What is pulmonary edema?
Pulmonary edema is a medical condition characterized by the accumulation of fluid in the lungs. This fluid buildup can impair the exchange of oxygen and carbon dioxide in the lungs, making it difficult for the affected person to breathe.
What are the first steps in BLS?
Check the Scene: Ensure the scene is safe for both you and the victim. Look for potential hazards, such as traffic, fire, or electrical dangers. If the scene is not safe, wait for professional help to arrive.
Check for Responsiveness: Approach the victim and gently tap them while shouting, "Are you okay?" If the person is unresponsive, they may need immediate assistance.
Call for Help: If the victim is unresponsive or not breathing normally, call for emergency medical help (e.g., 911 in the United States) immediately. If someone else is present, instruct them to call for help while you begin providing care.
Check for Breathing: Kneel beside the victim and open their airway by tilting their head backward and lifting their chin up. Look, listen, and feel for normal breathing for about 5-10 seconds. If the victim is not breathing or only gasping, begin chest compressions.
Start Chest Compressions: Place the heel of one hand on the center of the victim's chest (usually just below the nipple line) and place the other hand on top of the first. Lock your elbows and use your upper body weight to push hard and fast at a rate of at least 100-120 compressions per minute. Allow the chest to fully recoil after each compression. Compressions should be about 2 inches (5 centimeters) deep. Continue compressions until professional help arrives or the victim shows signs of life.
What discharge instructions would you provide for someone with heart failure?
Assessing fluid balance is crucial for individuals diagnosed with heart failure to manage their condition effectively and prevent fluid overload, which can exacerbate their symptoms. The nurse should educate the client on monitoring their fluid balance at home. Here are some important points the nurse should teach the client:
Daily Weighing: Instruct the client to weigh themselves at the same time each day, preferably in the morning after waking up and after voiding, while wearing the same clothing. Sudden weight gain, typically 2-3 pounds or more within a day or a few days, may indicate fluid retention and should be reported to their healthcare provider.
Fluid Intake Monitoring: Encourage the client to keep track of their daily fluid intake, including water, beverages, and foods with high water content. Set a daily fluid intake limit as per their healthcare provider's recommendation.
Sodium Restriction: Explain the importance of limiting sodium (salt) intake, as excess sodium can lead to fluid retention. Teach the client to read food labels and choose low-sodium options. Recommend avoiding high-sodium foods like processed and fast foods.
Recognizing Symptoms: Educate the client about the signs and symptoms of fluid overload, such as shortness of breath, fatigue, rapid weight gain, swelling of the legs, ankles, or abdomen, increased fatigue, orthopnea (multiple pillows), and reduced urine output. Emphasize the importance of promptly reporting these symptoms to their healthcare provider.
Medication Adherence: Ensure that the client understands the importance of taking prescribed medications, such as diuretics (water pills) and ACE inhibitors, as directed by their healthcare provider. Medications play a key role in managing fluid balance.
Dietary Restrictions: Discuss dietary restrictions, including limiting fluid intake, if necessary. The client may be advised to limit their daily fluid intake to a specific amount, and it's essential to follow these recommendations closely.
Position Changes: Teach the client to elevate their legs when sitting or lying down to reduce swelling, promote circulation, and help manage fluid balance.
Regular Follow-Up: Stress the importance of attending regular follow-up appointments with their healthcare provider. These visits are essential for monitoring the client's condition, adjusting medications, and assessing their fluid status.
Recognizing Triggers: Discuss potential triggers that can worsen heart failure symptoms, such as infections, excessive physical activity, or non-compliance with medications. Encourage the client to avoid these triggers.
Lifestyle Modifications: Encourage a heart-healthy lifestyle, including regular exercise (as recommended by the healthcare provider), a heart-healthy diet, smoking cessation, and limiting alcohol intake.
It's important to individualize the education based on the specific needs and conditions of the client, as well as any recommendations provided by their healthcare provider. Additionally, the client should have access to a healthcare professional or heart failure specialist for ongoing support and guidance in managing their condition at home.
What is the action of angiotensin-converting enzyme (ACE) inhibitors?
Name two Ace inhibitors.
Angiotensin-converting enzyme (ACE) inhibitors are a class of medications used primarily to treat conditions such as hypertension (high blood pressure) and heart failure. The action of ACE inhibitors is to block or inhibit the activity of an enzyme called angiotensin-converting enzyme. This enzyme plays a crucial role in the renin-angiotensin-aldosterone system (RAAS), a hormonal system that regulates blood pressure and fluid balance in the body. Therefore ace inhibitors: Promote vasodilation, diuresis Decrease BP, and afterload (improve LV ejection, reduce myocardial workload) Relieve s/s of HF, prevent progression of HF
Name of Ace inhibitors:
Enalapril (Vasotec): Enalapril is used to treat hypertension and various heart conditions.
Lisinopril (Prinivil, Zestril): Lisinopril is commonly prescribed for hypertension and heart failure.
Captopril (Capoten): Captopril is an older ACE inhibitor used for treating hypertension and heart problems.
Ramipril (Altace): Ramipril is used to manage hypertension and reduce the risk of heart-related events in high-risk individuals.
Benazepril (Lotensin): Benazepril is used for hypertension and certain heart conditions.
Quinapril (Accupril): Quinapril is prescribed for high blood pressure and other cardiac conditions.
Perindopril (Coversyl): Perindopril is used to treat hypertension and other cardiovascular conditions.
What is systolic heart failure/ What medications are key?
Systolic heart failure, also known as heart failure with reduced ejection fraction (HFrEF), is a condition in which the heart's ability to contract and pump blood is impaired. This results in a reduced ejection fraction, which is the percentage of blood that the left ventricle of the heart pumps out with each contraction. Normally, the ejection fraction is around 55-70%, but in systolic heart failure, it is typically reduced to 40% or lower.
The main goal of treating systolic heart failure is to improve the heart's ability to pump blood effectively and alleviate symptoms. Key medications that are commonly prescribed for systolic heart failure include:
ACE Inhibitors (Angiotensin-Converting Enzyme Inhibitors): Medications like enalapril, lisinopril, and ramipril are used to dilate blood vessels and reduce the workload on the heart. They can also improve symptoms and increase survival rates.
ARBs (Angiotensin II Receptor Blockers): Drugs like losartan and valsartan have effects similar to ACE inhibitors and may be used when ACE inhibitors are not tolerated.
Beta-Blockers: Medications like carvedilol, metoprolol, and bisoprolol are used to reduce the heart rate, decrease the heart's workload, and improve its efficiency. They can also improve symptoms and reduce the risk of hospitalization.
Diuretics: Diuretics like furosemide (Lasix) help to remove excess fluid from the body, reducing swelling and congestion, which are common symptoms of heart failure.
Aldosterone Antagonists: Spironolactone and eplerenone are used to block the effects of the hormone aldosterone, which can contribute to heart failure progression and fluid retention.
Sacubitril/Valsartan: This is a combination medication that includes sacubitril and valsartan. It is often used in place of ACE inhibitors or ARBs and has been shown to reduce the risk of heart failure hospitalizations and improve survival.
Digoxin: This medication may be used to help control heart rate and improve symptoms in some cases of systolic heart failure.
Hydralazine and Isosorbide Dinitrate: This combination is used in some situations, especially when other medications are not well tolerated.
In addition to these medications, lifestyle modifications such as a low-sodium diet, fluid restriction, regular exercise, and smoking cessation are essential in managing systolic heart failure. Some patients may also be candidates for device therapy, such as implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT), to help improve heart function and reduce symptoms.
It's important to note that the specific treatment plan for an individual with systolic heart failure may vary based on their unique circumstances, and the management should be overseen by a healthcare provider with expertise in heart failure. Regular monitoring and adjustments to the treatment plan may be necessary to optimize care.
What is heart failure?
Heart failure is a condition in which the heart is unable to pump blood effectively to meet the body's needs. There are several potential causes of heart failure, which can be categorized into two main types: systolic heart failure and diastolic heart failure. Systolic heart failure is characterized by a weakened heart muscle's reduced ability to contract and pump blood, while diastolic heart failure involves the heart becoming stiff and unable to fill properly.
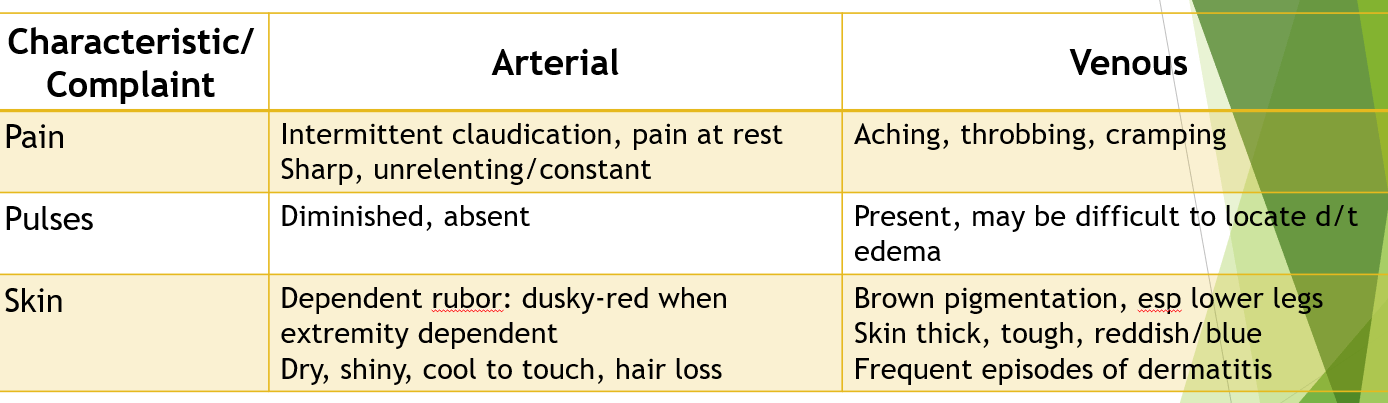
What are the vascular assessment common complaints for arterial and venous?
Patients with prolonged, uncontrolled hypertension is at risk for developing which health problems?
Prolonged, uncontrolled hypertension (high blood pressure) can significantly increase the risk of developing various serious health problems, including:
Heart Disease: Hypertension can lead to the thickening of the heart muscle (left ventricular hypertrophy) and increase the risk of coronary artery disease, heart attacks, and heart failure.
Stroke: High blood pressure can damage the blood vessels in the brain, increasing the risk of stroke.
Kidney Disease: Chronic uncontrolled hypertension can damage the blood vessels in the kidneys, leading to chronic kidney disease and even kidney failure.
Eye Problems: Hypertension can damage the blood vessels in the eyes, potentially leading to vision problems and even blindness.
Aneurysms: Persistent high blood pressure can weaken the walls of blood vessels, increasing the risk of developing aneurysms (bulges in the blood vessel walls) that can rupture and cause life-threatening bleeding.
Peripheral Artery Disease: Hypertension can narrow and harden the arteries in the legs and other extremities, leading to reduced blood flow, pain, and an increased risk of amputation.
Cognitive Decline: There is evidence to suggest that chronic hypertension is associated with an increased risk of cognitive decline and dementia, such as Alzheimer's disease.
Metabolic Syndrome: Hypertension is often a component of metabolic syndrome, which includes a cluster of conditions like high blood sugar, abdominal obesity, and abnormal cholesterol levels. Metabolic syndrome increases the risk of heart disease and type 2 diabetes.
It's important to manage and control hypertension through lifestyle changes, medication as prescribed by a healthcare professional, and regular check-ups. Lifestyle modifications such as maintaining a healthy diet, exercising regularly, reducing sodium intake, and managing stress can help prevent and manage hypertension, reducing the risk of these associated health problems. If you have hypertension, it's crucial to work with your healthcare provider to develop a personalized treatment plan and monitor your blood pressure regularly.
What are the nursing interventions for ACE inhibitors?
ACE inhibitors, or Angiotensin-Converting Enzyme inhibitors, are commonly used in healthcare to manage conditions like hypertension, heart failure, and diabetic kidney disease. Nursing interventions for patients taking ACE inhibitors should focus on monitoring, education, and promoting medication adherence while also assessing for potential side effects. Here are some nursing interventions for patients on ACE inhibitors:
Assessment and Monitoring:
- Regularly assess the patient's blood pressure, heart rate, and respiratory rate to monitor the drug's effectiveness.
- Monitor for signs of hypotension, especially during the initial dosing period.
- Assess for signs and symptoms of heart failure (e.g., dyspnea, edema, fatigue) and kidney dysfunction (elevated serum creatinine and blood urea nitrogen).
Electrolyte Imbalance Monitoring:
- Watch for signs of hyperkalemia (elevated potassium levels) due to the potential of ACE inhibitors to increase potassium levels. This includes muscle weakness, irregular heart rhythms, and palpitations.
Renal Function Monitoring:
- Monitor renal function by assessing urine output, serum creatinine, and blood urea nitrogen levels.
- Inform the healthcare provider promptly if there are any signs of kidney dysfunction.
Patient Education:
- Educate the patient about the importance of taking the medication as prescribed, including the dosage and frequency.
- Explain potential side effects and the importance of reporting them, such as dizziness, dry cough, or swelling of the face, lips, or throat.
- Encourage the patient to maintain a consistent schedule for taking their medication.
Dietary Guidance:
- Advise the patient to be mindful of their potassium intake, as ACE inhibitors can lead to elevated potassium levels. They should avoid high-potassium foods and supplements.
Fluid Intake:
- Ensure that the patient understands the importance of maintaining proper fluid intake, as ACE inhibitors can cause excessive urination. Encourage them to drink an appropriate amount of water to prevent dehydration.
Medication Reconciliation:
- Review the patient's complete medication list, including over-the-counter and herbal supplements, to prevent potential drug interactions or duplications.
Regular Follow-Up:
- Schedule regular follow-up appointments to monitor the patient's progress and adjust the medication regimen as needed.
Patient Safety:
- Caution the patient about the possibility of dizziness and orthostatic hypotension when rising from a sitting or lying position. Advise them to change positions slowly.
Lifestyle Modifications:
- Encourage the patient to adopt a heart-healthy lifestyle, including a low-sodium diet, regular exercise, and smoking cessation if applicable.
Documentation:
- Accurate and thorough documentation of the patient's vital signs, medication administration, and any reported symptoms or adverse effects is crucial for effective patient care and continuity.
Nursing care for patients taking ACE inhibitors is essential to ensure optimal therapeutic outcomes, minimize side effects, and prevent complications. Nurses play a vital role in patient education, medication management, and monitoring for potential issues related to ACE inhibitor therapy.
What are the nursing interventions when giving diuretics?
Nursing interventions when giving diuretics (medications that promote diuresis, or increased urine output) are essential to ensure patient safety and monitor for the desired therapeutic effects. Diuretics are commonly used to treat conditions like hypertension, heart failure, and edema. Here are some key nursing interventions when administering diuretics:
Assessment:
- Perform a thorough patient assessment, including baseline vital signs (blood pressure, heart rate, respiratory rate), weight, and fluid status. Note any preexisting conditions or allergies that may affect the choice of diuretic.
- Assess for signs and symptoms of fluid overload (e.g., edema, pulmonary congestion) and electrolyte imbalances (e.g., potassium, sodium, and calcium levels).
Medication Administration:
- Administer the diuretic as prescribed by the healthcare provider, following the "Five Rights" of medication administration: the right patient, right medication, right dose, right route, and right time.
- Administer some diuretics with food or milk to reduce gastrointestinal irritation, as directed by the healthcare provider.
- Ensure that the patient understands the importance of taking the medication as prescribed and reporting any side effects or concerns.
Patient Education:
- Educate the patient about the medication's purpose, potential side effects, and the need for compliance with the prescribed regimen.
- Advise the patient to maintain a consistent daily intake of potassium-rich foods or supplements, as diuretics can lead to potassium loss (e.g., bananas, oranges, spinach).
- Emphasize the importance of maintaining adequate fluid intake to prevent dehydration.
Monitoring:
- Monitor vital signs, particularly blood pressure and heart rate, to assess the drug's effectiveness and potential adverse effects.
- Evaluate urine output and characteristics, looking for changes in color, odor, and volume.
- Monitor electrolyte levels, especially potassium, sodium, and calcium, as diuretics can lead to electrolyte imbalances. Report any significant deviations to the healthcare provider.
- Assess for symptoms of hypokalemia (low potassium), such as muscle weakness, irregular heartbeat, or fatigue.
- Assess for orthostatic hypotension by monitoring blood pressure and signs/symptoms when the patient changes position.
Weight Monitoring:
- Weigh the patient regularly, ideally at the same time each day and with the same clothing, to monitor for changes in fluid balance. Report significant weight changes to the healthcare provider.
Lifestyle Modifications:
- Encourage the patient to follow a low-sodium diet to complement the diuretic's effects and reduce the risk of fluid retention.
- Instruct the patient to limit alcohol and caffeine intake, as they can increase fluid loss.
Safety Measures:
- Caution the patient to be aware of dizziness or lightheadedness, especially when rising from a seated or lying position.
- Recommend using support aids (e.g., handrails) if the patient has mobility issues due to the diuretic's potential to cause orthostatic hypotension.
Documenting:
- Thoroughly document all assessments, medication administration, and the patient's response to treatment. This documentation is vital for tracking the patient's progress and ensuring continuity of care.
Nursing interventions are crucial in the management of patients receiving diuretic therapy to optimize the therapeutic effects while minimizing potential side effects and complications. Regular communication with the healthcare provider and an interdisciplinary approach to care can enhance patient outcomes.
What are the common causes of heart failure?
Coronary Artery Disease (CAD): Blockage or narrowing of the coronary arteries, which supply blood to the heart muscle, can lead to myocardial infarction (heart attack) and damage the heart muscle. Atherosclerosis
Hypertension (High Blood Pressure): Prolonged high blood pressure puts extra strain on the heart, causing it to work harder over time, which can lead to heart failure.
Cardiomyopathy: Various types of cardiomyopathy, such as dilated, hypertrophic, and restrictive cardiomyopathy, can weaken the heart muscle and lead to heart failure.
Valvular Heart Disease: Malfunctioning heart valves, such as aortic stenosis or mitral regurgitation, can disrupt normal blood flow and contribute to heart failure.
Heart Arrhythmias: Irregular heart rhythms, particularly sustained tachycardias or atrial fibrillation, can affect the heart's pumping ability and lead to heart failure.
Congenital Heart Defects: Some individuals are born with structural heart abnormalities that can eventually lead to heart failure.
Infections: Viral infections, such as myocarditis, can damage the heart muscle and impair its function.
Drug or Alcohol Abuse: Prolonged use of certain drugs or excessive alcohol consumption can have toxic effects on the heart.
Diabetes: Poorly controlled diabetes can damage blood vessels and nerves, increasing the risk of heart failure.
Lung Diseases: Conditions like chronic obstructive pulmonary disease (COPD) can put additional strain on the heart and lead to right-sided heart failure.
Obesity: Excess body weight can increase the workload on the heart and contribute to heart failure.
Anemia: A lack of red blood cells can reduce the oxygen-carrying capacity of the blood, leading to an increased workload on the heart.
Hyperthyroidism: An overactive thyroid gland can affect the heart's function and potentially lead to heart failure.
Certain Medications: Some medications, especially those that affect heart function or blood pressure, may contribute to heart failure.
Previous Heart Attacks: Scarring from a prior heart attack can weaken the heart muscle and increase the risk of heart failure.
It's important to note that heart failure can result from a combination of factors, and it often develops gradually. Understanding and addressing the underlying causes are essential for managing and treating heart failure. Treatment may involve lifestyle changes, medications, devices (e.g., pacemakers or implantable cardioverter-defibrillators), or, in severe cases, heart transplant. If you suspect you or someone you know has heart failure, it's crucial to seek medical evaluation and care.
What is Peripheral artery disease (PAD)?
Peripheral artery disease (PAD), also known as peripheral vascular disease (PVD), is a common circulatory condition in which narrowed arteries reduce blood flow to the extremities, typically the legs. This reduced blood flow can lead to various symptoms and, in severe cases, can result in tissue damage, gangrene, and even amputation. PAD is usually caused by atherosclerosis, a buildup of fatty deposits (plaque) in the arteries, but it can also be related to other factors like inflammation or injury.
Here are some key points about PAD:
Risk Factors: Several factors can increase the risk of developing PAD, including smoking, diabetes, high blood pressure, high cholesterol, obesity, a family history of PAD, and advancing age.
Symptoms: Many people with PAD may not experience any symptoms (asymptomatic). However, when symptoms do occur, they often include:
- Claudication: Pain, cramping, or fatigue in the legs, especially during physical activity, which improves with rest.
- Numbness or weakness in the legs.
- Coldness in the lower leg or foot.
- Changes in the color of the legs or feet.
- Slow-healing sores or wounds on the feet or legs.
Diagnosis: PAD can be diagnosed through physical exams, ankle-brachial index (ABI) testing, which compares blood pressure in the arms and legs, and imaging studies like ultrasound, CT angiography, or magnetic resonance angiography.
Treatment: Treatment for PAD aims to alleviate symptoms, improve circulation, and reduce the risk of complications. Options include:
- Lifestyle changes: Smoking cessation, exercise, and dietary modifications.
- Medications: Blood thinners, cholesterol-lowering drugs, and medications to control blood pressure and blood sugar.
- Endovascular procedures: Angioplasty and stenting to open narrowed arteries.
- Bypass surgery: Redirecting blood flow around the blocked artery using a graft.
Prevention: Preventive measures can help reduce the risk of developing PAD. These include maintaining a healthy lifestyle, managing risk factors, and seeking regular medical check-ups.
Complications: Untreated PAD can lead to complications such as chronic leg pain, critical limb ischemia (severe restriction of blood flow), and an increased risk of heart attack and stroke.
It's essential for individuals at risk or experiencing symptoms of PAD to seek medical attention promptly to receive appropriate diagnosis and treatment. Effective management can help improve symptoms, mobility, and overall quality of life for those with this condition.
What is the action of Beta Blockers?
Beta blockers, also known as beta-adrenergic blocking agents, are a class of medications that primarily act by blocking the effects of the hormone epinephrine (adrenaline) and its related compounds on beta-adrenergic receptors in the body. These medications are used to treat various medical conditions, particularly those related to the cardiovascular and nervous systems. The main actions of beta blockers include:
Lowering Heart Rate: Beta blockers reduce the heart rate by blocking the action of epinephrine on beta-1 adrenergic receptors in the heart. This effect helps decrease the workload of the heart, making it useful in conditions such as hypertension (high blood pressure), angina (chest pain), and arrhythmias (irregular heart rhythms).
Reducing Blood Pressure: By lowering heart rate and the force of heart contractions, beta blockers decrease blood pressure. This is especially beneficial in managing hypertension.
Decreasing Myocardial Oxygen Demand: Beta blockers reduce the heart's oxygen demand by slowing the heart rate and reducing the force of contraction. This can be helpful in angina and after heart attacks to reduce the risk of further damage. Decreasing the afterload.
Antiarrhythmic Effects: Beta blockers can help control abnormal heart rhythms by regulating the electrical conduction system of the heart.
What oral diuretics are given for heart failure?
Oral diuretics are commonly prescribed in the management of heart failure to help reduce fluid retention and alleviate symptoms like edema (swelling) and shortness of breath. The most frequently used oral diuretics in heart failure include:
Furosemide (Lasix): Furosemide is a loop diuretic and is often the first-line choice for treating acute and chronic heart failure. It works by inhibiting the reabsorption of sodium and chloride in the loop of Henle in the kidneys.
Bumetanide (Bumex): Bumetanide is another loop diuretic that is similar in action to furosemide and may be used when furosemide is ineffective or causes adverse effects.
Torsemide (Demadex): Torsemide is also a loop diuretic and is sometimes preferred in heart failure patients due to its longer duration of action, which allows for once-daily dosing in many cases.
Hydrochlorothiazide (HCTZ): Hydrochlorothiazide is a thiazide diuretic. While it is not as potent as loop diuretics, it is sometimes used in combination with them to provide an additive diuretic effect.
Spironolactone (Aldactone): Spironolactone is a potassium-sparing diuretic that is often used in conjunction with other diuretics to help counteract potassium loss. It also has additional benefits in heart failure, as it can reduce the risk of adverse remodeling of the heart.
Eplerenone (Inspra): Eplerenone is another potassium-sparing diuretic and is similar to spironolactone in its effects. It can be used in conjunction with standard therapy for heart failure.
The choice of diuretic and dosing will depend on the individual patient's condition, response to treatment, and other factors. It's important for healthcare professionals to carefully monitor the patient's electrolyte levels, renal function, and clinical symptoms while using diuretics to avoid complications associated with excessive diuresis or electrolyte imbalances.
Please note that the use of diuretics in heart failure should be under the guidance of a healthcare provider, as they will tailor the treatment to the specific needs and circumstances of the patient.
What are the nursing interventions for peripheral arterial insufficiency?
Peripheral arterial insufficiency, also known as peripheral arterial disease (PAD), is a condition in which there is reduced blood flow to the extremities, typically the legs, due to the narrowing or blockage of the arteries. Nursing interventions for peripheral arterial insufficiency aim to alleviate symptoms, improve blood flow, prevent complications, and promote overall well-being. Here are some common nursing interventions for peripheral arterial insufficiency:
Assessment:
- Perform a thorough assessment of the patient's vascular status, including blood pressure, peripheral pulses, skin color, temperature, capillary refill, and signs of ischemia (e.g., pallor, coolness).
- Assess pain levels, location, and characteristics.
Education:
- Educate the patient about the disease, its risk factors, and the importance of lifestyle modifications, such as smoking cessation, diet, and exercise.
- Emphasize the need to maintain optimal blood pressure and cholesterol levels.
Medication Management:
- Administer prescribed medications, such as antiplatelet agents (e.g., aspirin), anticoagulants, and medications to manage underlying conditions like hypertension and diabetes.
Wound Care:
- Teach the patient about proper wound care and the importance of keeping the feet and legs clean and dry.
- Monitor and care for any wounds, ulcers, or gangrenous areas to prevent infection and further complications.
Exercise and Activity:
- Encourage regular exercise and physical activity within the patient's capabilities. Supervise exercise programs to promote circulation and reduce claudication symptoms.
- Advise the patient on a gradual walking program and the importance of avoiding prolonged periods of immobility.
Positioning:
- Encourage the elevation of the legs to help improve blood flow and reduce edema.
Foot Care:
- Teach the patient about foot care and the importance of daily inspection of the feet for signs of injury, infection, or ulcers.
- Recommend wearing well-fitting shoes and socks and avoiding tight, restrictive footwear.
Smoking Cessation:
- Provide support and resources to help patients quit smoking, as smoking is a significant risk factor for peripheral arterial insufficiency.
Pain Management:
- Administer prescribed pain medications and provide non-pharmacological pain management techniques like relaxation exercises and distraction techniques.
Monitoring:
- Continuously assess the patient's response to interventions and any changes in their condition.
- Monitor for signs of complications, such as infection, gangrene, or critical limb ischemia.
- Collaboration:
- Collaborate with other healthcare professionals, such as vascular specialists, to plan and coordinate care for the patient.
- Support and Lifestyle Modifications:
- Provide emotional support and encourage the patient to make necessary lifestyle modifications to manage their condition effectively.
Nursing care for peripheral arterial insufficiency should be individualized to the patient's specific needs and may evolve over time as the condition progresses. Frequent monitoring and patient education are essential components of care to prevent complications and improve the patient's quality of life.
What are the signs and symptoms of right sided heart failure?
Viscera and peripheral congestion
Jugular venous distention (JVD)
Dependent edema
Hepatomegaly
Ascites
Weight gain
What is the assessment for chronic leg ulcers?
A careful nursing history and assessment are important. The extent and type of pain are carefully assessed, as are the appearance and temperature of the skin of both legs. The quality of all peripheral pulses is assessed, and the pulses in both legs are compared. Any limitation of mobility and activity that results from vascular insufficiency is identified. It is not likely that there is any direct indication for assessment of apical heart rate, although peripheral pulses must be assessed.
What is the action of Dobutamine, and what are the side effects?
Dobutamine is a Catecholamine, simulate beta-adrenergic receptors, increased contractility medication primarily used for its positive inotropic effects. Therefore, it increases the force of contraction of the heart muscle. It is typically used to improve cardiac output in conditions such as heart failure or during certain medical procedures.
Here are some key actions and effects of dobutamine:
Positive Inotropy: Dobutamine primarily stimulates beta-1 adrenergic receptors in the heart, leading to an increase in the strength of cardiac contractions. This can help improve the heart's pumping ability, making it useful in cases of heart failure.
Increased Heart Rate: Dobutamine can also increase heart rate, which can further enhance cardiac output.
Vasodilation: It has some vasodilatory effects, which means it can dilate (widen) blood vessels, particularly in the peripheral vascular system. This can help reduce afterload, which is the resistance the heart has to pump against.
Improved Blood Flow: By increasing cardiac output and reducing afterload, dobutamine can improve blood flow to vital organs and tissues.
Side effects of dobutamine can include:
Increased Heart Rate: While the increase in heart rate can be beneficial in some cases, it can also lead to tachycardia (abnormally fast heart rate), which may not be well-tolerated by some patients.
Arrhythmias: Dobutamine can sometimes lead to cardiac arrhythmias (abnormal heart rhythms), particularly in patients with pre-existing heart conditions.
Hypertension: In some individuals, dobutamine may cause an increase in blood pressure.
Ischemia: Dobutamine can increase the heart's demand for oxygen, which can be problematic in patients with underlying coronary artery disease, potentially leading to myocardial ischemia (reduced blood flow to the heart muscle).
Headache, Nausea, and Other Minor Side Effects: Like many medications, dobutamine can cause common side effects such as headache, nausea, and sweating.
Elevated Blood Sugar: Dobutamine can raise blood sugar levels, which may be a concern in individuals with diabetes.
It's important to note that dobutamine is typically administered in a clinical setting, often in a hospital or under close medical supervision, due to its potential side effects and the need for careful monitoring of the patient's condition. The dose and duration of dobutamine therapy should be determined by a healthcare professional based on the patient's specific medical condition and response to the medication.
What is warfarin? What lab value monitors warfarin?
Warfarin is an anticoagulant medication commonly prescribed to prevent or treat blood clots, particularly in conditions such as deep vein thrombosis (DVT), pulmonary embolism, atrial fibrillation, and after certain surgeries like joint replacement. Warfarin works by interfering with the body's ability to form blood clots, primarily by inhibiting the production of clotting factors in the liver.
The effectiveness and safety of warfarin therapy are monitored through a specific laboratory test known as the International Normalized Ratio (INR). The INR is a standardized way of measuring the clotting time of a patient's blood and is used to assess how quickly the blood clots in response to warfarin therapy. The target INR value varies depending on the medical condition for which warfarin is prescribed. Common target ranges include:
- Atrial Fibrillation: Target INR range of 2.0 to 3.0.
- Venous Thromboembolism (DVT, PE): Target INR range of 2.0 to 3.0.
- Mechanical Heart Valve: Target INR range varies depending on the specific type and location of the valve, but it often falls within the range of 2.5 to 3.5.
- Patients not taking warfarin PT 11-13.5, INR 0.8-1.1
Patients on warfarin therapy typically have their INR levels monitored regularly by healthcare providers, especially when starting treatment or adjusting the medication dose. Frequent monitoring helps ensure that the INR remains within the therapeutic range to prevent both bleeding and clotting complications. The dosage of warfarin may be adjusted based on the INR results to maintain the desired level of anticoagulation.
It's important for patients taking warfarin to follow their healthcare provider's instructions carefully, including taking the medication as prescribed and attending regular INR monitoring appointments, as individual responses to warfarin can vary, and close monitoring is necessary to maintain its safety and effectiveness. Dietary choices can also affect warfarin's action, so patients are often advised to maintain consistent vitamin K intake and avoid drastic changes in their diet.
What is venous insufficiency?
Venous insufficiency, also known as chronic venous insufficiency (CVI), is a medical condition that occurs when the veins in the legs, and sometimes other parts of the body, have difficulty returning blood to the heart. This condition typically affects the lower extremities. It can result from problems with the valves in the veins, which are responsible for preventing blood from flowing backward. When these valves become weak or damaged, they may fail to function properly, leading to a range of symptoms and complications.
Common signs and symptoms of venous insufficiency include:
- Swelling of the legs and ankles
- Pain or aching in the legs, which may worsen when standing or sitting for extended periods
- Heaviness or fatigue in the legs
- Itching or tingling in the affected areas
- Skin changes, such as discoloration, thickening, and the development of varicose veins
- Open sores or ulcers, especially in more advanced cases
Venous insufficiency can result from various factors, including genetics, prolonged sitting or standing, obesity, a history of deep vein thrombosis (DVT), and aging. It can lead to more serious complications, such as venous ulcers and skin infections if left untreated.
Treatment for venous insufficiency typically involves lifestyle changes and medical interventions, such as:
Compression stockings: These are specially designed stockings that help improve blood flow by providing external pressure on the legs.
Elevation of the legs: Elevating the legs periodically throughout the day can reduce swelling and improve circulation.
Exercise: Regular physical activity, especially walking, can help pump blood back to the heart and strengthen the leg muscles.
Medications: In some cases, medications may be prescribed to reduce inflammation, relieve pain, or prevent blood clots.
Endovenous laser treatment (EVLT) or radiofrequency closure: These minimally invasive procedures can be used to seal off problematic veins, redirecting blood flow to healthier veins.
Surgery: In severe cases, surgical procedures such as vein stripping or valve repair may be necessary.
It's important to consult a healthcare professional if you suspect you have venous insufficiency or if you experience any of the symptoms mentioned above. Early diagnosis and management can help prevent complications and improve your quality of life.
What are the signs and symptoms of left-sided heart failure?
Pulmonary congestion, crackles
S3 or “ventricular gallop”
Dyspnea on exertion (DOE)
Low O2 sat
Dry, nonproductive cough initially
Oliguria
Mr. Jones is scheduled for furosemide 40 mg PO bid
(1000 and 2200). Would you question this dose?
WHY OR WHY NOT
Yes, taking at 2200 would impede a patient's sleeping cycle. Lasix may be prescribed to be taken in the morning to help reduce edema (fluid retention) during the day, while in other cases, it may be prescribed to be taken in the afternoon or evening to minimize nighttime urination. The timing of Lasix administration can also be influenced by factors such as the patient's daily routine and when it's most convenient for them to take the medication.
Mr. Jones has been ordered 60 mg of Lasix IVP. The medication arrives from the pharmacy. How many ml would you administer?
6 ml
10 mg/1 ml is the concentration
What is an Aldosterone agonist?
Name the medications that are aldosterone agonists.
Aldosterone agonists are a class of drugs that mimic the effects of aldosterone, a hormone produced by the adrenal glands. Aldosterone plays a crucial role in regulating sodium and potassium balance in the body, which in turn affects blood pressure and fluid balance.
Aldosterone agonists are typically used to treat conditions such as:
Hypertension (high blood pressure): By mimicking the effects of aldosterone, these drugs promote the reabsorption of sodium and the excretion of potassium in the kidneys. This leads to increased water retention and an overall increase in blood pressure. Aldosterone antagonists are sometimes used to counteract this effect.
Heart failure: Aldosterone agonists can help reduce the strain on the heart by promoting salt and water excretion, which can be beneficial in patients with heart failure.
These medications are often used to treat conditions like high blood pressure (hypertension) and certain heart and kidney disorders. Some common aldosterone agonists include:
Fludrocortisone: This is a synthetic aldosterone analog and is often used to treat conditions such as Addison's disease and primary adrenal insufficiency.
Spironolactone: While spironolactone is often considered an aldosterone antagonist (it blocks the effects of aldosterone), it also has some weak agonistic activity. It is primarily used as a potassium-sparing diuretic and can help in conditions where reducing potassium loss is necessary, like in heart failure.
Eplerenone: Eplerenone is another medication used primarily for the treatment of high blood pressure (hypertension). It is more selective for the aldosterone receptor than spironolactone and is often preferred in cases where avoiding some of the side effects associated with spironolactone is desirable.
What is the action of diuretics?
Diuretics, also known as water pills, are medications that increase the production of urine by the kidneys, leading to the removal of excess sodium and water from the body. Their primary action is to promote diuresis, which is the increased excretion of urine. Diuretics are commonly used to treat various medical conditions, including hypertension (high blood pressure), edema (fluid retention), and certain heart and kidney disorders. Here are the primary actions and effects of diuretics:
Increased Urination: Diuretics increase the volume and frequency of urination, which helps eliminate excess salt and water from the body. This can reduce the overall fluid volume in the bloodstream.
Reduction in Blood Pressure: By removing excess sodium and water from the body, diuretics can decrease the volume of blood circulating through the blood vessels. This, in turn, lowers blood pressure, making diuretics an important class of medications for managing hypertension.
Edema Reduction: Diuretics are often used to reduce edema, which is the accumulation of excess fluid in the body's tissues. This is commonly seen in conditions like heart failure, kidney disease, and certain liver disorders.
Electrolyte Imbalance: While diuretics are effective in removing excess sodium and water, they can also lead to electrolyte imbalances, particularly a loss of potassium. Some diuretics are known as "potassium-sparing" to counteract this effect. Others may require potassium supplements or dietary changes to maintain proper electrolyte balance.
Treatment of Certain Medical Conditions: Diuretics are used in the management of various medical conditions, including hypertension, congestive heart failure, kidney diseases, and certain types of edema. The choice of diuretic and its dosage depends on the specific condition and the patient's needs.
There are different types of diuretics, including thiazide diuretics, loop diuretics, and potassium-sparing diuretics. Each type works on different parts of the kidney's filtration system and has its specific uses and potential side effects. It's essential to use diuretics under the guidance of a healthcare professional, as they can have significant effects on fluid balance, blood pressure, and electrolyte levels.