A 53-year-old man with a history of HTN, CHF, DM, and CKD developed an intracerebral hemorrhage after receiving thrombolytic therapy for an ischemic stroke. This is the most appropriate treatment.
A. Protamine sulfate
B. Fresh-frozen plasma (FFP)
C. Cryoprecipitate
D. Vitamin K
E. Dialysis
What is Cryoprecitate?
Injury to this nerve causes a winged scapula.
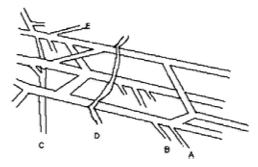
What is C. the long thoracic nerve?
.jpg)
- A dysfunction involving the stabilizing muscles of the scapula resulting in imbalance and abnormal motion of the scapula
- Types of scapular winging

- defined by the direction of the superomedial corner of the scapula
- medial scapular winging


- etiology
- dysfunction of the serratus anterior (long thoracic nerve)




- weak protraction of the scapula
- excessive medializing scapular retraction (rhomboid major and minor) and elevation (trapezius)
- dysfunction of the serratus anterior (long thoracic nerve)
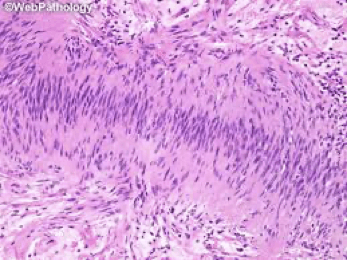
- epidemiology
- young athletic patient
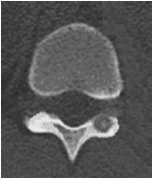
- more common than lateral
- etiology
- lateral scapular winging



- etiology
- dysfunction of the trapezius (cranial nerve XI - spinal accessory nerve)
- weak superior and medializing force on the scapula
- dysfunction of the trapezius (cranial nerve XI - spinal accessory nerve)
- epidemiology
- usually iatrogenic (history of neck surgery)
- etiology
This is the most common single suture craniosynostosis
A Sagittal craniosynostosis
B Unilateral coronal craniosynostosis
C Lambdoid synostosis
D Metopic synostosis
E Bilateral coronal craniosynostosis
What is A. Sagittal Craniosynostosis?

Brightly eosinophilic staining, irregularly shaped structures are associated with this tumor.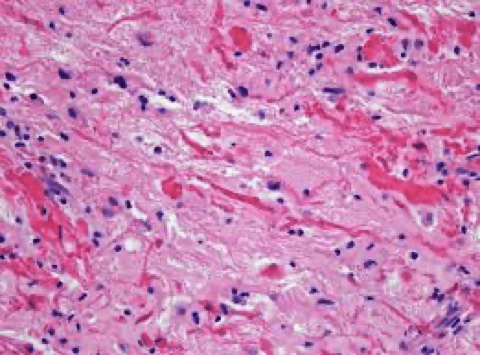
A. Medulloblastoma
B. Oligodendroglioma
C. Schwannoma
D. Pilocytic astrocytoma
E. Subependymoma
What is Pilocytic Astrocytoma?
Rosenthal fibers are beaded, elongated, or corkscrew-shaped intracytoplasmic inclusions measuring approximately 10–40 μm in diameter by 100 μm in length and are identified occasionally in astrocytes associated with intense fibrillary gliosis. On light microscopy, these acidophilic structures stain bright red with eosin.
Rosenthal fibers have been described in reactive tissue (such as the highly gliotic tissue surrounding cysts and vascular malformations), in neoplasms (such as juvenile pilocytic astrocytomas), and in the genetic disorder Alexander disease
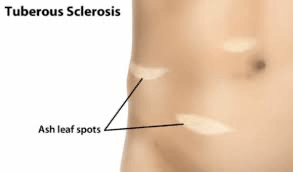
The patient in the picture is NOT likely to have this.

A. Lisch Nodules
B. Pheochromocytoma
C. Sphenoid dysplasia
D. Neurofibroma
E. Astrocytic periventricular hamartoma
What is E. Astrocytic periventricular hamartoma?

A 54-year-old male who is a heavy smoker presents with balance problems; below are his MRI scan and pathology slide from surgery. This is the most likely diagnosis.
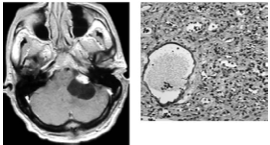
A) Metastasis
B) Hemangioblastoma
C) Glioma
D) CNS lymphoma
E) Pilocytic Astrocytoma
What is B. Hemangioblatoma?
The MRI shows an enhancing mural nodule with an associated cyst. Pathology shows highly vascular tissue and stromal cells characteristic of hemangioblastoma.
This is the approximate blood volume for a term neonate.
A. 90-105 ml/kg
B. 80-90 ml/kg
C. 70-80 ml/kg
D. 70ml/kg
E. 65 ml/kg
What is B 80-90 ml/Kg?
In general, approximate blood volumes are:
Pre-mature neonate 90-105 ml/kg
Term neonate 80-90 ml/Kg
Child 70-80 ml/Kg
Male adolescent 70 ml/Kg
Female adolescent 65 ml/Kg

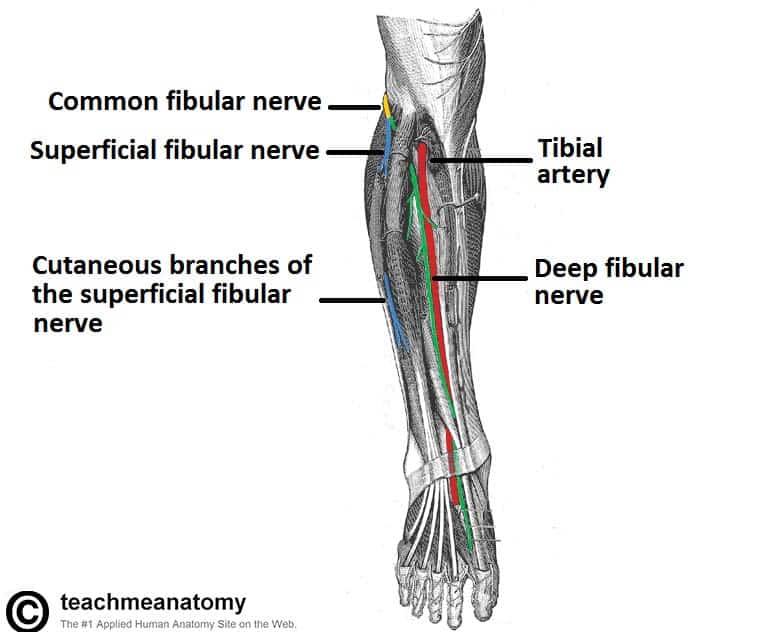
After a removal of a plaster cast for a tibia fracture following a bike accident, a 15 year old boy complains of paresthesias over the dorsum of his foot and finds he is unable to evert his foot, but is able to dorsiflex and invert.
This is the nerve most likely injured:
A) the deep peroneal nerve
B) the superficial peroneal nerve
C) the common peroneal nerve
D) the sciatic nerve
E) the tibial nerve
What is B. the superficial peroneal nerve?
The patient is suffering from superficial peroneal nerve entrapment. The superficial peroneal nerve innervates the peroneus longus and brevis, which evert the foot. A lesion of the deep peroneal nerve affects ankle dorsiflexion. A lesion of the common peroneal or sciatic nerve affects both ankle dorsiflexion and foot eversion. Sciatic nerve lesion also affects foot flexion and inversion.

Bilateral coronal craniosynostosis results in this.
A. Scaphocephaly
B. Anterior Brachycephaly
C. Posterior plagiocephaly
D. Harlequin eye deformity
E. Carinocephaly
What is B. Anterior Brachycephaly?

This tumor stains with S-100 protein immunoreactivity.
A. Anaplastic astrocytoma
B. Schwannoma
C. Ependymoma
D. Neurofibroma
E. Leiomyoma
What is B. Schwannoma?
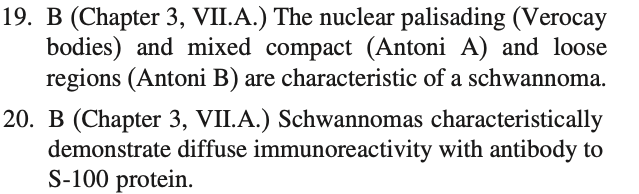
Of the following, this is FALSE regarding the syndrome that has a prominent feature illustrated in this CT scan
A) Involvement of the upper eyelid
B) Radiotherapy is not effective
C) Hemiparesis is contralateral to the facial lesion
D) The triad classically consists of nevus flammeus, venous malformation, and glaucoma.
E) Abnormalities of chromosome 9 are seen
What is E) abnormalities of chromosome 9?
Sturge-Weber syndrome occurs sporadically without mendelian inheritance and is of unknown etiology. Sturge-Weber syndrome is not inherited. The mutation that causes this disorder is somatic, which means it occurs after conception. In Sturge-Weber syndrome, the mutation is thought to occur in a cell during early development before birth. As that cell continues to grow and divide, the cells derived from it, specifically certain cells in the brain, eyes, and skin that are involved in blood vessel formation, also have the mutation, while the body's other cells do not. This situation is called mosaicism. The mosaic nature of the mutations helps to explain why the abnormal blood vessel growth occurs in some parts of the body but not in others.

This patient suffers from this type of spinal avm.

A) Type I - dural AVF
B) Type II - glomus AVM
C) Type III - Juvenile AVM
D) Type IV - perimedullary AVF
E) Type V - PeriHamadullary AVM
What is C. Type III: Juvenile AVMs?
•AKA metameric vascular malformations
•Intradural and extradural component
•Multiple feeders over several vertebral levels are common
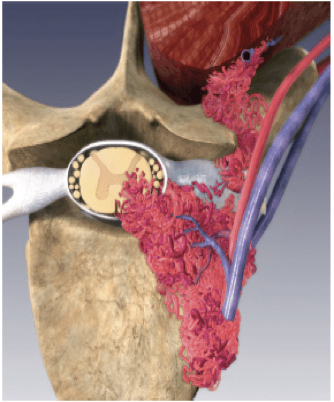
•High-flow lesion susceptible to hemorrhage
•Invasion of vertebral bodies may cause scoliosis
•Complete involvement of all embryologic layers has been described as Cobb’s syndrome
Massive blood transfusion is LEAST likely to be associated with this.
A. Iron overload
B. Hyperkalemia
C. Hypocalcemia
D. Hypothermia
E. Coagulopathy
What is A. Iron overload?
A massive transfusion is defined as a transfusion equaling the patient's blood-volume within 12-24 hours. The specific additional problems related to this scenario include:
-Volume overload resulting in non-cardiogenic pulmonary edema
- Thrombocytopenia:following storage there is a reduction of functioning platelets, so that there is a dilutional thrombocytopenia following a large transfusion
-Coagulation factor deficiency (relative) leading to a coagulopathy if concomitant cryoprecipitate/FFP not also transfused
-Hypothermia unless blood adequately warmed
-Hypocalcemia: Due to chelation by the citrate in the additive solution and may worsen coagulopathy
-Hyperkalemia: Due to progressive potassium leakage from the stored red blood cells
Of the following, this is NOT associated with the findings on this x-ray.

A. Weakness of hand
B. Horner's syndrome
C. Loss of the radial pulse
D. Torticollis
E. Ulnar paresthesias
What is D. Torticollis?
A cervical rib represents a persistent ossification of the C7 lateral costal element.[6][7] During early development, this ossified costal element typically becomes re-absorbed. Failure of this process results in a variably elongated transverse process or complete rib that can be anteriorly fused with the T1 first rib below.
The x-ray shows a cervical rib, usually associated with ulnar nerve weakness and paresthesia, Loss of radial pulse with rotating head to the ipsilateral side with extended neck following deep inspiration (Adson's sign) and compression of the sympathetic chain may cause Horner's syndrome
This genetic mutation is associated with craniosynostosis:
A. Rb
B. EGFR
C. TGF-B
D. FGFR
E. SOX2
F. MSH1
What is D. FGFR?
Genes most commonly mutated in craniosynostosis are FGFR2, FGFR3, TWIST1 and EFNB1. As well as being associated with syndromes, some clinically non-syndromic synostosis (usually affecting the coronal suture) can be caused by single gene mutations, particularly the Pro250Arg mutation in FGFR3.
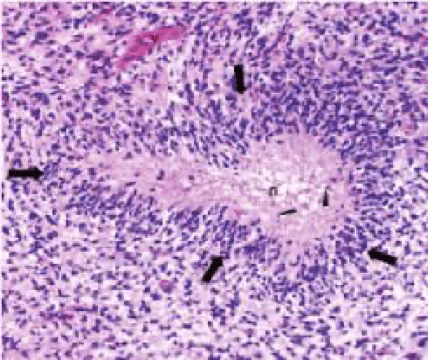
Prognosis in this tumor is most closely associated with deletion on this chromosome

A. 1
B. 3
C. 17
D. 20
E. 22
What is A. 1?
Pictured is an oligodendroglioma with typical 'fried egg' appearance. Deletions on chromosomes 1p and 19q are associated with chemoresponsiveness and better prognosis. The tumor represents a WHO grade II neoplasms and most common site is the frontal lobe.
Of the following, all are true of Lhermitte-Duclos disease EXCEPT:
A) It is also called dysplastic gangliocytoma of the cerebellum.
B) There is demyelination of the granular cell layer of the cerebellum.
C) There is thickening of one or more cerebellar folia.
D) Calcification and hydrocephalus may occur in this disorder.
E) A laminated pattern of folia on T2-weighted MRI is suggestive.
What is B. Demyelination of the granular cell layer of the cerebellum?
Lhermitte-Duclos disease is an uncommon cerebellar dysplasia that is characterized by hypertrophy of granular-cell neurons, and axonal hypermyelination in the molecular layer. Also known as dysplastic gangliocytoma of the cerebellum, it may occur in the setting of Cowden disease caused by a PTEN germline mutation. Mutation in PTEN gene on chromosome no. 10q leads to increased activity of AKT and mTOR pathways.
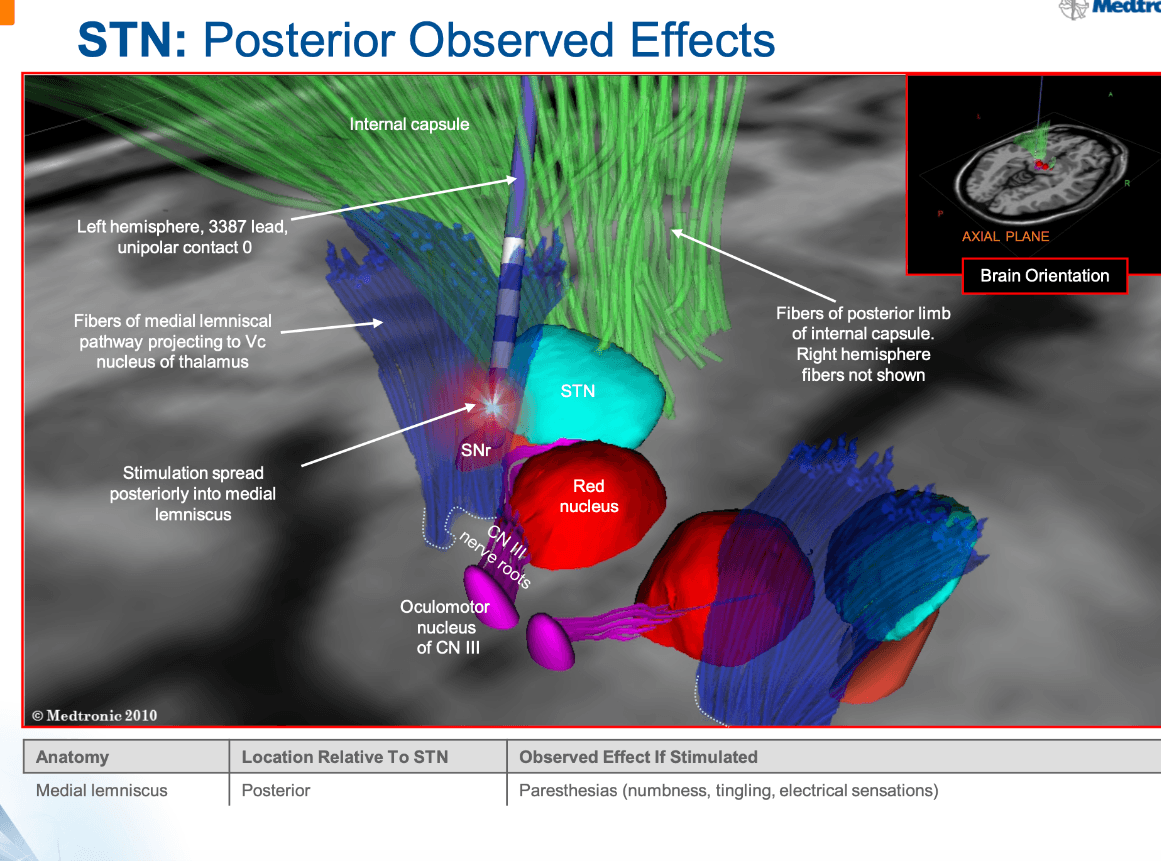
During a deep brain stimulation in the subthalamic nucleus for parkinsonian dyskinesias, the patient reports that he has paresthesias of the fingertips and the mouth. This effect happens when the lead is this:
A) anterior to the target.
B) posterior to the target
C) medial to the target.
D) lateral to the target.
E) Deep to the target.
What is B. Posterior the the target?
Paresthesias of the fingertips or mouth indicate that the electrode is too posterior (in the region of the medial leminiscus).
This is the most common inherited bleeding disorder
What is Von Willebrand's Disease?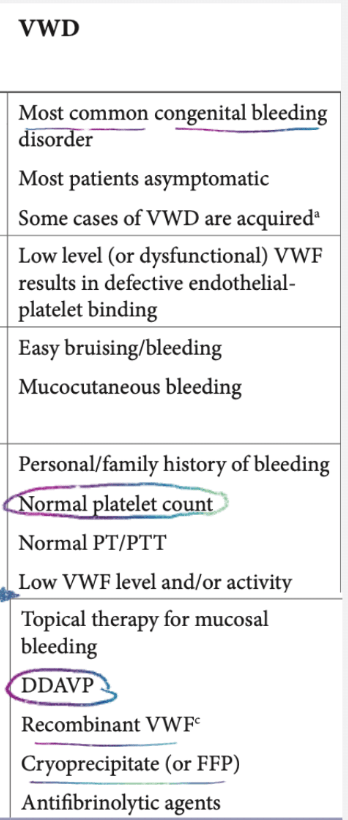
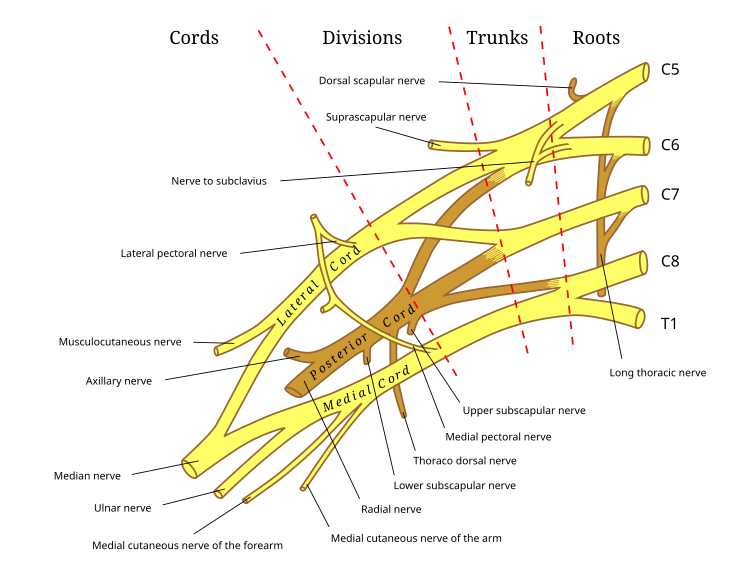
This brachial plexus structure is just distal to the division.

What is the cord?
The order of the brachial plexus structures is root, trunk, division, cord, branch.
The diagnosis:

What is positional plagiocephaly?

The circled structure is characteristic of this pediatric cerebellar tumor.
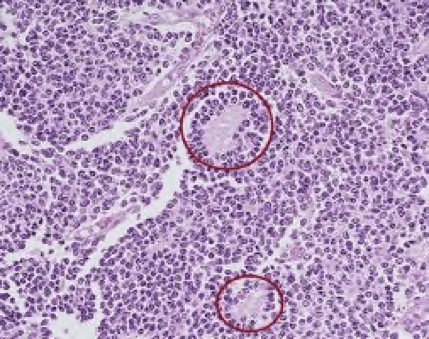
What is medulloblastoma?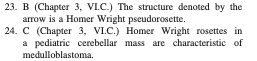
This deficit in lateral medullary syndrome is contralateral to the primary pathology
What is pain and temperature sensation of the body?

This pathology slide is characteristic of this tumor.
What is glioblastoma multiforme?
- 12 - 15% of adult intracranial tumors, 50 - 60% of astrocytic neoplasms
- Either primary (denovo, without recognizable precursor lesions, with p53 mutation) or secondary (develops slowly from grade II or III astrocytoma, often with partial #10 deletion)
- May be under graded on small stereotactic biopsies due to regional heterogeneity
- Median survival is 1 year; 5 year survival < 5%; survival may be overstated due to low grade tumors that dedifferentiate to glioblastoma (Cancer 2003;98:1745)
- Small cell morphology: associated with worse prognosis; poor prognosis even without necrosis or microvascular proliferation; typically have glioblastoma genetic features
A paradoxical effect happens when you give Warfarin alone because of this.
What is the short half-life of Protein C and S?
Warfarin inhibits the action of vitamin K, which γ-carboxylates glutamate residues on factors II, VII, IX, X as well as protein C + S.
When activated, Protein C and S cleave activated Factor V and Factor VIII.
You could become hypercoagulable by acutely decreasing protein C. In other words, while we typically think of warfarin acting against coagulation factors, it will ALSO decrease protein C. By having too little anticoagulant forces (too little protein C), we can become transiently hypercoagulable. Thus, BEFORE warfarin, we START with heparin/low molecular weight heparin, which will decrease the procoagulant forces transiently until the other coagulation factor levels fall


This patient, who denies any sensory changes, is suffering from this nerve entrapment
What is Anterior Interosseous Nerve Syndrome?
Pictured is the 'ok' sign.
- weakness of grip and pinch, specifically thumb, index and middle finger flexion
- patient unable to make OK sign (test FDP and FPL)
- normal median nerve sensory exam
- Compression of the AIN nerve (also known as Kiloh-Nevin's syndrome) is a forearm compressive neuropathy that results in motor deficits of the AIN nerve without sensory changes
- treatment involves a prolonged nonoperative course, and rarely, surgical decompression
Epideomology
- Incidence
- rare (<1% of median nerve neuropathies)
- Pathophysiology
- pathophysiology
- common causes
- transient neuritis (Parsonage-Turner syndrome)
- various anatomical cites of compression (see below)
- common causes
- pathoanatomy
- potential sites of entrapment of AIN
- tendinous edge of deep head of pronator teres
- most common cause
- fibrous arch of the FDS
- thrombosed radial, ulnar or anterior interosseous artery
- accessory head of FPL (Gantzer's muscle)
- accessory muscle from FDS to FDP
- abberant muscles (FCRB, palmaris profundus)
- tendinous edge of deep head of pronator teres
- patient with complete AIN palsy should have no motor function to all muscles innervated by AIN
- patients with Martin-Gruber anastomoses may also present with intrinsic weakness
- this is an anomalous anatomy in 15% of population where axons of AIN may cross over and connect to ulnar nerve and innervate other muscle groups (mainly adductor pollicis and dorsal interossei)
- patients with Martin-Gruber anastomoses may also present with intrinsic weakness
- potential sites of entrapment of AIN
- pathophysiology
- Associated conditions
- Parsonage-Turner Syndrome
- bilateral AIN signs caused by viral brachial neuritis
- be suspicious if motor loss is preceded by intense shoulder pain and viral prodrome
- Parsonage-Turner Syndrome
- Prognosis
- recovery generally begins 3 to 12 months after onset of symptoms with full resolution taking up to 18 months.
- patients < 40 years old noted to have faster recovery
- recovery generally begins 3 to 12 months after onset of symptoms with full resolution taking up to 18 months.
Anatomy
- Median nerve originates from the lateral and medial cords of the brachial plexus and travels between the biceps and brachialis as it heads towards the antecubital fossa
- The nerve travels deep to the lacertus fibrosis and gives a branch to the pronator teres
- AIN is terminal motor branch of median nerve
- AIN arises from the median nerve approximately 4 cm distal to the medial epicondyle (and 5-8 cm distal to lateral epicondyle)
- Travels between FDS and FDP initially, then between FPL and FDP, then it lies on the anterior surface of the interosseous membrane traveling with the anterior interoseous artery to pronator quadratus
- Terminal branches innervate the joint capsule and the intercarpal, radiocarpal and distal radioulnar joints.
- AIN has principally motor innervation (no cutaneous sensory) and innervates 3 muscles
- FDP (index and middle finger)
- FPL
- pronator quadratus
Presentation
- Symptoms
- common symptoms
- motor deficits without sensory loss
- may have vague complaints of deep forearm pain, but unlike other median compression neuropathies (carpal tunnel syndrome and pronator syndrome) pain can be absent
- if pain present, typically last only 2-3 weeks
- common symptoms
- Physical exam
- inspection
- severe disease may show forearm atrophy
- neurovascular
- weakness of grip and pinch, specifically thumb, index and middle finger flexion
- patient unable to make OK sign (test FDP and FPL)
- normal median nerve sensory exam
- provocative tests
- pronator quadratus weakness shown with weak resisted pronation with elbow maximally flexed
- distinguish from FPL attritional rupture (seen in rheumatoids) by passively flexing and extending wrist to confirm tenodesis effect in intact tendon
- if tendons intact, passive wrist extension brings thumb IP joint and index finger DIP joint into relatively flexed position
- inspection
Imaging
- MRI
- indications
- when concerned for a compressive mass lesion
- findings
- T2 or STIR images may show increased signal intensity in the FPL, FDP and PQ
- most reliable finding is edema in the PQ
- T2 or STIR images may show increased signal intensity in the FPL, FDP and PQ
- indications
Studies
- NCV / EMG
- indications
- helpful to make diagnosis
- may rule out more proximal lesions
- assess severity of neuropathy
- assess for nerve recovery
- helpful to make diagnosis
- findings
- EMG may reveal abnormalities in the FPL and FDP index and middle finger
- fibrillations, sharp waves, abnormal latency in the FPL and FDP
- EMG may reveal abnormalities in the FPL and FDP index and middle finger
- indications
Differential
- Tendon rupture
- Proximal sites of nerve compression (i.e cervical spine, brachial plexus)
- Pronator syndrome
- AIN syndrome differs from pronator syndrome in that it is a pure motor palsy
- pronator syndrome also involves sensory changes
- AIN syndrome differs from pronator syndrome in that it is a pure motor palsy
- Carpal tunnel syndrome
Treatment
- Nonoperative
- observation, rest and physical therapy
- indications
- first line treatment in all patients who do not have a space occupying lesion
- prognosis
- majority will improve with nonoperative management
- symptom resolution begins 3 to 12 months from onset of symptoms with full recovery taking up to 18 months
- mean full recovery is ~9 months
- symptom resolution begins 3 to 12 months from onset of symptoms with full recovery taking up to 18 months
- majority will improve with nonoperative management
- indications
- observation, rest and physical therapy
- Operative
- surgical decompression of AIN

- indications
- clear space occupying mass
- if nonoperative treatment fails after 12 months
- controversial in patients < 40 years old since some studies show patients in this age group uniformly respond to non-operative management.
- prognosis
- approximately 75% success rate of surgical decompression
- indications
- surgical decompression of AIN
Techniques
- Observation, rest and physical therapy
- technique
- given symptoms may take up to a year to improve, a prolonged course of observation is generally recommended in most patients
- massage and forearm stretches recommended during observation period
- technique
- Surgical decompression of AIN
- approach
- lazy-S incision over the proximal volar forearm centered over the anatomical area of most concern
- technique
- the AIN needs to be visualized proximal to distal with the following structures released
- detachment of superficial head of pronator teres
- lacertus fibrosus
- superficial arch of FDS
- Gantzer's muscle (if present)
- ligation of any crossing vessels
- removal of any space occupying lesion
- the AIN needs to be visualized proximal to distal with the following structures released
- post-operative rehab
- early motion encouraged with elbow ROM beginning post-op day 2
- approach
Complications
- Persistent AIN motor deficit
- incidence
- only ~5-10 cases reported in literature
- treatment
- tendon transfer
- brachioradialis to FPL transfer
- tendon transfer
- incidence
Contrary to its name, this unlucky newborn has what condition?


What is Clover leaf skull (associated with Pfeiffer syndrome)?
The disorder of Pfeiffer syndrome is an autosomal dominant disorder, probably caused by mutations in the gene for fibroblast growth factor receptor 1 of chromosome 8. The striking features of the syndrome are:
- broad, short thumbs and big toes. The proximal phalanx of the thumb is triangular or trapezoid, occasionally fused with the distal phalanx. Large alluces and partial syndactyly of the toes
- Ankylosis of the elbows
- Choanal stenosis
- Tracheal stenosis
- Stenosis and/or atresia of the external auditory canal, hypoplasia of the middle ear cavity with hypoplasic ossicles. The inner ear anatomy is normal.
- Craniosynostosis with fusion of coronal, lambdoid and sagittal sutures (cloverleaf skull)
- The intelligence is normal in some patients, and the development in the child after surgery appears to be normal.
This tumor is a bone-based sacrococcygeal mass.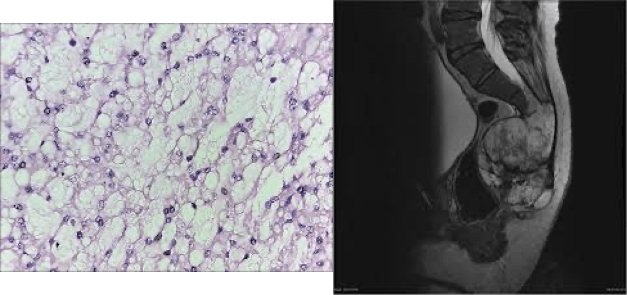
What is chordoma?
Myasthenia Gravis is characterized by these antibodies.
What is anti-nicotinic Acetylcholine receptors (Ach-R)?

This lesion in a 15 year old male causes pain that resolves with NSAIDs.
What is osteoid osteoma?
This CT reveals dense sclerosis around a lytic lesion with a central calcified nodule in the lumbar neural arch.

