 4.9 mEq/liter (3.5–5.0). Urine microscopy shows 15 to 20 white cells per high-power field (0–2), and her 24-hour urine protein excretion is 6400 mg/24 hours (<150).
Which one of the following initial management approaches is most appropriate for this patient?
A. Initiate diuresis with spironolactone
B. Initiate treatment with prednisone
C. Discontinue the ibuprofen
D. Discontinue the amlodipine
E. Order a renal Doppler ultrasound
C. Discontinue the ibuprofen
This patient has symptoms of nephrotic syndrome, but she has also had a decline in kidney function, and the urine test results are suggestive of acute interstitial nephritis. This constellation of symptoms can occur with use of nonsteroidal antiinflammatory drugs (NSAIDs), which can lead to either disorder or cause both simultaneously. Nephrotic syndrome linked to the use of NSAIDs may be a manifestation of either minimal change disease or membranous nephropathy. Discontinuation of the NSAIDs is critical to the management of this disorder.
Imaging and renal biopsy should be pursued if the patient does not improve promptly after discontinuing the ibuprofen.
A 73-year-old man reports a 6-month history of recurrent low-grade fevers, a 3-month history of abdominal fullness, and a 6-week history of fatigue and moderately reduced exercise tolerance. He was previously in overall good health.
On examination, he appears well and in no acute distress. His heart rate is 95 beats per minute, and his blood pressure is 132/64 mm Hg. He has several palpable cervical and axillary lymph nodes (1 to 2 cm) that are nontender and freely mobile. He has a palpable spleen tip with inspiration. No hepatomegaly or abdominal masses are present. The remainder of his physical examination is normal.
Laboratory results are as follows:
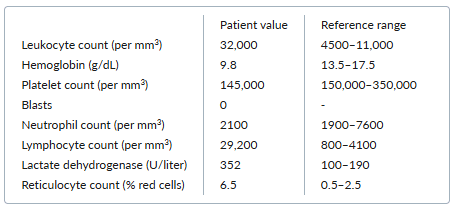
The peripheral-blood smear reveals increased numbers of mature-appearing lymphocytes, increased numbers of spherocytes, and polychromasia.
Which one of the following diagnoses is the most likely cause of the anemia noted in this case?
A. Replacement of the bone marrow with chronic lymphocytic leukemia
B. Myelofibrosis with extramedullary hematopoiesis
C. Pure red-cell aplasia
D. Microangiopathic hemolytic anemia
E. Autoimmune hemolytic anemia
E. Autoimmune hemolytic anemia
Autoimmune hemolytic anemia occurs in 10% to 20% of patients with CLL and does not depend on disease stage. In a patient with CLL, an elevated lactate dehydrogenase level, reticulocytosis, and polychromasia (the term for reticulocytosis as seen on the peripheral smear) suggest a diagnosis of autoimmune hemolytic anemia. The presence of anemia based on autoimmune hemolysis in CLL does not convey the poorer prognosis associated with anemia caused by marrow replacement.
A 76 year old woman with a history of hypertension and hyperlipidemia is hospitalized with pain and swelling in her right wrist. Her symptoms worsened since they started 2 days ago. She reports no fever, chills, skin rash, diarrhea, dysuria, or tick bites. Two years ago she had a similar episode in her left wrist that resolved with NSAIDs.
On examination, she is afebrile. Her wrist is warm, swollen, and erythematous, with markedly limited range of motion. Laboratory testing reveals a leukocyte count of 8200 per mm3 and a uric acid level of 7.0 mg/dL. A radiograph of the right wrist is obtained.

Which one of the following diagnoses is most likely in this case?
A) Acute calcium pyrophosphate crystal arthritis (pseudogout)
B) Reactive arthritis
C) Lyme arthritis
D) Septic arthritis
E) Gout
A) Acute calcium pyrophosphate crystal arthritis (pseudogout)
Acute calcium pyrophosphate (CPP) crystal arthritis, previously known as pseudogout, is a common cause of inflammatory monoarticular arthritis in older adults. It manifests similarly to gout, with self-limited acute attacks of monoarthritis characterized by joint pain, swelling, warmth, and redness. Acute CPP crystal arthritis can affect any joint, but the wrist and the knee are most often affected; in contrast, gout more commonly affects the foot.
Plain-film radiographs in patients with CPP deposition disease may reveal calcification of cartilage (chondrocalcinosis). However, chondrocalcinosis is frequently asymptomatic; therefore, arthrocentesis is indicated to confirm the diagnosis of acute CPP crystal arthritis.
An 83-year-old woman with long-standing hypertension comes to the emergency department (ED) because of concerns about very high blood pressure. She periodically checks her blood pressure at home and typically obtains readings of about 150/80 mm Hg. However, this morning, her blood pressure was 210/108 mm Hg; when she checked it 10 minutes later, it was 212/106 mm Hg. She does not report any symptoms. Her medications include hydrochlorothiazide 25 mg daily, losartan 100 mg daily, and amlodipine 5 mg daily.
On physical examination, her blood pressure is 196/102 mm Hg in the right arm and 198/100 mm Hg in the left arm. She has a regular heart rhythm and rate at 82 beats per minute and a grade 1/6 early systolic murmur at the right-upper-sternal border, with a slightly accentuated second heart sound. Her lung sounds are clear. She does not have papilledema.
Laboratory studies demonstrate a normal serum creatinine level, normal hemoglobin and hematocrit concentrations, a normal platelet count, and no troponin elevation. Urinalysis shows no evidence of proteinuria or hematuria.
An electrocardiogram is unchanged from the patient’s normal baseline.
Which one of the following management options is most appropriate for this patient?
A) Increase the dose of amlodipine, and discharge the patient home with outpatient follow up
B) Give oral hydralazine, and discharge the patient home after her blood pressure decreases
C) Give IV hydralazine, and admit the patient to the hospital for observation
D) Give oral lorazepam, and discharge the patient home
E) Give sublingual nitroglycerin, and discharge the patient home after her blood pressure decreases
A) Increase the dose of amlodipine, and discharge the patient home with outpatient follow up
Hypertensive urgency is often grouped with hypertensive emergency under the heading “hypertensive crises,” defined as a blood pressure (BP) >180/120 mm Hg. However, unlike hypertensive emergency, hypertensive urgency is characterized by the absence of end-organ compromise. Patients with hypertensive urgency and no symptoms can be managed with adjustment of long-acting medications and do not require immediate BP lowering, which carries the risk of causing cerebral hypoperfusion due to autoregulatory adaptations to chronic hypertension, especially in older adults.
A 38-year-old woman with a history of Raynaud phenomenon presents to the emergency department with severe headache, blurred vision, and confusion. She reports fatigue, arthralgias, and tightness and thickening of the skin on the arms and legs during the past 3 months.
Her blood pressure is 220/110 mm Hg, and her heart rate is 90 beats per minute. Physical examination reveals tightness of the skin on her fingers. Funduscopic examination shows arteriovenous nicking and flame-shaped hemorrhages. She is admitted to the intensive care unit.
Laboratory testing yields the following results:
The result of an antinuclear antibody test is positive, with a speckled pattern. Multiple schistocytes are present in a peripheral-blood smear. Urinalysis shows 1+ proteinuria, no blood, no cells, and no casts.
Which one of the following antihypertensive agents is most appropriate for managing this patient’s underlying condition?
A. Nicardipine
B. Esmolol
C. Furosemide
D. Captopril
E. Nitroprusside
A. Captopril
This patient with hypertensive emergency and historical and physical findings of scleroderma has scleroderma renal crisis (SRC). Multiple nonrandomized, uncontrolled retrospective, and prospective studies have shown that the use of angiotensin-converting-enzyme (ACE) inhibitors are associated with increased antihypertensive efficacy, increased preservation of kidney function, increased incidence of renal recovery with discontinuation of dialysis, and improved survival of patients with SRC (one-year survival rate, 76% vs. 18% without an ACE inhibitor).
Common features of SRC include malignant arterial hypertension, accelerated kidney failure, and markedly increased levels of plasma renin activity; hence, ACE inhibitors are mechanistically advantageous. Captopril may be particularly beneficial because of its rapid onset, and this agent has been used more than other ACE inhibitors in patients with SRC. ACE inhibitors may be used even in the setting of reduced kidney function and can be continued if the subsequent rise in serum creatinine level is modest.
An 82-year-old woman is brought to the hospital in a confused state. She describes a one-week history of progressive headache, lower-extremity numbness and tingling, and blurred vision.
She is afebrile, her blood pressure is 130/90 mm Hg, and her heart rate is 90 beats per minute. She is oriented to name only. Retinal examination is significant for dilated retinal veins. She has several areas of ecchymosis on her lower extremities.
She is up to date with Covid-19 vaccinations, and testing for SARS-CoV-2 is negative. Laboratory results are as follows:
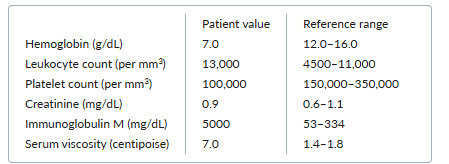
A bone-marrow biopsy demonstrates 30% infiltration by small plasmacytoid lymphocytes.
Which one of the following diagnoses is most likely in this case?
A. Chronic myeloid leukemia
B. Waldenström macroglobulinemia
C. Multiple myeloma
D. Non-Hodgkin lymphoma
E. Acute lymphoblastic leukemia
B. Waldenström macroglobulinemia
Hyperviscosity syndrome associated with Waldenström macroglobulinemia is caused by elevated levels of IgM, which causes impaired blood flow to the central nervous system. Symptoms of hyperviscosity include blurred vision, headache, dyspnea, neuropathy, retinal vein engorgement, and mental status changes. Treatment for hyperviscosity syndrome is urgent plasmapheresis to remove IgM from the circulation. The decision to initiate plasmapheresis is based on serum viscosity level, symptoms, and physical examination findings. Because 80% of IgM antibodies remain intravascular, plasmapheresis is an effective but temporary method of reducing viscosity.
- Multiple myeloma, characterized by plasma cells in the bone marrow, is usually associated with an immunoglobulin G paraproteinemia.
A 34 year old man is seen for a facial rash that began after a trip to the beach with his family a few weeks ago. He has also noticed pain in his knees and intermittent right-sided chest pain when he takes a deep breath but says acetaminophen has provided some relief. He has no fever or chills.
His medical history is notable for Crohn disease that has been well controlled on mesalamine for many years, but he currently has watery diarrhea once daily. He has bipolar disorder and was recently started on chlorpromazine after multiple other medications failed.
On examination, he has symmetric red plaques on his cheeks that extend over the nasal bridge and spare the nasolabial fold. Pulmonary exam is notable for diminished breath sounds at the right base with bronchial breath sounds in the mid-right lung field. Cardiac exam is without abnormality. The rest of the skin and joint examination is unremarkable.
Which one of the following tests is most likely to be positive in this patient?
A) Anti-Smith antibody
B) Anti-La antibody
C) Anti-double stranded DNA
D) Tissue transglutaminase immunoglobulin A antibody
E) Anti-histone antibody
E) Anti-histone antibody
This patient developed arthralgia, probable serositis, and a photosensitive malar rash that spares the nasolabial fold in the setting of a recent exposure to chlorpromazine. These features raise the possibility of drug-induced lupus. Other drugs commonly associated with drug-induced lupus include procainamide, hydralazine, minocycline, methyldopa, and tumor necrosis factor (TNF) inhibitors.
A 48-year-old man is hospitalized with weight gain, worsening lower-extremity edema, and increasing abdominal girth. His symptoms have progressed despite initiation of diuretic therapy 3 months ago. He was treated with chest radiation and chemotherapy for non-Hodgkin lymphoma at age 21.
On physical examination, he is afebrile and has a heart rate of 90 beats per minute, a blood pressure of 120/70 mm Hg, and an oxygen saturation of 97% while breathing ambient air. His jugular venous pressure is elevated and increases with inspiration, but cardiac and pulmonary examinations are otherwise unremarkable. The liver edge is palpable 3 cm below the costal margin, and he has 3+ pitting edema of the lower extremities.
Laboratory evaluation reveals a normal serum creatinine level, mildly elevated liver aminotransferase levels, and a total bilirubin concentration of 2.0 mg/dL (reference range, 0.3–1.0).
An abdominal ultrasound shows liver enlargement without obvious cirrhosis, as well as moderate ascites.
A transthoracic echocardiogram reveals normal left ventricular systolic function, with abnormal septal motion and a dilated inferior vena cava, without inspiratory collapse. During respiration, flow velocities across the tricuspid and mitral valves fluctuate substantially.
Which one of the following treatments is most appropriate for this patient?
A) Sildenafil
B) Transjugular intrahepatic portosystemic shunt
C) Surgical septal myotomy
D) Carvedilol
E) Pericardiectomy
E) Pericardiectomy
Peripheral venous congestion (elevated jugular venous pressure, anasarca, ascites, hepatic congestion) in the absence of pulmonary venous congestion in a patient with a history of chest irradiation is consistent with a diagnosis of constrictive pericarditis. Common causes of this condition include tuberculosis, previous cardiac surgery, acute pericarditis, autoimmune disease, and previous chest irradiation.
Physical examination findings in patients with constrictive pericarditis include Kussmaul sign (lack of decline or increased jugular venous distention with inspiration), pulsus paradoxus, and, less commonly, an audible pericardial friction rub or knock. A chest radiograph may reveal rimmed calcification around the heart, best seen on a lateral view of the chest. Echocardiographic findings include abnormal septal “bounce,” resulting from respiratory variation of septal motion, exaggerated respiratory variation in tricuspid and mitral inflow velocities, and a dilated inferior vena cava with minimal inspiratory collapse.
Pericardiectomy is the treatment of choice in a patient with chronic symptoms attributable to constrictive pericarditis that is refractory to conservative management (e.g., diuretics). Surgery should not be delayed in patients with constrictive pericarditis because advanced heart failure is associated with a high rate of operative mortality.
A 62-year-old man presents for routine follow-up. His history is significant for heart failure with a reduced ejection fraction of 45% due to ischemic cardiomyopathy, myocardial infarction 3 years ago, hypertension, chronic kidney disease stage 3 with severely increased albuminuria, and type 2 diabetes. He has previously met with a dietician and currently adheres to a low-potassium diet. He also reports adherence to his current medications: chlorthalidone 25 mg daily, empagliflozin 10 mg daily, and lisinopril 20 mg daily.
He has a heart rate of 62 beats per minute, a blood pressure of 115/72 mm Hg, and a temperature of 37.2°C. On physical examination, he has moist mucous membranes. There is no evidence of ascites or pitting edema in the extremities.
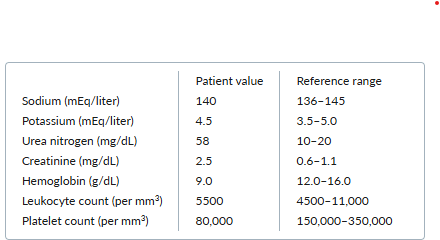
Laboratory tests obtained 2 weeks ago yield the following results:
Repeat laboratory testing at today’s visit shows similar results.
Which one of the following medication changes is most appropriate for this patient?
A. Initiate fludrocortisone
B. Initiate sodium bicarbonate
C. Discontinue lisinopril
D. Initiate torsemide
E. Initiate sodium zirconium cyclosilicate
E. Initiate sodium zirconium cyclosilicate
The most appropriate next step for this patient is to start an oral potassium binder, such as sodium zirconium cyclosilicate or patiromer. Both of these agents are nonabsorbable and bind potassium within the intestine, leading to enhanced excretion of potassium in the stool. Patiromer exchanges calcium for potassium, whereas sodium zirconium cyclosilicate exchanges both hydrogen and sodium, which likely explains the dose-dependent edema seen with this medication. Both agents have been associated with gastrointestinal symptoms, and patiromer also carries a risk of hypomagnesemia.
Another oral potassium binder that might be considered is sodium polystyrene sulfonate (SPS), a cation-exchange resin that binds potassium in exchange for sodium in the gut. It has traditionally been used for acute hyperkalemia and is often used in ambulatory patients, either as an emergency measure to avoid a visit to the emergency department or in small regular doses daily or several times a week. Despite its widespread use, SPS has only modest efficacy and has been associated with intestinal necrosis in numerous case reports and a higher risk of hospitalization for adverse gastrointestinal events. SPS can also interfere with the absorption of other medications, which is a challenge for patients taking multiple medications because they would need to take this agent at a separate time from the others. Finally, because of its high sodium content, SPS has the potential to contribute to volume overload. For these reasons, SPS is usually reserved for situations in which other options are not available and the serum potassium level cannot be controlled.
A 57-year-old man returns for evaluation after fine-needle aspiration of a spiculated, 3.6-cm peripheral right lung mass confirms a diagnosis of non-small-cell lung cancer. Symptoms of the lung cancer consisted of a persistent cough and occasional hemoptysis during the past 3 months. His medical history is significant for hypertension, hypothyroidism, and mild chronic obstructive pulmonary disease. His physical examination is unremarkable.
Combination positron emission tomography and CT reveals several right hilar and subcarinal lymph nodes, the largest measuring 1.2 cm, that are not 18 F-fluorodeoxyglucose-avid. No other enlarged lymph nodes or metastatic lesions are noted. An MRI of the brain reveals no evidence of intracranial metastases.
Which one of the following management steps is the most appropriate next step in this case?
A. Bronchoalveolar lavage
B. Surgical resection of the primary tumor and the lung lobe that contains it
C. Radiation of the primary lesion
D. Neoadjuvant chemotherapy
E. Mediastinoscopy and lymph-node sampling
E. Mediastinoscopy and lymph-node sampling
Determining the nodal stage is crucial for treatment decision-making in patients with T2 tumors, especially when the patient has suspicious lymph nodes on imaging, because the involvement of lymph nodes will alter treatment. Although positron emission tomography can help clarify the nature of lymphadenopathy, it is not sufficiently sensitive or specific to obviate the need for biopsy. Another method of assessing the mediastinal nodes is endobronchial ultrasound-guided transbronchial node aspiration. Some centers prefer this method of assessing the mediastinum. The key point is that the mediastinum must be assessed and found free of tumor to proceed with curative resection. Thus, of the answer options listed, mediastinoscopy and lymph-node sampling are the best choice.
• A patient whose lymph nodes are negative for cancer would have a T2aN0M0 stage IB lung cancer. Treatment is surgical resection (in operable candidates).
• Patients with positive ipsilateral lymph nodes would have a T2aN2M0 stage IIIA lung cancer. Multimodality therapy usually includes neoadjuvant treatment (chemotherapy with or without radiation) followed by surgery.
• Patients with positive contralateral lymph nodes would have a T2aN3M0 stage IIIB lung cancer, which is treated with a combination of chemotherapy and radiation therapy.
A 40-year old man presents to the ED with a 2 day history of right calf swelling and tenderness. He reports no chest pain, dyspnea, or history of immobilization or malignancy. He notes that he had similar symptoms in the left leg 5 years ago, which was diagnosed as a DVT and he was treated with 3 months of dabigatran.
On further history, he describes frequent aphthous ulcers, a few episodes of genital ulcers, and two episodes of uveitis. Some of the episodes of ulcers have been associated with knee and ankle swelling, but the patient denies any back pain. He reports he is sexually active in a monogamous relationship.
Three oral aphthae are evident on head and neck exam, and GU exam reveals a painful 2cm scrotal ulcer. The right calf is larger than the left calf, with a tender palpable cord.
Lab testing reveals a hemoglobin of 14 g/dL, ESR 50 mm/hr, and CRP of 40.5 mg/titer. The rest of the CBC and CMP are normal. Testing is negative for antiphospholipid antibody and beta 2 glycoprotein.
A vascular doppler of right leg reveals a DVT of popliteal and superficial femoral veins. The patient is started on dabigatran in the ED.
Which one of the following tests is most likely to be positive?
A) HLD B27
B) ANA
C) Testing for activated protein C resistance
D) Pathergy skin test
E) RPR
D) Pathergy skin test
The diagnosis of Behçet disease should be considered when a patient presents with oral aphthous ulcers and any of several systemic features. Although there are currently no widely accepted diagnostic criteria for this condition, an international team has proposed the system outlined in the table below whereby a score ≥4 indicates Behçet disease. Ethnic groups with higher rates of Behçet disease include those of Mediterranean or East Asian descent.
This patient presents with oral and genital ulcers, vascular thrombosis, and a history of uveitis and arthritis — and therefore meets the diagnostic criteria for Behçet disease. Foregoing the pathergy skin test may be reasonable, but if the test is performed, the likelihood of a positive result is around 50%. In addition to anticoagulation for deep-vein thrombosis, management of this patient’s Behçet disease could include any of the following treatments: glucocorticoids, colchicine or apremilast (both are especially effective for aphthous ulcers), methotrexate, and tumor necrosis factor inhibitors.
