A 45-year-old patient presents with complaints of neck pain radiating to the right arm, associated with numbness and tingling in the right hand. On examination, you note decreased cervical spine range of motion, particularly with extension and right lateral flexion. Sensory examination reveals diminished sensation along the C6 dermatome, and muscle strength testing shows weakness in the right biceps (C5-C6). Reflex testing reveals a diminished biceps reflex on the right.
What is the most likely diagnosis for this patient?
A) Cervical spondylosis
B) Thoracic outlet syndrome
C) Cervical radiculopathy
D) Shoulder impingement syndrome
C) cervical radiculopathy
A 55-year-old female presents with complaints of persistent low back pain for the past 4 weeks. The pain is described as dull and achy in the lumbar region, with occasional sharp episodes. She reports that the pain is worse at night and has been interfering with her sleep. The patient has a history of breast cancer treated 5 years ago with surgery and radiation. She has also experienced some recent fatigue, and her appetite has decreased slightly. On physical examination, the patient has tenderness over the lumbar spine and limited range of motion, but there are no neurological deficits or signs of acute injury.
Which of the following is the most concerning red flag in this patient’s presentation?
A) Persistent low back pain for 4 weeks
B) Pain that is worse at night
C) History of breast cancer
D) Decreased appetite and fatigue
Explanation: Pain that is worse at night is a significant red flag in this patient’s presentation. Night pain that interferes with sleep is often associated with more serious conditions, such as malignancy (e.g., metastatic cancer to the spine) or infection (e.g., osteomyelitis or spinal abscess). In this case, the patient's history of breast cancer, a known risk factor for metastatic disease, increases the concern that the low back pain may be related to cancer recurrence or metastasis.
- A) Persistent low back pain for 4 weeks is a common presentation in musculoskeletal disorders like lumbar strain or disc herniation. However, the duration of pain alone is not enough to raise concern for a serious underlying condition unless other red flags are present.
- C) History of breast cancer raises suspicion for metastatic disease, but it is the night pain that is the more concerning red flag. A history of cancer warrants further investigation, but the presence of night pain increases the urgency of ruling out metastatic involvement.
- D) Decreased appetite and fatigue can be seen in various conditions, including cancer, but these symptoms alone are less specific and are not as strongly associated with the immediate concern of a spinal metastasis or infection as night pain is.
A 28-year-old male presents to physical therapy with complaints of anterior knee pain after participating in a recreational basketball game. He reports feeling a "pop" during a jump, followed by immediate swelling and difficulty bearing weight on the affected leg. On physical examination, the patient has swelling around the knee, and there is notable tenderness along the patellar tendon. The patient demonstrates decreased knee extension and reports instability with activities that involve pivoting. The Lachman’s test is positive, and the Anterior Drawer test also reproduces the symptoms.
Which of the following is the most likely diagnosis based on the patient’s history and examination findings?
A) Anterior cruciate ligament (ACL) tear
B) Patellar tendinopathy
C) Medial collateral ligament (MCL) sprain
D) Meniscal tear
Answer:
A) Anterior cruciate ligament (ACL) tear
Explanation: The patient's history of hearing a "pop" during jumping, followed by immediate swelling, inability to bear weight, and instability during pivoting, combined with positive findings on the Lachman’s test and Anterior Drawer test, strongly suggests an anterior cruciate ligament (ACL) tear. The ACL is often injured during activities that involve cutting, pivoting, or jumping, and the patient may experience instability or a feeling of the knee "giving way." The Lachman’s test and Anterior Drawer test are both specific tests for ACL integrity, and a positive result typically confirms an ACL tear.
- B) Patellar tendinopathy: This condition typically causes pain along the inferior pole of the patella, especially with jumping or repetitive load-bearing activities. However, it would not cause instability or a positive Lachman’s or Anterior Drawer test.
- C) Medial collateral ligament (MCL) sprain: MCL injuries typically occur from a direct blow to the outside of the knee or a twisting force. While MCL sprains can cause pain and swelling, they do not typically result in positive Lachman’s or Anterior Drawer tests, which are more specific to ACL injuries.
- D) Meniscal tear: While meniscal tears can present with knee pain and instability, they are usually not associated with the sudden "pop" and immediate swelling that occur with ACL injuries. The tests that are most useful for diagnosing meniscal tears (e.g., McMurray's or Apley’s compression tests) were not mentioned here, and the primary instability and positive Lachman’s test point to an ACL injury.
A 52-year-old female presents to physical therapy with a 4-month history of progressive shoulder pain and stiffness. She reports difficulty reaching behind her back, brushing her hair, and performing activities that require overhead arm movement. The pain is dull and constant, and she notes that the shoulder stiffness has gradually increased over the past several weeks. Upon examination, she has limited range of motion in all directions, especially external rotation, with a capsular pattern of restriction. There is tenderness in the anterior shoulder but no evidence of acute inflammation or obvious injury.
What is the most likely diagnosis based on this patient's presentation?
A) Rotator cuff tear
B) Adhesive capsulitis
C) Shoulder impingement syndrome
D) Glenohumeral instability
Answer:
B) Adhesive capsulitis
Explanation: The patient’s gradual onset of pain, progressive stiffness, and restricted motion in all directions with a capsular pattern (i.e., external rotation > abduction > internal rotation) are characteristic features of adhesive capsulitis (Frozen Shoulder). This condition typically progresses through three stages: the freezing stage (pain and stiffness), the frozen stage (stiffness without pain), and the thawing stage (gradual improvement in range of motion).
- A) Rotator cuff tear: While a rotator cuff tear can cause weakness and pain, it does not typically present with the same capsular pattern of motion loss, especially widespread motion loss like adhesive capsulitis.
- C) Shoulder impingement syndrome: Shoulder impingement typically presents with pain during overhead activities and a painful arc but does not usually cause global motion loss or the capsular pattern seen in adhesive capsulitis.
- D) Glenohumeral instability: Instability usually presents with apprehension and pain during certain shoulder movements but does not cause a global limitation of motion like adhesive capsulitis.
Name 3 positive tests that may suggest SIJ dysfunction.
Thigh thrust, distraction, and compression are the 3 main tests we learned where any 2 positive tests rule in SIJ dysfunction. Other tests for SIJ may include sacral thrust and Gaenslen's. A positive FABER reproducing pain along SIJ region may indicate SIJ dysfunction.
A 32-year-old male presents with mid-back pain that has been progressively worsening for the past 6 weeks. He describes the pain as a dull ache located between his shoulder blades, which intensifies with prolonged sitting and activities involving reaching overhead. He has no history of trauma or injury, and his neurological exam is normal. Upon physical examination, the patient demonstrates limited thoracic spine rotation and extension with increased tenderness in the paraspinal muscles around T6-T8.
Which of the following is the most likely diagnosis based on the patient's history and clinical findings?
A) Thoracic disc herniation
B) Thoracic spine fracture
C) Thoracic facet joint dysfunction
D) Costovertebral joint dysfunction
Answer:
C) Thoracic facet joint dysfunction
Explanation: The patient’s presentation of mid-back pain that is exacerbated by sitting and overhead activities, along with limited thoracic spine rotation and extension, suggests thoracic facet joint dysfunction. The pain is typically localized around the facet joints, and the restriction in movement (particularly in extension and rotation) is indicative of this condition.
- A) Thoracic disc herniation: Although thoracic disc herniations can cause mid-back pain, they are much less common than lumbar disc herniations. They typically present with more neurological signs, such as radiating pain, numbness, or weakness, which this patient does not have. Disc herniations often involve the lower thoracic or lumbar region.
- B) Thoracic spine fracture: A fracture in the thoracic spine would likely result from trauma (e.g., a fall or motor vehicle accident) and would typically present with more acute, severe pain. There is no history of trauma in this case, so a fracture is less likely.
- D) Costovertebral joint dysfunction: Costovertebral joint dysfunction can present with rib and thoracic spine pain, especially during deep breathing or trunk rotation. However, the absence of rib-related symptoms and the localized paraspinal tenderness make costovertebral dysfunction less likely.
A 22-year-old male athlete presents with hip pain following a fall during a soccer game. He reports immediate sharp pain in the groin area and is unable to bear weight on the affected leg. On physical examination, the patient demonstrates limited hip flexion and internal rotation, with pain reported during these movements. There is no significant swelling or bruising around the hip joint. X-rays reveal a femoral neck fracture.
Which of the following is the most appropriate initial management for this condition?
A) Non-weight-bearing with crutches and referral for physical therapy
B) Hip spica cast for 6 weeks
C) Immediate surgical consultation for possible reduction and fixation
D) Application of a femoral brace and observation for 2 weeks
C) Immediate surgical consultation for possible reduction and fixation
Explanation: A femoral neck fracture, particularly in a young, active patient, is a serious injury and often requires surgical intervention to prevent complications such as non-union, avascular necrosis, or long-term functional disability. Immediate surgical consultation is necessary to evaluate the need for reduction and internal fixation to ensure proper healing and minimize complications.
- A) Non-weight-bearing with crutches and referral for physical therapy is not an appropriate treatment for a femoral neck fracture, as this type of fracture typically requires surgical intervention.
- B) Hip spica cast for 6 weeks is generally not appropriate for femoral neck fractures, as these fractures often require surgical fixation to maintain proper alignment and avoid complications.
- D) Application of a femoral brace and observation for 2 weeks is also not recommended for femoral neck fractures, as these fractures have a high risk of complications without surgical management.
A 30-year-old male recreational runner presents with ankle pain after tripping while running on uneven terrain. He describes the pain as sharp and located along the medial aspect of his ankle. The patient reports swelling around the medial malleolus and difficulty with weight-bearing, especially when attempting to walk or run. Physical examination reveals the valgus stress test produces pain.
Which of the following is the most likely diagnosis based on the patient’s history and examination findings?
A) Medial ankle sprain (deltoid ligament injury)
B) Lateral ankle sprain (ATFL injury)
C) Tibiofibular syndesmosis injury
D) Achilles tendonitis
A) Medial ankle sprain (deltoid ligament injury)
Explanation: The patient’s history of tripping with subsequent medial ankle pain, tenderness over the deltoid ligament, and positive findings on the valgus stress test strongly suggest a medial ankle sprain, specifically involving the deltoid ligament. The deltoid ligament is located on the medial side of the ankle, and its injury typically occurs in eversion injuries, such as the one described.
- B) Lateral ankle sprain (ATFL injury): Lateral ankle sprains usually result from inversion injuries (the foot rolling inward) and would primarily involve the anterior talofibular ligament (ATFL). This injury would not present with pain or tenderness over the medial aspect of the ankle.
- C) Tibiofibular syndesmosis injury: Also known as a high ankle sprain, this injury typically involves external rotation of the foot and pain above the level of the lateral malleolus. The symptoms in this case are more localized to the medial ankle, which makes a syndesmosis injury less likely.
- D) Achilles tendonitis: Achilles tendonitis typically presents with pain and tenderness in the posterior heel or Achilles tendon, especially with running or jumping activities. It would not cause medial ankle pain or tenderness over the deltoid ligament.
A 45-year-old male presents with lateral elbow pain that has gradually worsened over the past 6 months. He is a carpenter and reports that his pain is aggravated by gripping tools, lifting objects, and performing repetitive wrist extension activities. On physical examination, there is tenderness over the lateral epicondyle and pain with resisted wrist extension. The Cozen's test is positive. His range of motion is within normal limits, but he experiences discomfort with activities that involve gripping or wrist extension.
What is the most likely diagnosis?
A) Medial epicondylitis (golfer's elbow)
B) Lateral epicondylitis (tennis elbow)
C) Radial tunnel syndrome
D) Elbow osteoarthritis
B) Lateral epicondylitis (tennis elbow)
Explanation: The patient's presentation, including lateral elbow pain, pain with resisted wrist extension, and a positive Cozen's test, is highly suggestive of lateral epicondylitis (commonly known as tennis elbow). This condition involves degeneration of the extensor tendons, particularly the extensor carpi radialis brevis (ECRB), due to repetitive strain from activities that require wrist extension and gripping. The Cozen's test (resisted wrist extension with the elbow in a flexed position) is commonly used to diagnose this condition.
- A) Medial epicondylitis (golfer's elbow): This condition involves pain on the medial side of the elbow and is aggravated by activities that involve wrist flexion or pronation, not wrist extension.
- C) Radial tunnel syndrome: This condition involves compression of the radial nerve in the forearm, leading to pain in the lateral forearm and weakness in the wrist and finger extensors. However, it does not typically present with tenderness over the lateral epicondyle or a positive Cozen's test.
- D) Elbow osteoarthritis: While osteoarthritis can cause elbow pain, it is usually associated with joint stiffness, decreased range of motion, and crepitus. The patient’s symptoms and positive physical exam findings are more consistent with lateral epicondylitis than with osteoarthritis.
A patient presents to your clinic with c/o neck pain. Upon further questioning she mentioned feeling tingling pain down her arm. Which tests would you perform to rule in a classification of neck pain with radiating pain?
Positive test cluster includes:
- Upper limb neurodynamic/tension test
- Spurling's test
- Cervical distraction
- less than 60 degrees of rotation to the involved side
A 38-year-old female presents to physical therapy with complaints of daily headaches that begin in the neck and radiate to the forehead, temples, and behind the eyes. The patient reports that her headaches are often triggered by prolonged sitting at her desk, poor posture, and stress. She has no history of migraines, and the headaches are typically one-sided. On physical examination, the patient demonstrates limited cervical range of motion, especially with rotation and extension, and tenderness in the upper cervical spine, particularly around C1-C3. The clinical diagnosis is cervicogenic headache.
Which of the following interventions is most appropriate for the management of this patient's cervicogenic headache?
A) Cervical traction and modalities such as heat for pain relief
B) Strengthening of the deep neck flexors and postural retraining
C) Upper cervical spine manipulation for immediate pain relief
D) Ergonomic modifications and corticosteroid injections
Answer:
B) Strengthening of the deep neck flexors and postural retraining
Explanation: Cervicogenic headaches are caused by cervical spine dysfunction, typically due to poor posture, muscle imbalances, or restricted mobility in the upper cervical spine (C1-C3). The most effective management involves addressing the underlying musculoskeletal issues that contribute to the headache. This includes:
Strengthening the deep neck flexors (which are often weak in patients with cervicogenic headache) to improve cervical stability.
Postural retraining to reduce strain on the cervical spine and prevent the development of musculoskeletal imbalances that trigger headaches.
A) Cervical traction and modalities: While these may provide temporary pain relief, they do not address the root cause of cervicogenic headaches (i.e., muscle weakness and poor posture). Traction and heat are adjuncts to treatment, not the primary management.
C) Upper cervical spine manipulation: While cervical spine manipulation may be effective for some patients with cervicogenic headache, it should be used cautiously and only in patients who are appropriate candidates (e.g., absence of contraindications like osteoporosis or severe instability). It is not typically the first-line treatment.
D) Ergonomic modifications and corticosteroid injections: Ergonomic modifications may be beneficial for reducing triggers, but corticosteroid injections are typically not recommended for cervicogenic headaches unless there is significant inflammation or a specific structural issue that warrants them.
A 42-year-old male presents with low back pain that started after he lifted a heavy object at work. He describes the pain as a dull ache in the lumbar region, with occasional sharp sensations when bending forward or lifting. He denies leg pain, numbness, or tingling. He is able to perform most daily activities, but reports difficulty with prolonged sitting and standing. On physical examination, the patient demonstrates limited lumbar range of motion with pain at end range flexion, but no neurological deficits. He has a positive prone instability test, and his fear-avoidance behavior scale score is moderate.
According to the Treatment-Based Classification (TBC) system, which of the following is the most appropriate classification for this patient?
A) Manipulation classification
B) Specific exercise classification
C) Stabilization classification
D) Traction classification
C) Stabilization classification
Explanation: This patient’s presentation is most consistent with the stabilization classification under the Treatment-Based Classification (TBC) system. The following features support this classification:
- Positive prone instability test, which is indicative of spinal instability.
- Moderate fear-avoidance behavior, suggesting that the patient may benefit from stabilization exercises to improve motor control and reduce fear-related avoidance of movement.
- Difficulty with activities that involve prolonged sitting and standing, which could be linked to instability and the need for strengthening and stabilization exercises.
In the stabilization classification, treatment focuses on strengthening the core musculature, improving motor control, and addressing the fear-avoidance behavior that may contribute to the patient's symptoms.
- A) Manipulation classification would be appropriate if the patient had acute, low back pain with no neurological signs and a mechanical presentation amenable to manual therapy. However, this patient’s symptoms and positive prone instability test suggest that manipulation would not be the primary intervention.
- B) Specific exercise classification is typically used for patients with symptoms that can be alleviated through specific movement patterns, such as flexion or extension-based exercises, often seen in cases of disc herniation. This patient’s symptoms do not align with that classification.
- D) Traction classification is typically used for patients with symptoms of nerve root compression (radiculopathy) or severe symptoms that may benefit from mechanical traction. This patient does not report radiating leg pain or neurological symptoms.
A 22-year-old male presents to the emergency department with a sprained ankle after rolling his foot while playing soccer. He is able to bear weight, but the ankle is swollen, and he reports moderate pain when walking. On physical examination, there is tenderness over the posterior aspect of the lateral malleolus and medial malleolus, but no tenderness over the navicular bone or base of the 5th metatarsal. The patient’s range of motion is limited due to pain.
According to the Ottawa Ankle Rules, which of the following is true regarding whether the patient should undergo ankle radiographs?
A) The patient should receive ankle radiographs because of tenderness over the lateral and medial malleolus
B) The patient should not receive ankle radiographs because he is able to bear weight and does not have tenderness over the navicular or base of the 5th metatarsal
C) The patient should receive ankle radiographs because he has tenderness over both the lateral and medial malleolus
D) The patient should receive ankle radiographs because he cannot bear weight on the affected ankle
Answer:
B) The patient should not receive ankle radiographs because he is able to bear weight and does not have tenderness over the navicular or base of the 5th metatarsal
Explanation: The Ottawa Ankle Rules are a clinical decision tool used to determine when radiographs (X-rays) are necessary for an ankle injury. According to these rules, X-rays are required if there is:
- Tenderness over the posterior malleolus (medial or lateral) and the patient is unable to bear weight (i.e., cannot walk more than four steps) or
- Tenderness over the navicular bone or the base of the 5th metatarsal, or
- Inability to bear weight after the injury.
In this case:
The patient has tenderness over the lateral and medial malleolus, but he is able to bear weight and does not have tenderness over the navicular or base of the 5th metatarsal. According to the Ottawa Ankle Rules, he does not meet the criteria for requiring radiographs.
A) The patient should receive ankle radiographs because of tenderness over the lateral and medial malleolus: This is incorrect. Tenderness alone over the malleolus does not automatically require radiographs; the patient must also be unable to bear weight, which he can do.
C) The patient should receive ankle radiographs because he has tenderness over both the lateral and medial malleolus: This is incorrect. The presence of tenderness over both malleoli does not indicate the need for radiographs unless the patient cannot bear weight.
D) The patient should receive ankle radiographs because he cannot bear weight on the affected ankle: This is incorrect. Although the patient reports pain, he is able to bear weight, so radiographs are not required based on this rule.
Patient is struggling to lift arm into flexion. What scapular movements are necessary to assist the arm in flexion?
Answer: upward rotation, elevation, and protraction
Bonus! Can you explain all of the necessary scapular movements that accompany shoulder movement?
What tests would you perform to rule in subacromial impingement?
Test cluster needing 3 positive tests to rule in- infraspinatus muscle test, Hawkins Kennedy, painful arc (mid range)
Positive Neer's would rule out
-ac joint- painful arc at end range (not in cluster), crossover test, resisted extension (horizontal abduction), O'Brien's
-Rotator cuff cluster- infraspinatus muscle test, drop arm sign, painful arc
A 40-year-old male presents to the emergency department after a minor motor vehicle accident (MVA). He was the driver and reports that his head was jerked forward and backward during the crash. He denies any tingling, numbness, or weakness in the arms or legs and has no history of previous neck injuries. On examination, he has mild neck pain, but he is able to turn his head 45 degrees to both the left and right without difficulty. He has no other significant injuries, and the accident was relatively low impact.
Based on the Canadian C-Spine Rule, which of the following is the most appropriate course of action regarding cervical spine imaging for this patient?
A) Immediate cervical spine imaging is required due to the mechanism of injury.
B) Cervical spine imaging is not required because the patient can rotate his neck 45 degrees.
C) Immediate cervical spine imaging is required due to the patient’s age of 40.
D) Cervical spine imaging is required because the patient reports mild neck pain.
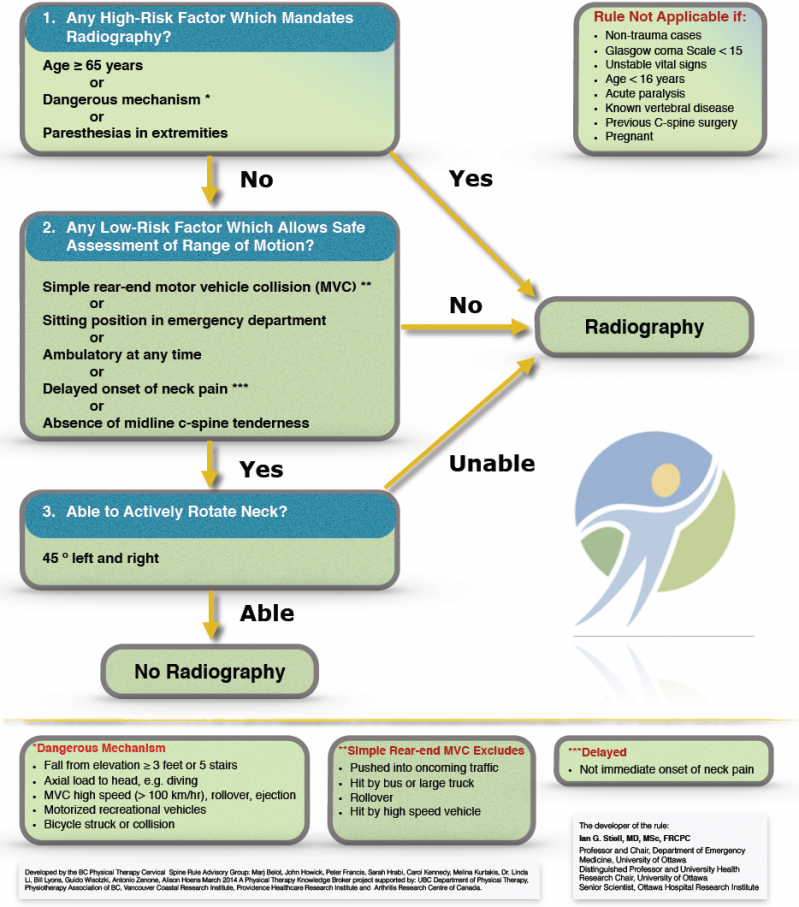
Answer:
B) Cervical spine imaging is not required because the patient can rotate his neck 45 degrees.
Explanation: The Canadian C-Spine Rule is designed to help clinicians decide when cervical spine radiographs (X-rays) are necessary for patients who have experienced trauma. According to the rule:
- If the patient is alert and stable and has no high-risk factors (e.g., age > 65, dangerous mechanism of injury, neurological deficits, midline neck tenderness), and they can rotate their neck 45 degrees to both sides without significant pain, cervical spine imaging is typically not required.
In this case:
The patient does not have any high-risk factors, such as neurological deficits or significant mechanism of injury.
The patient is able to rotate his neck 45 degrees in both directions, which is a low-risk factor and excludes the need for imaging according to the Canadian C-Spine Rule.
A) Immediate cervical spine imaging is not required because the mechanism of injury was minor and does not indicate a high-risk factor for a cervical spine injury.
C) Immediate cervical spine imaging is not required due to the patient’s age of 40, as age alone is not a high-risk factor for cervical spine injury.
D) Cervical spine imaging is not required solely due to mild neck pain if there are no high-risk factors and the patient can rotate their neck 45 degrees.
Patient is lacking adduction and internal rotation at the hip. In what direction would you mobilize to improve this deficit?
decreased ROM from capsular causes in these directions is cause by posterior capsule tightness (often the ischiofemoral ligament)
A 25-year-old female presents with complaints of anterior knee pain that worsens with activities such as running, squatting, and climbing stairs. She reports no history of trauma or injury. On physical examination, the patient's Q angle is measured to be 18 degrees. The Q angle is the angle formed by two lines: one from the anterior superior iliac spine (ASIS) to the center of the patella, and the other from the center of the patella to the tibial tuberosity.
Which of the following is most likely associated with the patient's knee pain given the increased Q angle?
A) Patellofemoral pain syndrome (PFPS)
B) Medial collateral ligament sprain
C) Iliotibial band syndrome
D) Meniscus tear
A) Patellofemoral pain syndrome (PFPS)
Explanation: An increased Q angle (typically > 15° in females and > 20° in males) is associated with altered patellar tracking and patellofemoral pain syndrome (PFPS). The Q angle reflects the alignment of the quadriceps muscle pull and the angle of the patella. When this angle is increased, it can cause excessive lateral tracking of the patella, leading to irritation of the patellofemoral joint. This results in anterior knee pain, which is often aggravated by activities that load the patellofemoral joint, such as running, squatting, or climbing stairs—common symptoms of PFPS.
- B) Medial collateral ligament sprain: While a MCL sprain can cause knee pain, it typically results from trauma or a valgus force applied to the knee. The increased Q angle is not directly related to MCL injury.
- C) Iliotibial band syndrome: This condition causes lateral knee pain and is typically aggravated by activities such as running or cycling. However, it is not directly related to an increased Q angle.
- D) Meniscus tear: A meniscus tear typically results from twisting or pivoting movements and is more likely to be associated with mechanical symptoms such as locking or catching in the knee. It is not typically linked to an increased Q angle.
A 35-year-old male baseball player presents to physical therapy with pain in his shoulder that worsens with overhead throwing activities. He reports a deep, aching pain in the shoulder joint that radiates toward the back of the shoulder. On examination, he demonstrates limited internal rotation and painful arc during shoulder abduction. You suspect that the patient may have internal subacromial impingement.
Which of the following is the key feature that differentiates internal from external subacromial impingement?
A) Pain location – internal impingement presents with anterior shoulder pain, while external impingement presents with lateral or anterior pain
B) Pain during range of motion – internal impingement occurs during shoulder flexion, while external impingement occurs during shoulder abduction
C) Painful arc – internal impingement is associated with pain during the mid-range of shoulder abduction, while external impingement is associated with pain at the end of shoulder abduction
D) Range of motion – external impingement is more likely to have limited internal rotation, while internal impingement is associated with decreased external rotation
C) Painful arc – internal impingement is associated with pain during the mid-range of shoulder abduction, while external impingement is associated with pain at the end of shoulder abduction
Explanation: The primary difference between internal and external subacromial impingement lies in the painful arc and the mechanism of impingement:
Internal impingement: This typically involves the posterior aspect of the rotator cuff, especially the supraspinatus and infraspinatus, as they are impinged between the posterior glenoid labrum and the humeral head during abduction and external rotation (especially in athletes like baseball pitchers). This results in pain during the mid-range (90-120 degrees) of shoulder abduction, and the pain is usually located posteriorly.
External impingement: This involves the subacromial space, where structures like the rotator cuff tendons and subacromial bursa are impinged against the acromion and coracoacromial ligament. It typically causes pain at the end range of abduction (above 90 degrees), and the pain is often lateral or anterior.
A) Pain location – internal impingement presents with anterior shoulder pain, while external impingement presents with lateral or anterior pain: This statement is partially correct, but it does not specifically address the primary difference in the painful arc and range of motion.
B) Pain during range of motion – internal impingement occurs during shoulder flexion, while external impingement occurs during shoulder abduction: Both internal and external impingement can occur during abduction. This option is inaccurate because the painful arc and location of pain differ for internal vs external impingement, not the range of motion itself.
D) Range of motion – external impingement is more likely to have limited internal rotation, while internal impingement is associated with decreased external rotation: This is incorrect. Both types of impingement can cause some range of motion limitations, but the painful arc is the key differentiator rather than specific ranges of motion.
Patient presents to clinic with imaging positive for hip OA. What tests would you perform to ensure their pain was truly due to these imaging findings?
Diagnostic cluster: painful squat, IR <25, pain with active extension, pain with hip flexion, + Scour
A 32-year-old patient presents with complaints of numbness and tingling in the right hand and forearm. The patient reports a history of intermittent pain and weakness in the right upper limb that has progressively worsened over the past few months. On physical examination, the patient demonstrates a positive Adson's test. The pain and sensory changes are exacerbated by neck movements, particularly with rotation and extension of the neck to the left. The patient is suspected to have thoracic outlet syndrome (TOS).
Which of the following is the most likely cause of this patient's symptoms?
A) Compression of the median nerve by the transverse cervical ligament
B) Compression of the brachial plexus between the anterior and middle scalene muscles
C) Compression of the ulnar nerve in the cubital tunnel
D) Compression of the radial nerve at the spiral groove
B) Compression of the brachial plexus between the anterior and middle scalene muscles
Explanation: Thoracic outlet syndrome (TOS) typically involves compression of neurovascular structures (brachial plexus, subclavian artery, or vein) as they pass through the thoracic outlet. In this case, the most likely cause is compression of the brachial plexus between the anterior and middle scalene muscles, which is a common finding in TOS. The positive Adson's test suggests that the symptoms are exacerbated by positional changes in the neck, which are associated with TOS due to scalene muscle involvement.
If when performing traction of the lumbar spine at 40% body weight the patient's pain begins to worsen, what would be your next course of action?
a. immediately stop treatment
b. cut the force by 50%
c. maintain the level of force until pain resides or patient can no longer tolerate
d. increase the force by small amounts
Answer: b. cut force by 50%
a. do not immediately stop treatment, first attempting to cut the force by 50% is the better answer
c. maintain the level if patient experiences partial pain relief, do not maintain if the patient's pain increases
d. only increase the force if the patient experiences no change
*if patient experiences complete pain relief it indicates that there is more going on and you should assess the indicators of nerve conduction
*force should not exceed 50-60% of body weight and typically adjust force 5-15 lbs at each subsequent session
A 58-year-old female presents to physical therapy with knee pain that has gradually worsened over the past year. She describes the pain as dull and aching, with stiffness in the morning that improves after some movement. The pain is exacerbated with prolonged walking and climbing stairs. On physical examination, she has decreased range of motion, crepitus on knee flexion, and tenderness over the medial joint line. X-rays of her knee are performed, showing joint space narrowing, osteophyte formation, and subchondral sclerosis.
Based on the Kellgren-Lawrence grading system for osteoarthritis, which of the following is the most likely grade for this patient’s knee?
A) Grade 1
B) Grade 2
C) Grade 3
D) Grade 4
Answer:
C) Grade 3 (Moderate osteoarthritis)
Explanation: The Kellgren-Lawrence grading system is commonly used to classify the severity of osteoarthritis (OA) based on radiographic findings. The criteria for each grade are as follows:
- Grade 1 (Doubtful osteoarthritis): Minimal osteophyte formation, with no significant joint space narrowing.
- Grade 2 (Mild osteoarthritis): Small osteophytes, with some joint space narrowing and mild sclerosis.
- Grade 3 (Moderate osteoarthritis): Moderate osteophyte formation, moderate joint space narrowing, and subchondral sclerosis. This is the most likely grade for this patient, based on the X-ray findings of joint space narrowing, osteophyte formation, and subchondral sclerosis, along with moderate clinical symptoms (pain with walking, climbing stairs, and morning stiffness).
- Grade 4 (Severe osteoarthritis): Large osteophytes, significant joint space narrowing, subchondral cysts, and deformity. Severe joint degeneration with marked pain and loss of function.
This patient’s symptoms, along with the X-ray findings of joint space narrowing and osteophytes, indicate moderate OA (Grade 3), as there is no mention of severe deformity or extensive joint space loss that would suggest Grade 4.
A 28-year-old male presents with shoulder pain following a recent fall onto an outstretched arm during a recreational basketball game. He reports pain and a feeling of instability in the shoulder, particularly with overhead movements and throwing. On examination, he demonstrates positive apprehension and relocation tests. Additionally, he has pain with resisted external rotation and reports a clicking sensation during certain movements, especially with abduction and external rotation. His range of motion is full, but he experiences pain at the extremes of motion.
Which of the following is the most likely diagnosis?
A) Rotator cuff tear
B) Adhesive capsulitis
C) Labral tear (SLAP or Bankart lesion)
D) Shoulder impingement syndrome
Answer:
C) Labral tear (SLAP or Bankart lesion)
Explanation: The patient’s symptoms, including pain, clicking, and instability with overhead movements, and a positive apprehension test, suggest a labral tear. Specifically, SLAP lesions (Superior Labrum Anterior to Posterior) or Bankart lesions (often associated with anterior shoulder dislocations) are common in athletes who perform repetitive overhead motions or who experience trauma, like a fall on an outstretched arm.
- A) Rotator cuff tear: A rotator cuff tear would present with weakness and pain, especially in abduction and external rotation, but would not typically cause a clicking sensation or positive apprehension test.
- B) Adhesive capsulitis: This condition is characterized by progressive stiffness and limited range of motion (especially external rotation) with gradual onset. It does not typically present with the clicking sensation or apprehension seen in labral tears.
- D) Shoulder impingement syndrome: Impingement syndrome causes pain during overhead activities and a painful arc in the range of 60-120 degrees but does not typically result in clicking or instability.
A 45-year-old male presents with complaints of knee pain that has been gradually worsening over the past few months. He reports pain along the medial aspect of the knee, especially after prolonged standing and walking. On physical examination, the patient demonstrates tenderness along the medial joint line and reports pain with weight-bearing activities. The clinician performs the following tests:
- McMurray’s test
- Apley’s compression test
- Thessaly test
Which of the following conditions is most likely based on the positive findings in all three tests?
A) Medial meniscus tear
B) Patellofemoral pain syndrome
C) Ligamentous instability
D) Iliotibial band syndrome
Answer:
A) Medial meniscus tear
Explanation: The positive findings in the McMurray’s test, Apley’s compression test, and Thessaly test are most indicative of a medial meniscus tear. These tests are specifically used to assess meniscal tears, and when all three tests are positive, it significantly increases the likelihood of this diagnosis.
McMurray’s test: This test involves rotating the knee while applying a valgus or varus stress and can provoke pain or a clicking sound if a meniscus tear is present.
Apley’s compression test: This test also assesses for meniscal tears by applying compressive force while the knee is in a prone position, which may reproduce symptoms if there is damage to the meniscus.
Thessaly test: This dynamic test involves the patient standing on one leg while rotating the body and knee. Positive results (pain or a catching sensation) can indicate a meniscal tear, particularly if the symptoms are reproduced in the medial joint line.
B) Patellofemoral pain syndrome: Patellofemoral pain syndrome typically presents with anterior knee pain, particularly around the patella, and would not typically present with positive findings for meniscal tests. The symptoms are usually exacerbated by squatting, running, or climbing stairs.
C) Ligamentous instability: Ligamentous instability (e.g., ACL or MCL injury) would present with instability and abnormal movement of the knee. The tests used in this case are more specific to meniscal pathology rather than ligamentous injury.
D) Iliotibial band syndrome: Iliotibial band syndrome typically presents with pain on the lateral aspect of the knee, not medial, and is not associated with the meniscal tests. The condition is often aggravated by running, particularly downhill or with excessive hip adduction.