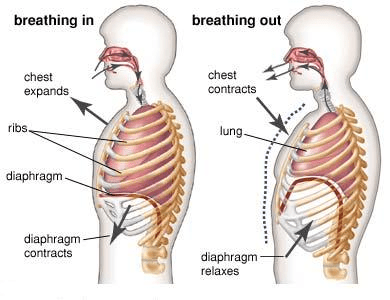
The diaphragm contracts. Increasing lung volume, and making the pleural pressure more negative. Air to rushes in and fills the lung.
Inspiration
For NIV to be successful this device seal must be adequate
Mask
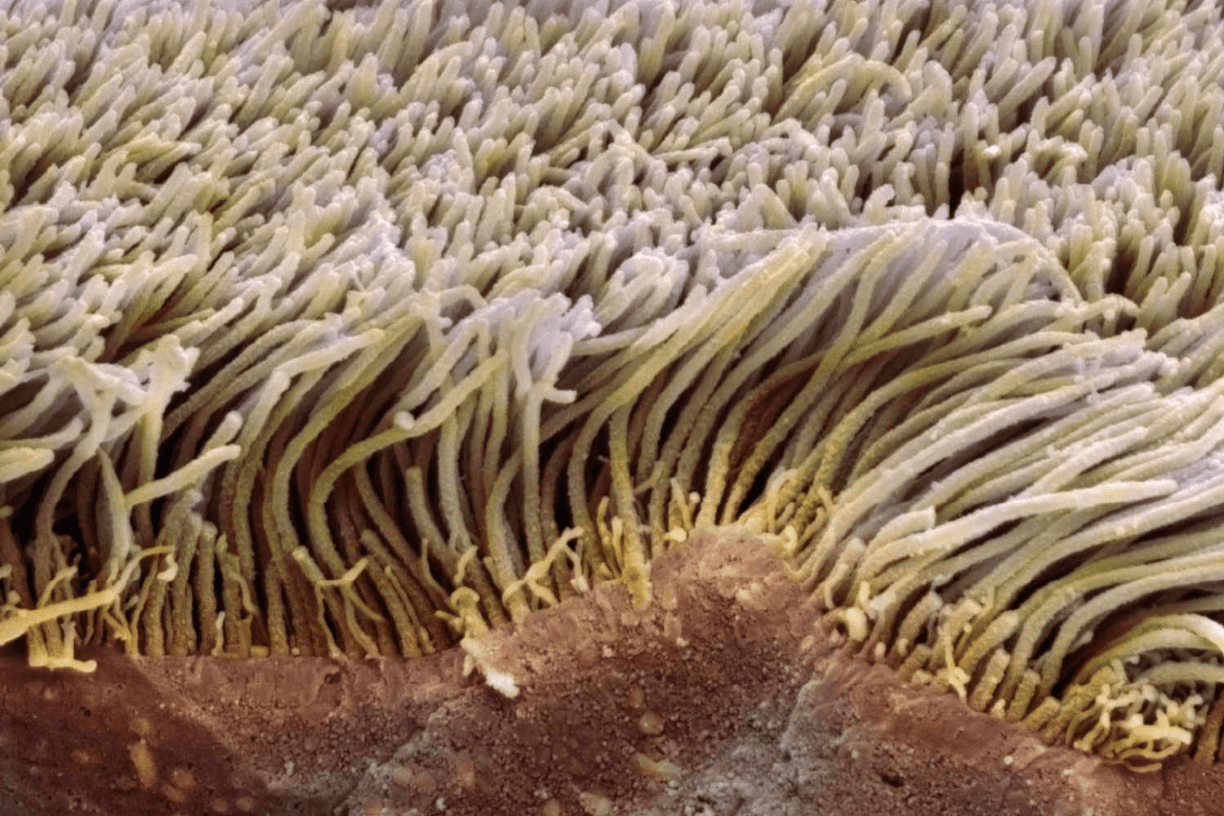
I move particles at a rate of 3mm per min to the larynx where these particles are either coughed up or swallowed.
Cilia
The difference between IPAP and EPAP
Pressure Support - PS
PS provides ventilatory support during the inspiratory phase of ventilation
Characterised by Low Pa02 (Pa02 <50mmHg) but C02 is not elevated (paC02 <60 mmHg).
Type 1 Respiratory Failure or Hypoxemic Respiratory Failure
The diaphragm relaxing, and intrinsic recoil of the lungs allowing air to be expelled passively
Expiration
To assess the effectiveness of NIV _______ should be taken as a baseline 1 hour after commencement and 1 hour post setting changes to assess effectiveness.
Blood Gas (arterial or venous)
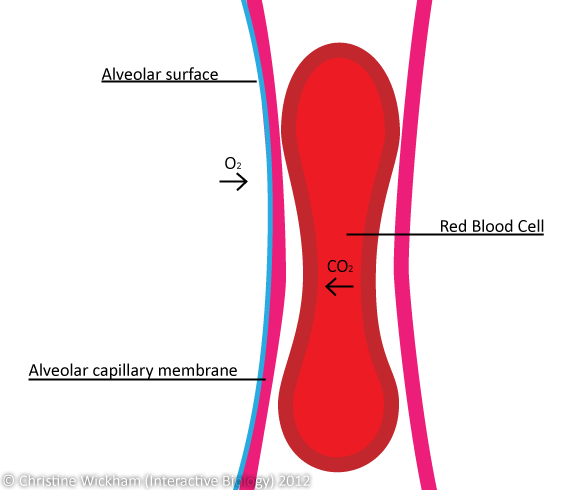
I form 70-80 sq meters of surface area in close contact with capillaries for gas exchange.
Alveoli

Respiratory support to improve oxygenation, patient breathes against resistance throughout the respiratory cycle.
Previously closed airways are opened, atelectasis is decreased & surface area for gas exchange is increased resulting in increased arterial oxygenation
CPAP (Continuous Positive Airway Pressure)
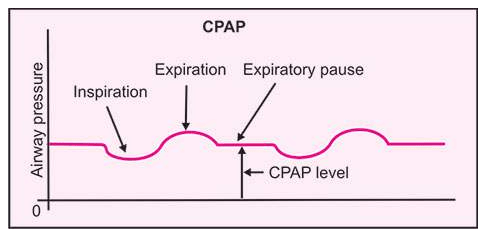
Supports oxygenation - not ventilation (movement of air into the lungs)
Commonly used for acute APO in addition to standard therapy.
Characterised by low Pa02 (<50mmHg) and elevated PaCO2 (>60mmH)
Type 2 Respiratory Failure
During quiet breathing the amount of air that is inspired and expired
Tidal Volume - TV
The Below device goes by the acronym DEP, name the correct terminology:
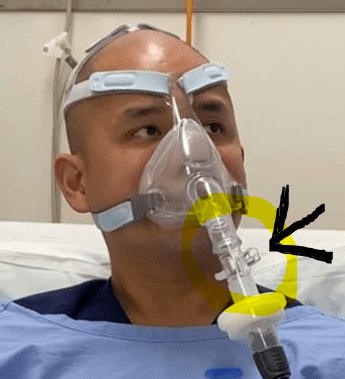
Disposable Exhalation Port
When in network for gas exchange, each red blood cell passes by me single file, and spends approximately 3/4 seconds to exchange 02 or C02
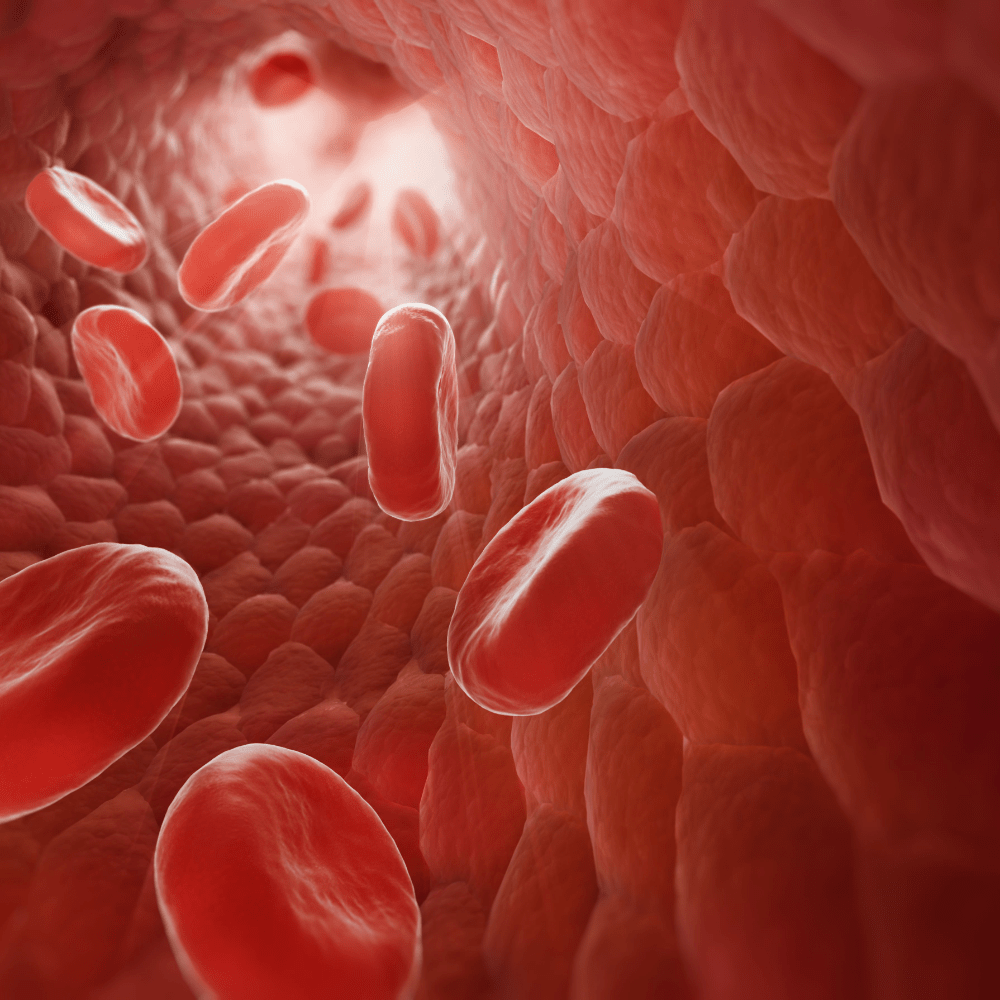
Capillary Membrane
Respiratory mode that means the pressure varies within each breath cycle.
BiPAP (Spontaneous/timed)
EPAP and IPAP settings are determined by the abnormalities requiring correction
In hypoxia, a high EPAP guarantees alveolar ventilation
In hypercapnia, a high IPAP gives more volume for diffusion.
A build up of fluid in the interstitial space of the lungs
APO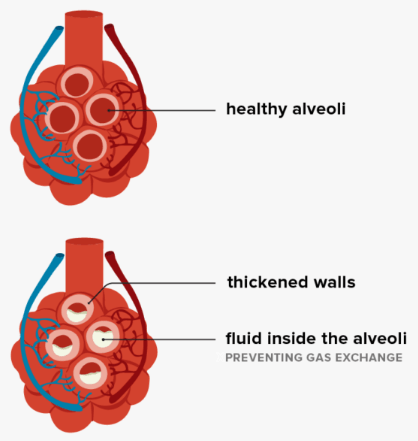
The lungs ability to stretch and expand
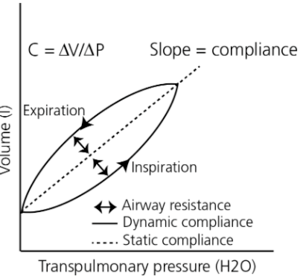 Lung compliance
Lung compliance
The delivery of positive pressure ventilation to a spontaneously breathing patient to augment breathing and ventilation
Non-Invasive Ventilation
It takes 0.25 seconds for these levels to reach normal saturation when exposed to alveolar gas
haemoglobin
A pressure applied at end expiration
Used to increase functional residual capacity of the lungs and decrease airway collapse.
EPAP
Pressure drops, exhalation is against less resistance. Prevents airway collapse acting as a splint. Minimum of 5cmH20 to overcome intrinsic airway collapse.
Loss of elasticity, the walls between alveoli are destroyed, alveoli become large and floppy because there is less surface area for gas exchange, airways are thick, inflammed and there is increased mucus production
Chronic Obstructive Pulmonary Disease - COPD
Volume in the alveoli after passive expiration
Functional Residual Capacity
Important to keep small airways open, thus prevention areas of collapse and allows for continual gas exchange.
Bilevel support is provided, but the patient is able to initiate breaths with a constant inspiratory time (I time).
If the intrinsic respiratory rate there is also the back up rate available (with the same fixed I time).
What ventilation mode is this?
Pressure Control Ventilation (PCV)
A gas that diffuses 20 times more rapidly than oxygen
C02
The delivery of positive pressure during Inspiration.
Increasing the patient's tidal volume and supporting alveolar ventilation.
IPAP
On Inhalation pressure rises and augments breath. Allows resting of inspiratory muscles and improves hypercapnia with increased volume.
Blood flowing past poorly ventilated alveoli that does not exchange gas.
Poorly oxygenated blood then lowers the total oxygen content of the arterial blood - leading to hypoxaemia.
Shunt/shunting
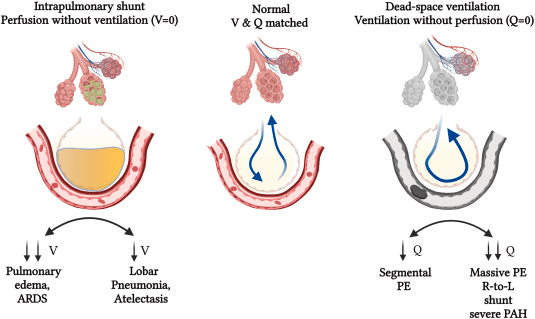
Common causes of shunt include:
- pnueomnia and pulmonary odeoma
- tissue trauma - alveolar wall swelling
- atelectisis collapse of alveoli from failure to expand
- mucus plugging