Q: What type of PICC is this?
Valved open ended PICC
How do you decide the frequency of changing the indwelling catheter?
Base on the material of the catheter and other clinical indicators such as infection, encrustation, blockage, bypassing or catheter malfunction. No doctor's order is required regarding changing frequency.
What is Anasept?
- Anasept is a skin and wound cleansing solution containing an antimicrobial solution of 0.057% Sodium Hypochlorite
Why do we need to complete Braden scale for all our clients?
- A reliable VALIDATED tool to assess the risk of developing a Pressure injury used in conjunction with clinical judgment and part of a comprehensive Pressure injury prevention plan.
What is Pyoderma Gangrenosum?
A rare skin condition that causes large, painful wounds (ulcers) to develop on your skin, most often on your legs. The exact causes of pyoderma gangrenosum are unknown, but it appears to be a disorder of the immune system.
- What is the definition on a Pressure Injury?
- A pressure injury is localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device.. [as a] result of intense and/or prolonged pressure or pressure in combination with shear.
- When do we need to complete an ABI?
- Ankle Brachial Index for lower leg with wounds to determine blood flow status and healability and to determine if safe for compression therapy
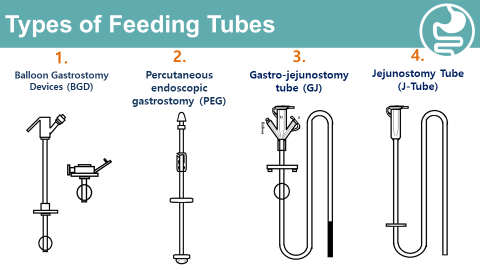
What type of the feeding tube can nurses change at bedside?
The Ballooned Gastrostomy Device (BGD) is the ONLY tube nurses can change at bedside.
- RN with additional education can replace the BGD once the stoma is mature
(4 weeks post-insertion). - Initial BGD change is completed by the physician
What do you use to clean CVC site? How long will you wait before you apply covering dressing after?
SoluPrep Swab-2% chlorhexidine gluconate and 70% alcohol. Alcohol provides instant bactericidal action to the skin surface and CHG provides long acting anti-microbial action
The skin must be completely dry before applying the securement device and covering dressing (3-5 mins). 1. Solution must be dry for maximum anti-microbial effect.
2. If not completely dry, CHG can react with the dressing adhesive and causing a chemical burn to the client's skin
What is physician's responsibilities regarding long term indwelling catheter?
1. To perform first S/P catheter change after initial insertion
2. To provide orders for
Insertion of long-term urinary catheter
Insertion of Coude and S/P catheters
Discontinuation of all urinary catheters
Must clearly state the reason for the indwelling catheter e.g. Atonic bladder, urinary retention, neurogenic bladder.
What is BIATAIN IBU?
- Biatain IBU is a Polyurethane foam dressing which contains Ibuprofen (Ibu) 0.5gm/cm2 homogeneously dispersed throughout the dressing(analgesic dressing )
How often do we need to complete Braden Scale in HH?
Braden Scale is done on admission
- If at risk with score 18 or less, reassess clients:
- Community care: every visit for first 3 weeks, then quarterly and following hospitalization.
What is IAD?
- IAD: Incontinent Associated dermatitis
- What does a STAGE X mean?
- Unstageable - The depth of the wound can not be determined.
Can we apply compression therapy with ACUTE S.S of infection?
Hold compression with acute s.s infection (heat, pain and redness and reassess )
what do you teach your client for daily care to his/her BGD?
- Clean the stoma site and feeding tube with water and mild soap.
- Q-tip can be used to clean the ports of debris.
- Verify the bolster is floating 2 to 3 mm above the skin.
- Check the tube position. If the tube length changes by 2.5 cm, the tube might have moved out of the stomach
- Rotate the BGD 360o degrees plus a quarter turn daily. (Do not rotate a GJ or J-Tube or any sutured tube.)
Mr. Smith is on Cloxacillin 2g Q4H with CADD Solis VIP pump infusion. The first dose starts at 14:00 and each dose runs for one hour. What time frame will you go to visit Mr. Smith for daily medication bag change?
After 11am and before 2pm every day.
True or False: It is the best practice to change leg urinary bag and night bag every day
Answer: False
The urinary drainage bag should only be changed when odorous, discolored, leaking or with the catheter change. The best practice is keeping a closed urinary drainage system to decrease risk of infection
What is Mesalt?
- Hypertonic saline impregnated gauze that creates an environment to draw gently exudate, debris and edema out from the wound.(debride )
What other assessment need to be done when completing the Braden Scale?
Head to Toe skin assessment
What may be the cause of lower leg cellulitis?
- Edema , trauma , blisters , not wearing compression stockings
what stage is this Pressure Injury?
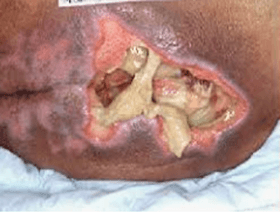
Stage 4
What level of compression is a Coban lite?
- 20-30 mmHg
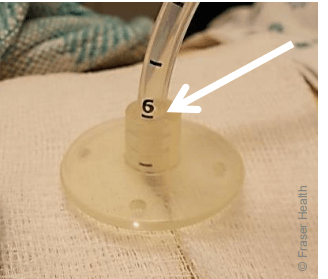
How often to check the balloon for Ballooned Gastrostomy Device (BGD) and why the balloon needs to be checked?
- Check the balloon every 7 days.
- The water can leak out over time. If too much water leaks out of the balloon, the tube could fall out.
Mrs. Smith is on Ertapenem 2g IV gravity daily. The total bag volume is 120ml and infusion time is 30 mins. Home Health use 10drops/ml IV tubing. What is the IV drip rate?
Total bag volume (120ml)x10/30 mins=40 drops/min
What would you do if the suprapubic catheter does not insert?
1. Try to insert a new catheter, one size smaller than previous catheter
2. If client is spasming, wait until spasm is resolving then try again
3. If unable to insert catheter, call urologist for further direction
4. Tell the client to go to emergency
What is HFB?
- An absorbent polyvinyl alcohol foam (PVA) containing Methylene Blue and Gentian Violet which provides a broad-spectrum antibacterial activity effective against a variety of bacteria and yeasts
Where do you document Braden Scale score?
Paris and Pixalere (wound care clients)
How can we correct venous insufficiency of the lower leg?
- Compression therapy
What stage is this Pressure Injury?
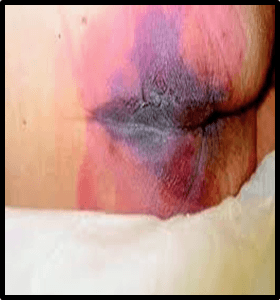
Deep tissue injury
- What level of compression can we achieve with Tubigrip application?
- 10-20mmHg
When does the client start to check the balloon for Ballooned Gastrostomy Device (BGD)?
Starting 4 weeks after the tube is put in.
if there is a big different between the amount you pull out and the amount of water originally put in, the balloon might be leaking. Recheck in 10 minutes, if there is still big difference in amount, the tube might need to be replaced.
Fill up blanks regarding CADD pump IV abx infusion
Medication bag change Q________
Tubing change Q_________
Battery change Q__________
PICC dressing change Q_______
PICC flushing Q____________
Medication bag change: Q day (usually)
Tubing change: Q Week
Battery change: Twice a week
PICC dressing change: Q Week
PICC flushing Q Week (If medication end with cillin-Cloxacillin will require daily flushing)
What are the possible signs and symptoms of urinary retention?
1. Dull sound with percussion (Dull sound to umbilicus indicates about 500ml of urine)
2. Lower abd pain/tenderness
3. Increased BP
4. Inability to void even though sensation to void is present
5. Diaphoresis
6. Frequent and small voids (less than 50 ml)
7. Restlessness or agitation (with or without cognitive impairment)
8. Incontinence of urine or feces/continuous leakage (fecal oozing)
What is a precaution we need to be aware of with using HFB?
Do not allow the dressing to dry out • The use of the dressing should not extend beyond six months without a clinical review by Physician/NP/ NSWOC/ Wound Clinician • The use of dressing for pregnant or breastfeeding women has not been studied for safety
Provide 3 interventions you may implement to prevent pressure injuries?
Repositioning Q 2 h when bed bound , OT referral , Dietician referral , increase protein intake
Should we elevate the leg with arterial disease?
No leg elevation due to increased pain with elevation with arterial disease (moderate to severe )
What stage is this Pressure Injury

Stage 2
When is Compression contra indicated?
Severe pain, DVT, SOB ,Arterial compromise (moderate –severe ) and acute infection.
What client needs to do if the Ballooned Gastrostomy Device (BGD) falls out accidently?
The stoma hole can close quickly. Contact with nurse or go to nearest ER as soon as possible. Bring the old tube and the new tube if client has one at home. If a tube is not available, a urinary catheter could be put in through the stoma to keep it open.