This "killer headache" is characterized by a sudden, severe headache often described as the worst headache of one's life.
What is a subarachnoid hemorrhage?
This term describes a prolonged seizure lasting more than 5 minutes or multiple seizures occurring without full recovery of consciousness in between.
What is status epilepticus?
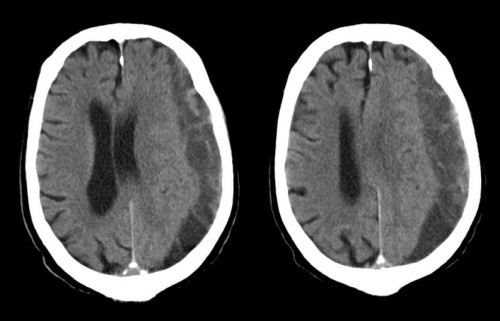
What is the diagnosis?
What is a subdural hematoma?
This maneuver, involving rapid head movements, is used to treat the most common cause of peripheral vertigo.
What is the Epley maneuver (for Benign Paroxysmal Positional Vertigo)?
How do you differentiate between Bell's Palsy and an acute CVA?
Bell's Palsy: Affects the entire side of the face (upper and lower)
CVA: Often spares the forehead (upper face) due to bilateral innervation of the upper face
This medication, often used for migraine treatment in the ED, carries a risk of serotonin syndrome when combined with SSRIs
What is sumatriptan (or other triptans)?
This post-seizure phenomenon is characterized by transient weakness in a limb or one side of the body and can mimic an acute stroke
What is Todd's paralysis?
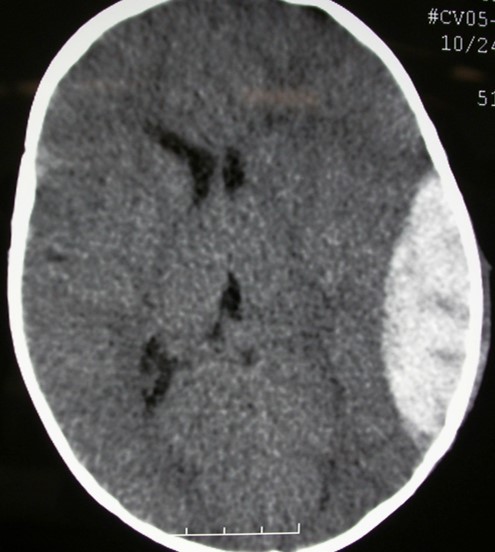
What is the diagnosis?
What is epidural hematoma?
This three-part bedside examination can help differentiate between central and peripheral causes of acute vestibular syndrome with high sensitivity and specificity.
What is the HINTS exam (Head Impulse, Nystagmus, Test of Skew)?
This treatment for acute ischemic stroke has a time window of up to 24 hours in select patients with a large vessel occlusion and salvageable brain tissue.
What is mechanical thrombectomy?
A 43 year old male patient with no significant PMHx who lives in NYSHA building in Harlem presents to the ER in the middle of January with an unremitting headache x 3 days associated with blurry vision and nausea. Vitals are within normal limits. What single test can confirm the diagnosis?
What i a VBG?
Carbom monoxide poisoning
What is the mechanism of action of levetiracetam/keppra?
Affects intraneuronal Ca2+ levels by partial inhibition of N-type Ca2+ currents, and reducing the release of Ca2+ from intraneuronal stores. Partially reverses the reductions in GABA and glycine gated currents induced by zinc and β-carbolines
 66 year old woman with PMHx of Afib on coumadin presents to the ER BIBEMS after being found unresponsive in home by relative. What medicine can be administered to mitigate the above pathology?
66 year old woman with PMHx of Afib on coumadin presents to the ER BIBEMS after being found unresponsive in home by relative. What medicine can be administered to mitigate the above pathology?
What is 4-factor prothrombin complex concentrate and IV vitamin K.
This condition, causing recurrent episodes of vertigo with fluctuating hearing loss and tinnitus, is thought to be due to endolymphatic hydrops.
What is Meniere's disease?
What is the mechanism of action of tpa?
Activation of plasminogen:
- tPA binds to fibrin in a blood clot
- It then catalyzes the conversion of plasminogen to plasmin
- Plasmin activity:
- Plasmin is a proteolytic enzyme
- It degrades fibrin, the main component of blood clots
Fibrinolysis:
- The breakdown of fibrin results in the dissolution of the blood clot
- This process is called fibrinolysis
This condition should be suspected in patients with new-onset headache, proximal muscle pain, jaw claudication, and blurry vision, especially in those over 50.
What is temporal arteritis (also known as giant cell arteritis)?
What are Dr. Chirurgi's two dogs names?
Ollie and Sam

Patient comes in with a sudden headache that started 2 hours ago. 10/10 in intensity, unremitting, worst headache of life. Vital signs include a BP of 195/96 mm Hg, HR of 92 bpm, RR of 16/minute, and T of 98.6°F (37°C). Which of the following is the best next step in patient care?
What is blood pressure control?
What type of nystagmus is concerning for a central cause of vertigo? Name at least 3
1. Gaze-evoked nystagmus
2. Vertical nystagmus: Almost always indicates a central cause.
3. Pure torsional nystagmus: Usually central in origin.
4. Bidirectional nystagmus: Changes direction without changing the position of the head, indicating a central cause.
Name at least 7 ABSOLUTE contraindications to tPA administration in an acute ischemic stroke.
1. Intracranial hemorrhage on CT
2. Neurosurgery, head trauma, or stroke in past 3 months
3. Uncontrolled hypertension (>185 mmHg SBP or >110 mmHg DBP)
4. History of intracranial hemorrhage
5. Known intracranial arteriovenous malformation, neoplasm, or aneurysm
6. Active internal bleeding
7. Suspected/confirmed endocarditis
8. Known bleeding diathesis
(a) Platelet count <100,000.
(b) Patient has received heparin within 48 hours and has an elevated aPTT (greater than upper limit of normal for laboratory).
(c) Current use of oral anticoagulants (ex: warfarin) and INR >1.7.
(d) Current use of direct thrombin inhibitors or direct factor Xa inhibitors.
9. Abnormal blood glucose (<50 mg/dL)
10. Intra-axial intracranial neoplasm
11. Gastrointestinal (GI) malignancy
12. Gastrointestinal (GI) hemorrhage within the last 21 days
13. Intracranial or intraspinal surgery within the last 3 months
14. CT brain imaging shows extensive regions of clear hypoattenuation
15. Stroke is known or suspected to be associated with aortic arch dissection
10.