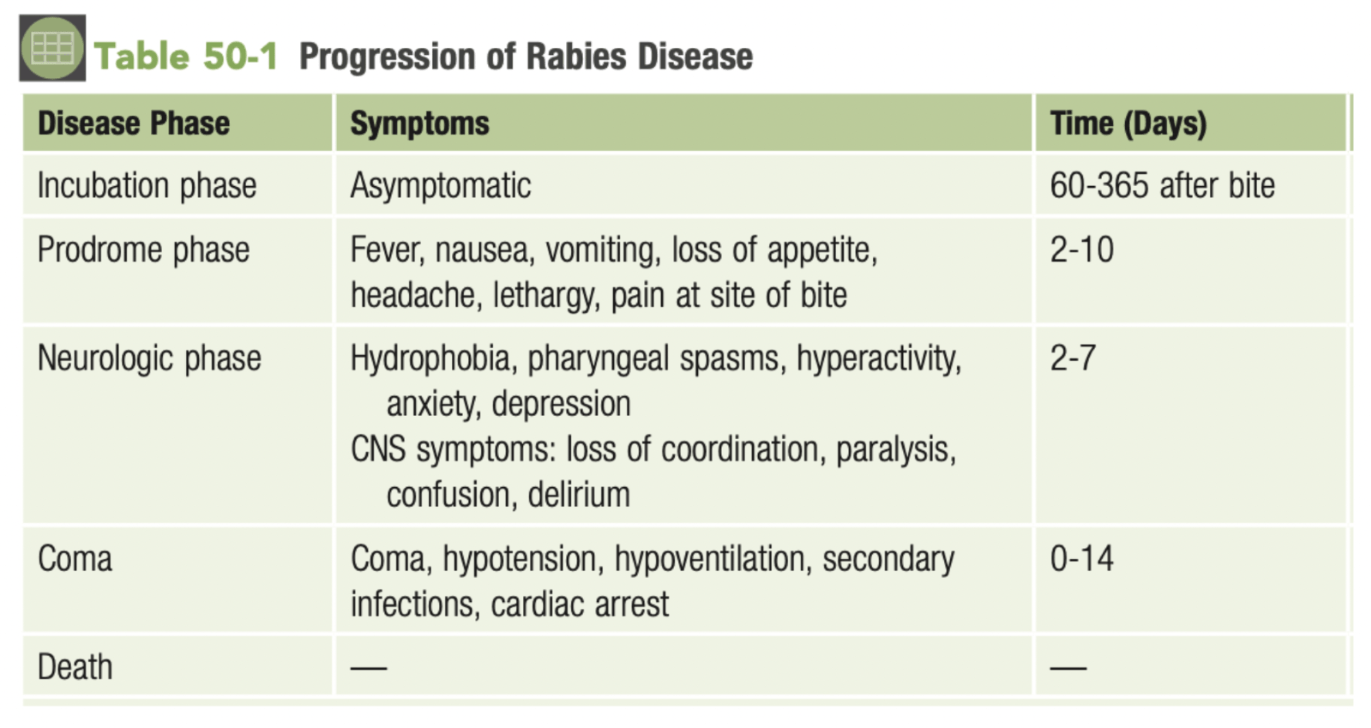
A 7-year-old boy presents to the emergency room with acute kidney failure. His initial lab work shows thrombocytopenia, and a blood smear shows:
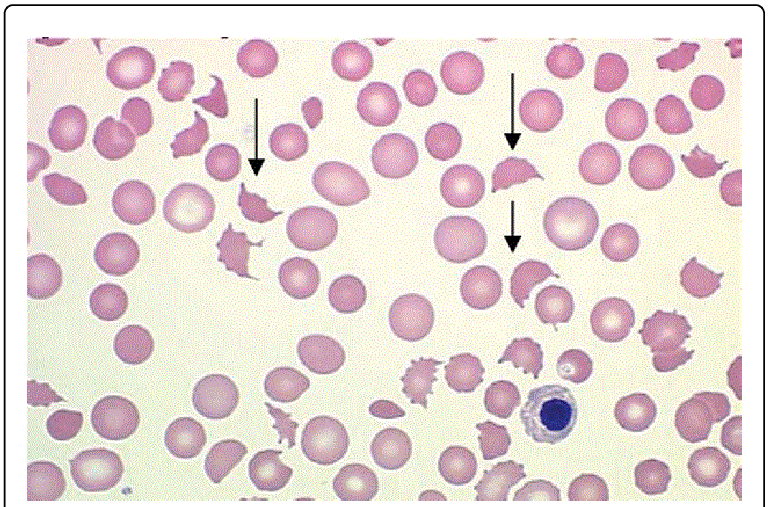
What complication of STEC is this patient experiencing?
Hemolytic uremic syndrome
Hemolytic uremic syndrome is a toxin mediated microangiopathic injury that causes a prothrombotic state and causes intravascular microthrombi. it is well known for its three classical features of acute kidney failure caused by the occlusion of renal vessels, thrombocytopenia, and hemolytic anemia as shown in the photo above.
A 30 y.o. woman presents to clinic with increased frequency of urination, burning sensation when urinating, and suprapubic abdominal pain. Laboratory testing reveals that the organism is a non-motile. coagulase-negative, non-hemolytic, and urease-positive. What is the likely cause of the infection?
Staphylococcus saprophyticus
Reasoning: S. saprophyticus is the second most common cause of urinary tract infections behind uropathogenic E. coli. While you can differentiate the two species based on gram stain, E. coli is also urease negative while S. saprophyticus is urease positive. Proteus mirabilis is also a cause of urinary tract infections and is urease positive but can be differentiated from S. saprophyticus as Proteus mirabilis is motile and gram-negative.
Fourteen hours after birth, a neonate develops fever, hypotension, tachypnea, apnea, lethargy, poor feeding and vomiting. The newborn genetic screening panel returned normal. The mother reports no family history of any metabolic disorders. During one of her prenatal care visits, she remembers a doctor telling her she was colonized with “a bacteria of some kind” but declined treatment. What is the likely causative agent of the newborn’s illness?
Group B streptococci (Streptococcus agalactiae)
Reasoning: Group B strep is a major cause of disease in neonatal and perinatal periods. Mothers who are colonized by Group B strep can pass on the organisms to their child during birth. If the neonate becomes ill, they will often develop meningitis, septicemia, and pneumonia.
45-year-old man presents to the ER for a five-week history of cough with bloody sputum. He is HIV positive and has lived in several homeless shelters in Omaha. He also reports having night sweats and chest pain. He remembers other people in the shelter having similar symptoms as him. You perform an acid fast stain which shows:
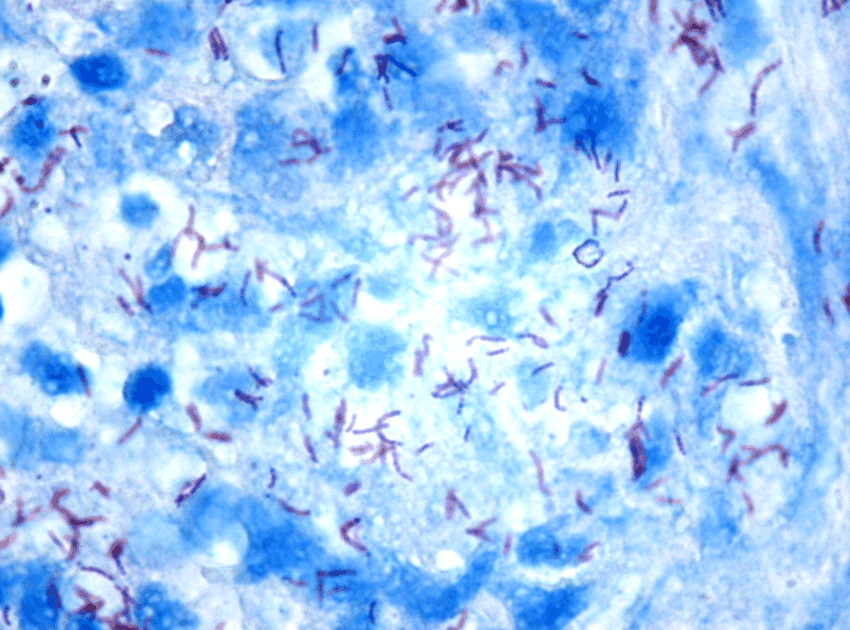
What organism is most likely responsible for his illness?
Mycobacterium tuberculosis
Reasoning: Mycobacterium tuberculosis is an acid-fast bacteria that causes cough with bloody sputum, night sweats, weight loss, chest pain, and fever. Living in close quarters like homeless shelters is a risk factor for getting TB as is being immunocompromised. Non-TB mycobacterium typically do not spread from person to person like TB does.
What species of Plasmodium are responsible for relapsing disease?
Plasmodium vivax and ovale
P. vivax and P. ovale invade liver cells where they go dormant in a Hypnozoite stage. Hypnozoites can reactivate and trigger a new presentation of infection.
A 40-year-old man has recently undergone a kidney transplant and takes immunosuppressant drugs to prevent organ rejection. Three weeks after his transplant, he reports feelings of fatigue, malaise, muscle aches, and gastrointestinal distress. A biopsy of his small intestine shows this image. Which pathogen is most likely causing this patient’s symptoms?
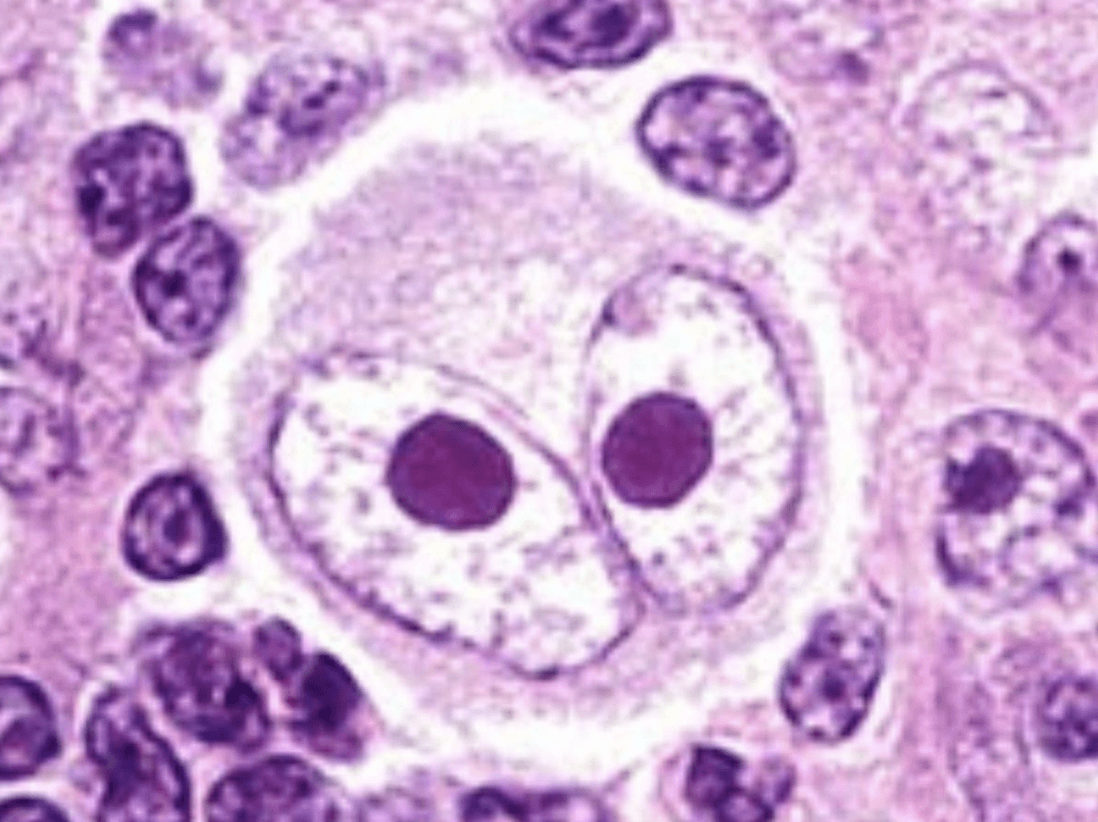
Cytomegalovirus (CMV)
CMV is very common – 90% of 80-year-olds have antibodies to the virus. Infection is usually asymptomatic; however, immunosuppressed patients can have severe manifestations ranging from nonspecific symptoms of viremia to end-stage organ disease and death. The patient in this vignette presents with nonspecific symptoms, but the biopsy shows an owl’s eye inclusion body, which is highly specific for CMV.
A 19 yo male presents to his PCP with concerns about an itchy rash. Upon closer inspection, the rash appears red and circular, with an area of clearing in the center. It is limited to the patient’s trunk. Scrapings of the rash also demonstrate hyphae on KOH wet mount. What is the causative agent of this rash?
Dermatophytes (Trichophytum, Epidermophyton, Microsporum)
Explanation: This is tinea corporis. The presentation is usually itchy ring-shaped scaly rashes. The name of the rash is based on the body site (capitis, cruis, pedis, etc.). Hyphae are the key finding on KOH mount. Sabourad agar can sometimes be used, but not often (time constraints of culture).
A 60-year-old patient in the ICU develops thick secretions from his endotracheal tube, fever and chills. He has a past medical history of COPD, hypertension and type 2 diabetes. When you collect his sputum it looks like: 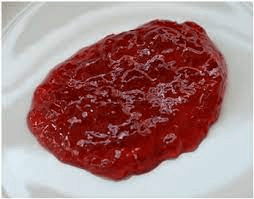
What is the virulence factor that the patient’s infection produces to cause ”currant jelly” sputum.
Polysaccharide matrix
Reasoning: This patient is suffering from nosocomial Klebsiella pneumoniae infection which classically presents with “currant jelly” sputum. The polysaccharide matrix produces a thick layer that prevents phagocytosis and causes an inflammatory response leading to necrosis in the lungs and the characteristic look of the sputum.
A 32-year-old arrives in clinic for a suspected UTI. She has had increased frequency of urination, back pain, increased urgency, and she has noted gross blood in her urine. An ultrasound was performed to look at her kidneys and staghorn calculi were noted. Lab work showed that the bacteria cultured was negative for lactose fermentation and negative for oxidase. What mechanism does this bacterium use that leads to struvite stones as seen in this patient?
Urease
Reasoning: The organism in this prompt is Proteus mirabilis. It classically causes UTIs as it infects the genito-urinary tract. It is known to produce large quantities of urease which hydrolyzes urea into ammonia and carbon dioxide. As it creates an alkaline environment it leads to the precipitation of phosphate, carbonate, and magnesium which leads to the characteristic struvite stones.
A 22 year old female patient arrives in clinic with a suspected UTI. She has an urgent, frequent need to pee, increased bladder fullness, burning while urinating, and pelvic pain. You take a urine sample and send it in for culture. The bacteria is found to be aerobic and have positive lactose fermentation. On gram stain it is revealed to be a gram-negative rod. What virulence factor does this organism have that allows it to colonize and invade the bladder?
P pili or P fimbriae adhesions
Escherichia coli is the most common cause of community acquired urinary tract infections (UPEC). It is heavily associated with ascending infections. It is a lactose fermenting bacterium. It uses adhesions to bind cells lining the bladder and upper urinary tract preventing bacterial elimination when urine is voided from the bladder.
You have a 23-year-old patient who contracted Mycobacterium tuberculosis when doing her emergency medicine rotation. Her X-ray showed the following:
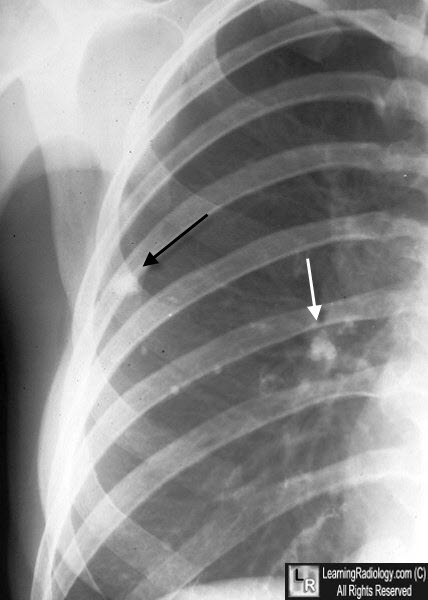
What is this classic finding of TB called?
Ghon complex
Reasoning: TB classically forms necrotizing granulomas. When there is a combination of a parenchymal granuloma and an involved hilar lymph node on the same side, the two together are called a “Ghon Complex”.
A 40 y.o female patient living in Egypt presents with painful and extreme swelling of her left lower extremity. It is determined that an infection with the organism W. bancrofti is the cause of her symptoms.
Where in the body do adult W. bancrofti worms live?
Lymphatics
This organism is Wuchereria bancrofti, which is transmitted via mosquitos. Once inside the body, adult worms live and proliferate inside lymphatic vessels, leading to the symptoms of lymphatic filariasis. Microfilaria produced by adult worms circulate inside the lymphatics as well as blood vessels, where they can be reingested by mosquitos.
A 36-year-old woman presents to her primary care physician with complaints of painful recurrent sores that appear on her lower lip. She shows this recent picture to her physician. Which type of cell does this pathogen reside in during its latent phase?

Sensory neurons (trigeminal ganglion)
This patient is infected with herpes simplex virus 1 (HSV-1). The alpha sub-family of human herpesviruses includes HSV-1, HSV-2, and varicella-zoster virus (VZV). Viruses of the alpha sub-family reside in sensory neurons in their latent phase (trigeminal ganglion for HSV-1), and cause pain in the local skin and mucous membranes during reactivation.
A 53 yo female presents to the ER with fever, cough, and chest pain that worsens with normal breathing. Upon getting an X-ray, nodular infiltrates are noted. When taking the patient’s history, the ER physician notes that she had recently traveled to Arizona to visit her sister. Her medication list includes etanercept, ibuprofen, and propanolol. What is the most likely agent responsible for the patient’s illness?
Coccidioides imitis
Explanation: Pt is presenting with pulmonary signs of a possible fungal infection. Nodular infiltrates and history of immunosuppression (etanercept) also raises this on the differential. History of travel to Southwest US would raise suspicion for Coccidioides.
Other important info: This fungus forms spherules in the tissue as part of its pathogenesis, which can help differentiate it from other fungi.
An 18-year-old male arrives to the emergency room with shortness of breath, extreme fatigue, productive cough that he reports steadily worsened over the past 12 hours. He has a past medical history of cystic fibrosis and several episodes of pneumonia. A sputum culture is ordered that grows green with a metallic sheen on Mueller-Hinton agar. The laboratory technician notes that the colonies smell like grapes. What is the main endotoxin that this organism produces that trigger cytokine pathways in its hosts?
Lipopolysaccharide
The patient in this scenario is infected with Pseudomonas aeruginosa which commonly is a cause of pneumonia in patients that are on ventilators and patients with neutropenia, burns, or cystic fibrosis. This organism classically grows a green/blue color that has a metallic sheen and these colonies smell “grape-like” or “corn tortilla-like". These are gram-negative organisms and have many molecules that contribute to pathogenesis, but in this case, lipopolysaccharide is an endotoxin that resists host defenses and often triggers cytokine pathways. Not to be confused with Exotoxin A which is responsible for disrupting protein synthesis by blocking peptide elongation.
A 68 y.o. male with a past medical history of asthma and a 40-pack year smoking history presents to clinic with cough, fatigue, fever, and chills. You obtain a gram stain that shows:
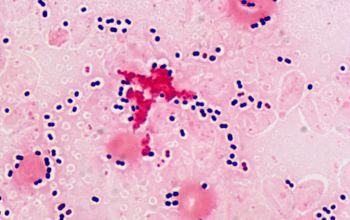
What is the main virulence factor produced by this organism protects it from host immunity?
Polysaccharide capsule
Reasoning: The organism shown by the gram stain is Streptococcus pneumoniae which is a gram-positive bacterium that is typically described as “lancet shaped” and found in diplococci. The polysaccharide capsule it produces makes it difficult for macrophages to phagocytose the organism. Streptococcus pneumoniae is a common cause of community acquired pneumonia, adult meningitis, sinusitis, otitis media, and bacteremia.
A 34-year-old woman comes to clinic complaining of joint pain in her knees, elbows and wrists. She tells you that she arrived in the U.S. three years ago from El Salvador and when asked tells you that she remembers having some throat infections as a child. Upon examination, she has a fever of 100 F and a systolic heart murmur on auscultation. What is the likely mechanism causing this woman’s symptoms?
Cross-reactive antibodies to Group A strep
This patient likely has rheumatic fever which is characterized by arthritis, fever, and heart failure but can also present with fatigue, and chorea (uncontrollable movements). Rheumatic fever develops when strep pharyngitis or scarlet fever infections are not treated, and the immune system develops cross-reactive antibodies that target healthy tissue. While it is not a common illness in the US, it remains relatively common in other countries.
A 55-year-old patient arrives to the emergency room with severe leg weakness. He has a past medical history of hypertension, asthma and untreated Mycobacterium tuberculosis infection. You perform an MRI of the spine and find:
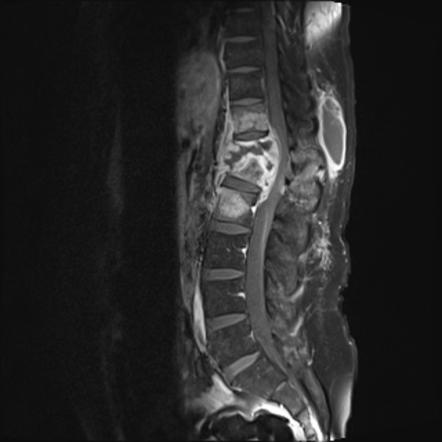
What complication of TB has this patient developed?
Pott’s Disease
Reasoning: While TB is classically a pulmonary disease, it has several extra-pulmonary symptoms including bone infection, especially in the spine. This can lead to bony destruction as what is depicted above.
This organism uses snails as an intermediate host in its life cycle and invades humans directly via skin. What is the most common mechanism of exposure of this parasite?
Contact wtih unclean water
Schistosoma mansoni has its eggs deposited in water sources. From here, the larvae hatch and migrate to snails where they develop into cercariae. After leaving the snails they must find a human host via chemotaxis in order to survive. If successful, they enter the unbroken skin and a male and female mate in the liver, before traveling to the intestines to deposit their eggs. Illness includes Katayama fever (fever, flu-like ssx, swollen lymph nodes, hepatosplenomegaly; hypersensitivity to antigens), granulomas, portal HTN from fibrosis, and GI hemorrhage.
A 3-month-old infant presents to the emergency department with intermittent apnea. His parents state that he started attending a new daycare three weeks ago and has been showing signs of lethargy and poor appetite for the past four days. Which pathogen is most likely responsible for this infant’s illness?
Respiratory syncytial virus (RSV)
Explanation: Although RSV can infect people of any age, it is most common and often most severe in infants < 6 months of age. The classic presentation of RSV in infants includes poor appetite, irritability, and lethargy. In severe cases, it can cause apnea. Another clue for RSV in this vignette is the fact that the infant started at a new daycare recently – RSV is transmitted through direct contact of mucous membranes with infectious respiratory droplets.
A 34 yo HIV positive male with a CD4 count <100 presents to clinic concerned about new dysphagia. Most of the physical is normal, except for white plaques noted in the patient's oral cavity, which are removed and bleed upon scraping. After being referred for swallowing difficulties, endoscopy shows similar white plaques along the esophagus as well. Upon visualization, yeast and psuedohyphae can be visualized. What is the causative agent of this patient’s dysphagia?
Candida albicans
Reasoning: white plaques in the oral cavity that you can scrape off are a key physical finding. Additionally, esophagitis is another clinical presentation of candida infections which is usually confirmed with endoscopy. Yeast and pseudohyphae are the typical pathological description of candida species. Another clue is that the patient has a CD4 <100 (level associated with infections like esophageal candidiasis)
A 23 y.o. male presents to the emergency room with a 24-hour history of fever, chills, abdominal pain, vomiting and confusion. His mother tells you that he had surgery to remove his gallbladder last week. The patient has a 102 F fever and a BP of 80/50. Upon physical examination, the patient has a diffuse, red, macular rash resembling a sunburn with peeling skin shown in the picture below: 
What toxin is most likely responsible for this patient’s symptoms?
Toxic Shock Syndrome Toxin 1 (TSST1)
Reasoning: Staphylococcus toxic shock syndrome is characterized by rapid onset of fever, rash, hypotension and multiorgan involvement. While classically associated with tampon use, it can also occur with recent surgery, or recent cellulitis. The picture depicts scalded skin syndrome which is induced by toxin damage to the skin causing blisters that frequently rupture. While Group A strep can also cause toxic shock syndrome, the “sunburn like rash” is only occasionally seen in Group A strep toxic shock syndrome.
You have a 40-year-old patient in clinic who has recently returned from Mexico with a weeklong history of non-bloody diarrhea and abdominal pain. He reports only drinking bottled water however he does recall eating fresh fruits and vegetables while on the beach. He denies fever and chills. Which of the toxins the organism produces binds to the intestinal receptor guanylyl cyclase C?
Heat stable enterotoxin
This patient likely received enterotoxigenic E coli from eating fruits and vegetables washed with contaminated water. This is likely as he has recently traveled abroad. Enterotoxigenic E coli produces 2 enterotoxins the first one is heat stable enterotoxin which binds to guanylyl cyclase receptor causing hypersecretion of fluids and inhibition of fluid absorption. The second is heat labile enterotoxin which interacts with a membrane protein (Gs) that upregulates adenylyl cyclase to increase cAMP, and thus Cl- secretion.
You have a patient in the ICU who is being treated for S. aureus bacteremia with clindamycin. After 3 days of therapy, the patient develops abdominal pain, distention and severe diarrhea. A glutamate dehydrogenase antigen test returns positive. What medication would you give to treat this patient’s infection?
Oral vancomycin
Reasoning: This patient developed severe diarrhea in a hospital setting after receiving antibiotics (particularly clindamycin) is a classic patient presentation of Clostridioides difficile. A positive glutamate dehydrogenase antigen test is a highly sensitive test that detects the presence of C. difficile but does not discern toxigenic vs. non-toxigenic strains. Given the patient’s symptoms and history though, you would treat by discontinuing clindamycin, give supportive care and oral vancomycin.
A 45-year-old male arrives in clinic with a chief complaint of skin lesions. Upon physical exam you find a sporotrichoid pattern of lesions like so: 
You order microbiological testing and find acid fast bacteria. What is the most likely cause of this patient's infection?
Mycobacterium marinum
Reasoning: Mycobacterium marinum is an acid-fast organism that commonly follow minor trauma or inadvertent inoculation that led to “fish tank granulomas” as shown in the picture above. The organism produces specific membrane lipids that recruit permissive macrophages to the site of infection which allow the bacteria to spread.
A 24-yo female who recently immigrated from Nigeria presents to your clinic for fever, malaise, and myalgia. Upon ordering a CBC, you also find that she has a hemoglobin of 10.1. A giemsa-stained blood smear is completed, and shows the following:
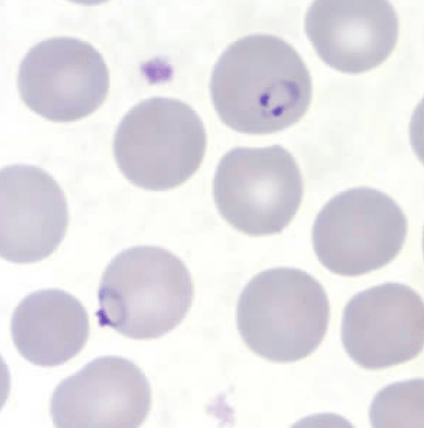
What lifecycle stage of the pathogen is observed in this stain?
Trophozoite
Malaria generally presents with ssx of fever, malaise, myalgia, headache, and mild anemia. The blood smear also shows the rings they form in RBCs as part of their life cycle. Giemsa-stained smears can be used to help in ID'ing the species.
The trophozoite form is observed inside red blood cells and represents the feeding stage of the parasite. Schizonts are the the replicating stage and rupture to release merozoites, which continue infection. Hypnozoites are observed in P. vivax and ovale and infect liver cells, causing relapsing infection
A 24-year-old woman was bitten by a stray dog during a trip to Madagascar. Three months later, her roommate brings her to the emergency department. She presents with hydrophobia, pharyngeal spasms, lack of coordination, and confusion. Based on her clinical presentation and travel history, an infectious disease physician diagnoses her with rabies. Considering the natural course of rabies, which disease stage was this patient in when she presented to the emergency department?
Neurologic phase
There are four phases of rabies disease: incubation, prodrome, neurologic, coma, and death. Summaries of each phase are included in the image. The patient in this vignette is in the neurologic phase due to her distinct symptoms of hydrophobia, pharyngeal spasm, lack of coordination, and confusion.
A 44-yo woman present to clinic with recent concerns about changes in skin coloration. During her physical exam, you note areas of hyperpigmentation which also fluoresce under Wood’s Lamp. Upon taking skin scrapings, what would you expect to see on a KOH prep?
Clusters of yeast cells and long hyphae (“spaghetti and meatballs”)
Explanation: Hyperpigmentation or hypopigmentation (tinea versicolor) is the typical presentation for malassezia furfur (neonates and those on TPN can get funginemia). Additionally, the patches fluorescing under wood’s lamp is a key point in the physical (dermatophytes can also fluoresce). “Spaghetti and meatball’ is the typical described appearance due to the mix of yeast cells and longer hyphae on KOH wet mount.
A 65-year-old patient on a ventilator due to complications from bacterial pneumonia developed thick secretions from his endotracheal tube. He has been diagnosed with stage II renal cell carcinoma and has been on a chemotherapy regiment for the past 4 months. A sample from the endotracheal tube is sent to the lab for an initial gram stain and culture. The lab report shows that the organism is a gram-negative rod with uniform staining that is non-lactose fermenting, and oxidase negative. What is the likely identity of this organism?
Stenotrophomonas maltophilia
Reasoning: Stenotrophomonas maltophilia typically causes a wide range of opportunistic infections in hosts and fits the lab characteristics presented. Pseudomonas aeruginosa is oxidase positive. Acinetrobacter baumannii are coccobacilli typically found as single cells or in pairs.
A 55-year-old woman has come into clinic today for concerns about her peripherally inserted central catheter (PICC) line. The patient receives regular doses of chemotherapy to treat her medullary thyroid cancer. Upon examination, the area around the PICC line insertion site is erythematous, hot to the touch, and has purulent exudate. You collect a sample from the line and send it to the medical microbiology lab for analysis. Labs reveal large, gram-negative coccobacilli arranged in pairs. It does not ferment lactose and is oxidase negative. What is the likely identity of this organism?
Acinetrobacter baumannii
Acinetrobacter baumannii fits the description above and is typically associated with ventilator-associated pneumonia, central line associated infections, and skin and soft tissue infections. Stenotrophomonas maltophilia is a gram-negative rod. Pseudomonas aeruginosa is oxidase positive.
What are two common causes of hematogenous urinary tract infections?
Staphylococcus aureus bacteremia and Mycobacterium tuberculosis.
Reasoning: there are two major mechanisms for urinary tract infections. Ascending urinary tract infections are the most common and there are hematogenous urinary tract infections.
You have a patient who has recently immigrated from Nepal, who comes into clinic with very dry, scaly, hypopigmented patches with very sharply defined edges:

Upon palpation, the plaques are anesthetic. A biopsy is performed on the plaques revealing well-formed granulomas, and a few acid-fast bacteria. What is the most likely cause of this person's lesions?
Mycobacterium leprae
Reasoning: This patient is likely suffering from tuberculoid leprosy. It is classically characterized by anesthetic macules or plaques, enlarged peripheral nerves near the skin lesions, and histology with well-formed granulomas with few acid-fast bacteria.
A 33-yo female in South America presents to her physician with complaints of fever, malaise, and a large swollen lesion on her right cheek. A peripheral blood smear is collected, and it is determined that she has Chagas disease for which she is treated.
What complications is she at risk of if her disease progresses to a chronic stage (hint: there are 4)?
Hepatosplenomegaly, Myocarditis, Megaesophagus, and Megacolon
The causative organism is Trypanosoma cruzi. T. cruzi is transmitted via the triatomine (kissing) bug. Bites from the bug leave large swollen areas (particularly on the face or extremities) called Chagomas. The complications listed are essentially due to inflammatory damage to their respective tissues (heart, GI tract, Liver, and spleen
A 74-year-old man of Swedish descent reports receiving countless blood transfusions to treat his hemophilia. This history includes hundreds of transfusions received before 1992, when blood donations began to be screened for all variants of HIV. Despite his very high risk of HIV exposure, he never became infected with the virus. Which homozygous mutation is most likely contributing to this patient’s inability to become infected with HIV?
CCR5 gene deletion
The CCR5 receptor is a protein expressed on the surface of leukocytes and is used by HIV to enter and infect the cells. Up to 13% of individuals of Northern European descent have a deletion of the CCR5 receptor gene, which codes for a mutant CCR5 receptor that fails to reach the cell surface. Homozygotes for this deletion do not become infected with HIV despite multiple exposures, and heterozygotes, if infected, have a very slow course of disease. The patient in this vignette is likely to be a homozygote for this mutation.
A 70 yo male presents to clinic with the following skin findings. When asked about his recent activities, he tells you that he has been working in his garden with his wife. Based on these findings, what histopath would you expect to see for the most likely causative organism?

Cigar shaped yeast
Explanation: This is sporotrichosis cause by Sporothrix schenckii. It is a nodular, ulcerative skin finding that follows the lymphatics, and is typically associated with gardeners (source is soil and decaying plant material; needs direct inoculation like rose thorns)
A 19-year-old male arrives at the emergency room with trismus, difficulty breathing and muscles spasms. His mother found him unable to move two hours prior when coming over to visit. Physical exam shows a deep puncture wound on the bottom of his foot. What neurotransmitters are blocked by the toxin produced by this patient’s infection?
GABA and glycine
Reasoning: Trismus (“lock jaw”) is a classic system of generalized Clostridium tetani infection which causes spastic paralysis. The toxin that the organism produces is Tetanospasmin which blocks the release of inhibitory neurotransmitters GABA and glycine.
A 6-month-old child arrives to the emergency department with constipation, poor feeding, hypotonia and a weak cry. The child had been healthy up to this point with no complications during birth. The mother recalls the child had been eating normally and had recently filmed a video of her child trying honey for the first time. What is the gold standard for diagnosis of the organism responsible for the infant’s symptoms?
Mouse bioassay
Reasoning: The infant is suffering from infection of food botulism caused by Clostridium botulinum. In infants, it is classically caused by ingestion of spores (particularly through consumption of raw honey). In adults it is more associated with wound botulism. In the laboratory, conventional health diagnosis requires demonstration of the toxin for which mouse bioassay is the gold standard.
A 65 y.o. woman arrives at the hospital with worsening shortness of breath, fever, chills. Upon admission she was diagnosed with COVID-19 and after a week, required ventilator assistance to breathe. After being placed on a ventilator, purulent tracheal discharge was sent for a gram stain revealing gram-positive cocci in clusters. What other clinical manifestations would you expect to see in this patient?
Secondary bacteremia with subsequent seeding to the kidney, bones, or heart.
Reasoning: The most common causes of ventilator associated pneumonia are Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, Acinetobacter, and Staphylococcus aureus. The Gram stain reveals gram-positive cocci in clusters, which is characteristic of S. aureus. S. aureus can colonize the respiratory tract leading to pneumonia, especially when patients are already ill. Bacteremia is a common complication.
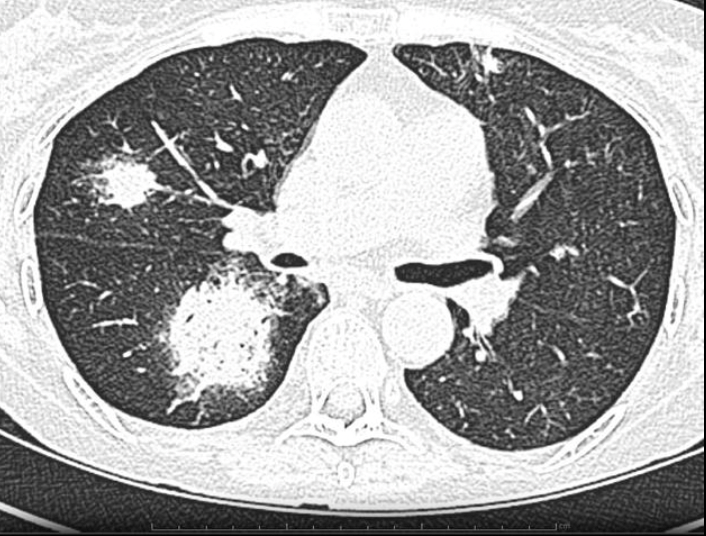
An 80-year-old woman presents to clinic with A four-year history of productive cough, and intermittent dyspnea with exertion. She has been treated with azithromycin for presumed community acquired pneumonia, and her symptoms had initially improved. Subsequently she experienced discrete recurrent episodes of “bronchitis” with productive cough. She reported a 10-year pack smoking history in the past. Her past medical history includes asthma, atrial fibrillation, GERD, osteopenia, and hyperthyroidism. Her sputum culture returned positive for an acid fast bacteria, but her TB test returned normal. CT imaging was performed and it showed:
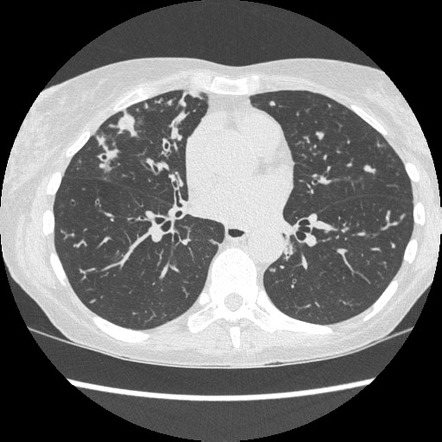
What is the most likely cause of her symptoms?
MAC
This woman likely suffers from MAC pulmonary disease. This patient fits the pattern of lady Windermere syndrome, which is typically seen in elderly white woman who chronically suppressed the normal cough reflex.
A 27-yo male from Ohio presents to the clinic with fever, weakness, and exercise intolerance. He tells you this is abnormal for him, as he usually goes on 5 mile hikes each weekend on wooded trail near his home. Physical exam demonstrates a male who appears with slight jaundice. A thin blood smear is ordered an demonstrates the following:
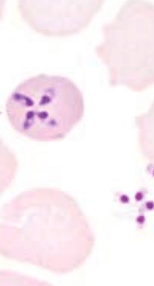
How do you suspect the causative organism was transmitted in this case (be specific)?
Ixodes scapularis (tick bite)
The causative organism of the patient's symptoms is Babesia microti. Patients usually present with non-specific ssx and fever. This organism can also cause anemia, which lends to the ssx profile as well (weakness, exercise intolerance). The blood smear shows a key finding (maltese cross). This organism can be transmitted via tick bites (ixodes scapularis is the vector; white tailed deer and white footed mouse are the reservoirs) or blood transfusions.
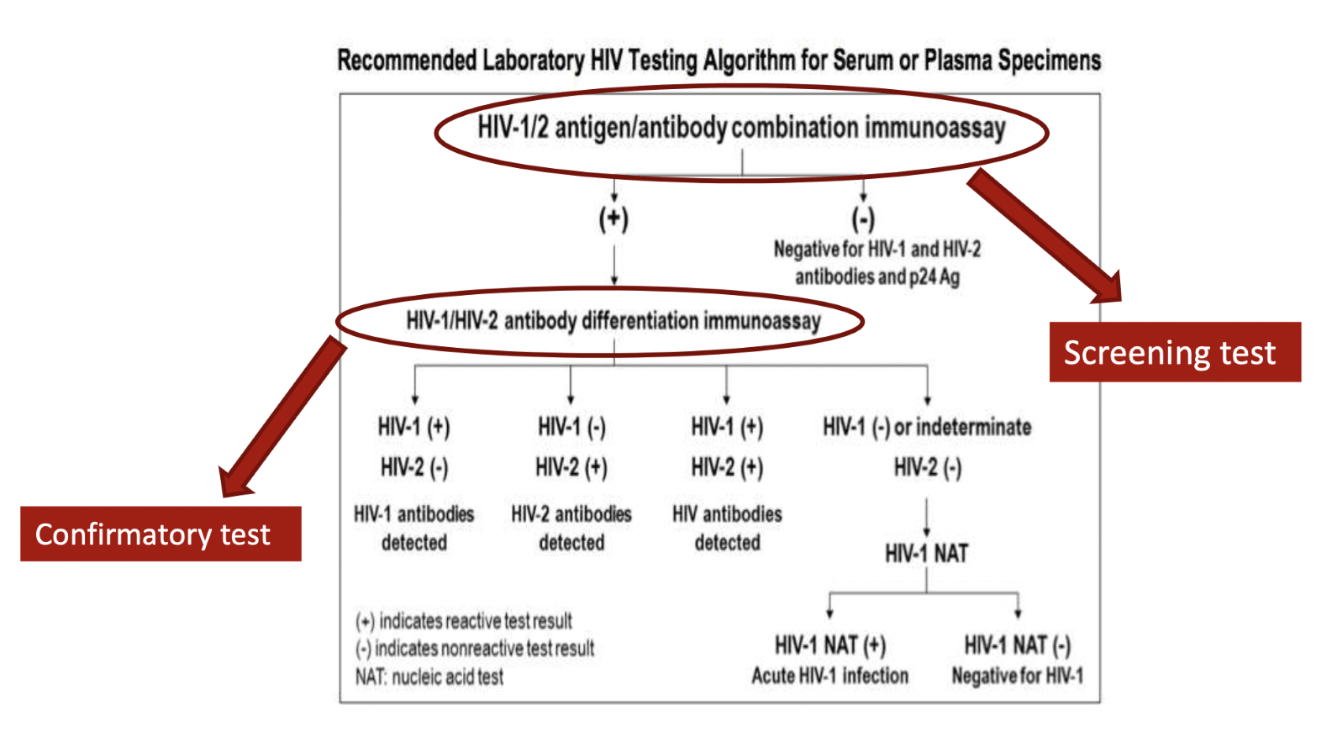
An 18-year-old man tested positive for HIV on an HIV 1/2 antigen/antibody combination immunoassay (screening test). His physician explains that an HIV diagnosis cannot be made based on the screening test alone, and that a confirmatory test must be ordered to make a definitive diagnosis. What is the confirmatory test for HIV testing?
HIV-1/HIV-2 antibody differentiation immunoassay
The HIV screening test includes antibodies for HIV-1 and HIV-2, as well as the p24 antigen. Detection of any of these components yields a positive result. To make a definitive diagnosis of HIV, an antibody differentiation immunoassay must be performed. This is a confirmatory test and yields information about whether the patient is infected with HIV-1, HIV-2, both viruses, or neither.
A 23 yo male presents to the ER with fatigue, fever, cough, and shortness of breath. He has a history of lupus for which he takes prednisone. A chest CT is performed shows the following. What marker could you test for in the blood for diagnosis of this infectious organism?
Galactomannan
Explanation: This is pneumonia caused by aspergillus. The patient presentation, history of steroid use (for lupus), and characteristic imaging on chest CT (halo sign) can all lend to this on the differential. Galactomannan is a polysaccharide antigen in the cell walls of aspergillus that can be released into the bloodstream during infection. It is very specific for aspergillus.
Other key findings: septate, acute-angle branching histopath; risk factor of chronic granulomatous disease (NADPH oxidase deficiency/dysfunction); voriconazole is first-line treatment