A 62-year-old woman with severe COPD (FEV1 36% predicted) is admitted to the hospital with an acute exacerbation of COPD. This is her third hospitalization for an acute exacerbation of COPD in the past 2 years. She benefitted from acute noninvasive ventilation, responded well to in-hospital management, and did not experience any complications. Discharge from the hospital is being arranged, and her pharmacologic therapy is being optimized. Planned discharge medications include combination inhaled corticosteroid/long-acting ß2-agonist/long-acting muscarinic antagonist and oral N-acetylcysteine, in addition to as-needed albuterol. Arterial blood gas results on room air are as follows:
- pH, 7.39
- PCO2, 41 mm Hg
- PO2, 48 mm Hg HCO3, 26 mEq/L (26 mmol/L)
She will be discharged on continuous supplemental O2 2 L/min (SpO2 93% with O2 2 L/min). She is a nonsmoker, received the influenza vaccination 2 months prior to hospital admission, and is up-to-date with appropriate pneumococcal vaccination. Which of the following additional interventions has been shown to be associated with a reduction in all-cause mortality in this setting?
A. Long-term nocturnal noninvasive ventilation
B. Participation in pulmonary rehabilitation within 3 months of hospital discharge
C. Roflumilast
D. Endobornchial valve(s) insertion
B. Participation in pulmonary rehabilitation within 3 months of hospital discharge
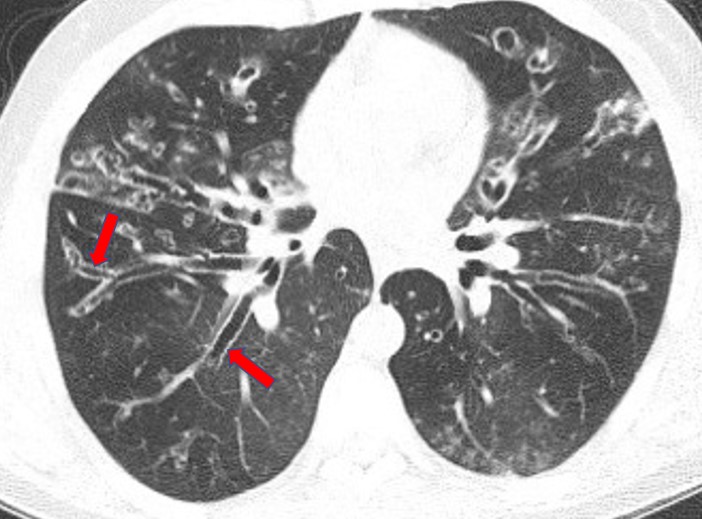
A 68-year-old woman with no history of smoking or asthma presents with several years of progressive dyspnea and cough that is productive of thick yellow sputum. She reports no seasonal allergies and nasal congestion. Her medical history reveals mild hypertension and no childhood respiratory diseases. She never worked in an industrial setting and has raised five healthy children. Examination results reveal coarse rhonchi and faint wheezes. Spirometry results demonstrate moderate obstruction, and a chest CT scan (Figure 1) was obtained after a chest radiograph revealed subtle abnormalities.
Which of the following statements is correct?
A. This condition has an equal prevalence among men and women.
B.Sputum colonization with Staphylococcus aureus is associated with more severe disease.
C. With diagnostic testing, a specific cause of this condition can be determined in 80% to 90% of patients.
D. Even when started early, inhaled antibiotics do not benefit most patients.
D. Even when started early, inhaled antibiotics do not benefit most patients.
A 25-year-old woman with a history of asthma since age 15 reports worsening asthma control days before her menses, with increased need for rescue bronchodilator therapy. She is a nonsmoker and is maintained on an inhaled steroid and a leukotriene receptor antagonist. She reports no seasonal variation. Her BMI is 30 kg/m2.
What is the best next intervention to control symptoms in this patient?
A. Add a long-acting β2-agonist.
B. Advise daily nonsteroidal anti-inflammatory drugs prior to menstruation.
C. Start estrogen replacement therapy.
D. Refer for salpingo-oophorectomy.
A. Add a long-acting β2-agonist.
You consult with a 55-year-old man for evaluation of progressive dyspnea on exertion over the past year. The patient has a history of asthma dating back to childhood with an associated finding of allergic rhinitis. He has smoked intermittently over the years, with a cumulative history of about 10 pack-years. The patient has been admitted to the hospital for acute episodes of dyspnea, wheezing, and hypoxemia on three occasions over the past 20 years. His blood cell counts have shown intermittent eosinophilia. The patient is treated with a combination inhaler (long-acting β-agonist and inhaled steroid) and has been adherent to his regimen.
His medical history is notable for prediabetes mellitus, hypertension, and hyperlipidemia. He has no pets after he discovered he had allergies to animal dander. He works on a road construction crew.
On examination, he is comfortable sitting at 90°; his Spo2 is 94% without supplemental oxygen. His BP is 140/85 mm Hg, heart rate is 88/min, and respiratory rate is 18/min. Jugular venous pressure is 8 cm above the right atrium. His chest is resonant to percussion with a few scattered expiratory wheezes. His heart sounds are normal; no gallop or murmur is noted. His abdomen is soft with no guarding or tenderness. His extremities are negative for clubbing and edema.
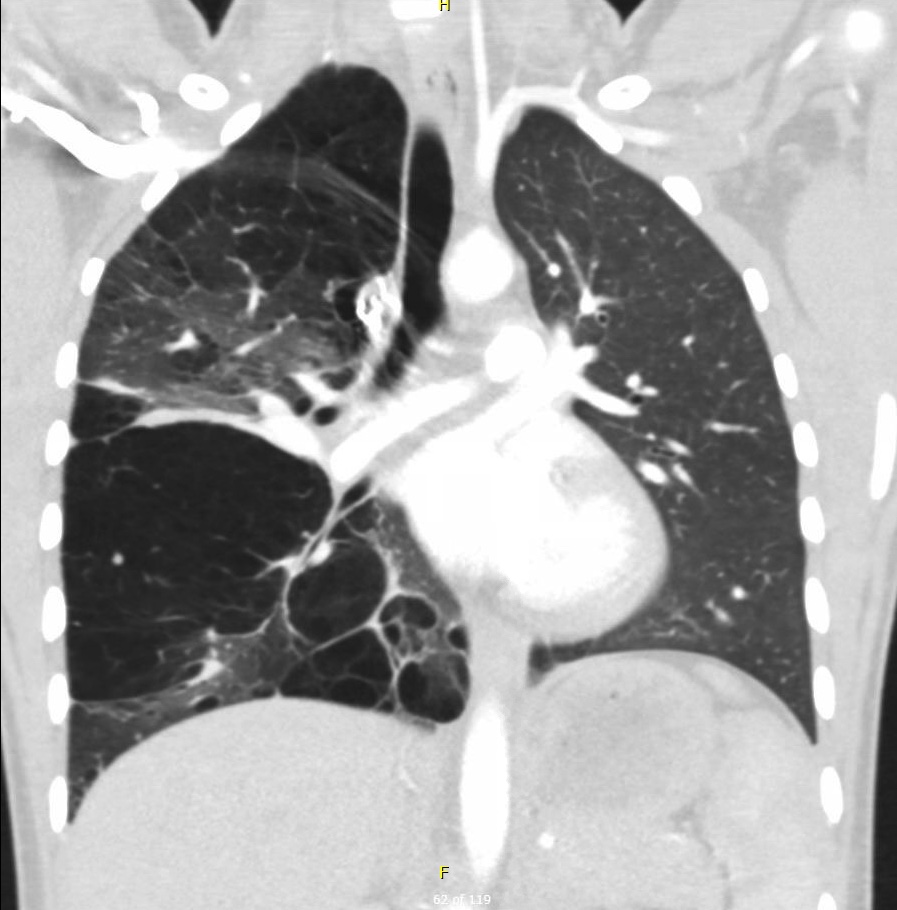
Pulmonary function test results are as follows: FVC, 2.75 L (85% predicted); FEV1, 1.85 L (75% predicted); FEV1/FVC, 67%; total lung capacity, 5.71 L (115% predicted); functional residual capacity, 3.4 L (112% predicted); and residual volume, 2.33 L (120% predicted). There is minimal bronchodilator response. A chest radiograph is shown in Figure 1.
What is the most likely diagnosis?
A. Asthma
B. Emphysema
C. Asthma-COPD overlap
D. Combined pulmonary fibrosis and emphysema
C. Asthma-COPD overlap
A 63-year-old woman with advanced COPD is referred to you because of worsening shortness of breath. She gets short of breath and must stop after walking approximately 367 ft (110 m). She has a prior 60 pack-year smoking history but has been a nonsmoker for 4 years. She has been hospitalized on two occasions for acute exacerbation of COPD but has no other significant comorbid conditions. Her vaccinations are up-to-date. She is adherent to her medications, which include an inhaled long-acting muscarinic antagonist and a combination inhaled corticosteroid/long-acting β2-agonist, as well as albuterol as needed. Physical examination is consistent with advanced COPD. A chest radiograph demonstrates striking vascular deficiency and hyperlucency, with no masses, adenopathy, or effusions. Pulmonary function testing reveals FEV1 of 0.73 L (29% predicted), FEV1/FVC of 0.36, residual volume of 3.97 L (180% predicted), and DLco of 8.9 mL/min/mm Hg (40% predicted).
You are considering evaluation to assess whether the patient might benefit from endobronchial valve insertion. Before proceeding with further investigations, the patient asks for more information. Which of the following statements regarding outcomes from endobronchial valve insertion in this patient with advanced COPD are true?
A. Upper lobe emphysema and low exercise capacity are necessary for benefit.
B. Pneumothorax is the most common adverse effect.
C. The 6-min walk distance but not FEV1 improves following insertion.
D. St. George's Respiratory Questionnaire score improves in the short term but returns to baseline at 12 mo.
B. Pneumothorax is the most common adverse effect.
![]()



A 24-year-old man is referred for treatment of newly diagnosed cystic fibrosis. He is originally from the Dominican Republic and has had recurrent respiratory infections since early childhood. After moving to the United States 8 months ago, he was evaluated for diffuse bronchiectasis, and a sweat chloride test result was abnormal. Genetic test results were positive for homozygous F508del mutation.
In addition to vaccination, nutritional interventions, bronchodilators, and sputum clearance measures, treatment with which of the following is most likely to benefit the patient?
A. Elexacaftor plus tezacaftor plus ivacaftor
B. Ivacaftor
C. Lumacaftor plus ivacaftor
D. Tezacaftor plus ivacaftor
A. Elexacaftor plus tezacaftor plus ivacaftor
A 30-year-old woman (G1P0) in her ninth week of pregnancy seeks consultation for adjustments in her asthma regimen. Her current medical regimen includes medium-dose inhaled corticosteroids (fluticasone) twice per day and as-needed albuterol. She has been stable (no awakenings, using albuterol once per week, no limitations) with this current regimen. She had an acute exacerbation 8 months previously that required a regimen escalation but is now back with her usual regimen. On examination, her vital signs are stable, and her lungs are clear without wheezing.
Which of the following do you recommend?
A. Continue the current medical regimen.
B. Change fluticasone inhaled corticosteroid (ICS) to equivalent dose budesonide ICS.
C. De-escalate regimen to an as-needed short-acting β-agonist.
D. Measure fractional exhaled nitric oxide to determine next steps.
A. Continue the current medical regimen.
You consult with a 50-year-old man with a history of asthma since childhood. The asthma was generally well controlled with bronchodilator and corticosteroid inhalers, with an occasional need for a short course of prednisone. Over the past 10 years, however, he has had more frequent episodes of respiratory infections with wheezing, requiring corticosteroid treatment. He has developed a chronic cough over the past 5 years productive of mucus plugs, some of which are very dark in color. Once or twice, he has noticed a small amount of blood in the mucus.
The patient is a nonsmoker. His medical history is notable for gastroesophageal reflux; he regularly undergoes endoscopy because of a concern for Barrett esophagus. He also has a history of environmental allergies.
On examination, he appears comfortable sitting at 90°. Jugular venous pressure is 7 cm above the right atrium. His chest is resonant to percussion, with scattered rhonchi and wheezes bilaterally. His heart sounds are normal without gallop or murmur. Abdominally, he has mild epigastric tenderness without guarding. There is no clubbing or edema of the extremities.
Results from laboratory studies 4 weeks ago include an absolute blood eosinophilia count of 500/μL (0.5 × 109/L) and an IgE level of 1,200 IU/mL. Allergy skin testing showed reactivity to animal danders, pollen, and Aspergillus. Electrolyte levels and renal function were normal.
Spirometric results are as follows: FVC, 2.90 L (90% of predicted); FEV1, 1.93 L (78% of predicted); FEV1/FVC, 67%; total lung capacity, 4.90 L (98% of predicted); functional residual capacity, 2.90 L (95% of predicted); and residual volume, 2.0 L (110% predicted). FEV1 increased 15% with an inhaled bronchodilator. A chest radiograph is shown in Figure 1.
What is the most likely diagnosis in this patient?

A. Allergic bronchopulmonary aspergillosis
B. Eosinophilic granulomatosis with polyangiitis
C. Hypereosinophilic syndrome
D. Bronchiectasis from recurrent aspiration
A. Allergic bronchopulmonary aspergillosis
A 69-year-old man with COPD whose therapy is high-dose fluticasone, salmeterol, and tiotropium is inquiring about initiation of roflumilast because of a history of multiple annual exacerbations requiring corticosteroids.
Which one of the following clinical and physiological/laboratory characteristics would make him most suitable for initiation of this medication?
A. Symptoms of chronic bronchitis, at least one hospitalization for an exacerbation in the previous year, and FEV1 less than 50% predicted
B. Former smoker, multiple exacerbations in the previous year, and FEV1 less than 80% predicted
C. Recurrent pneumonia and oropharyngeal candidiasis, multiple exacerbations in the previous year, and blood eosinophil count less than 100/µL (0.10 × 109/L)
D. COPD Assessment Test score of 10 or greater, multiple exacerbations in the previous year, and blood eosinophil count of 100/µL (0.10 × 109/L) or greater
A. Symptoms of chronic bronchitis, at least one hospitalization for an exacerbation in the previous year, and FEV1 less than 50% predicted
A 65-year-old woman presents for evaluation of chronic cough and daily sputum production. She had been previously well without upper or lower respiratory symptoms, rhinosinusitis, or pulmonary disease until she noted the gradual onset of cough about 18 months ago. At physical examination, she had normal vital signs. She was a thin but otherwise well-appearing woman. Lung examination revealed crackles and inspiratory squeaks and pops in the middle lung field bilaterally. Pulmonary function test results showed a total lung capacity of 100% predicted, residual volume of 140% predicted, FVC of 85% predicted, FEV1 of 75% predicted, FEV1/FVC of 0.65, and DLCO of 85% predicted. A chest CT scan is shown in Figure 1.
Which of the following tests is most likely to elucidate the diagnosis?
A. Sputum culture for nontuberculous mycobacteria
B. Serum immunoglobulin testing
C. Sweat chloride testing
D. Gene testing for primary ciliary dyskinesia
A. Sputum culture for nontuberculous mycobacteria
A 25-year-old woman presents for evaluation of shortness of breath and chest tightness that occurred 15 min after completing a winter half-marathon running race. Symptoms lasted about 60 min and then resolved without treatment. She had prepared for the run on her treadmill following a marathon training protocol. She has no history of asthma and does not smoke or vape. Other than a mild upper respiratory infection the week before the race, she has been in good health. Results from spirometry with bronchodilator testing performed 1 week after the event are normal.
Which of the following tests will most likely yield the diagnosis?
A. Technetium-99m sestamibi exercise test
B. Laryngoscopy with videostroboscopy
C. Eucapnic voluntary hyperpnea test
D. Expiratory high-resolution CT imaging
C. Eucapnic voluntary hyperpnea test
A 20-year-old patient with documented hereditary angioedema and low C1 esterase level has been maintained with reasonably few attacks on a home regimen including subcutaneous administration of lanadelumab. Today she began having breakthrough symptoms, including abdominal pain and areas of nonpitting, nonpruritic swelling notable on the arms and trunk. She has not had an episode of airway obstruction in the past but now feels some tightening at the back of her throat when she swallows. You evaluate her airway bronchoscopically in the ED, and there is mild laryngeal edema, but her airway is not compromised to a point requiring intubation. She is being admitted to the ICU for observation.
Which medication would have the most significant and most rapid effect on reversing her symptoms and the anatomic effects of edema?
A. Inhaled racemic epinephrine
B. IV epinephrine
C. IV methylprednisolone
D. Subcutaneous icatibant
D. Subcutaneous icatibant
A 55-year-old man with a 10-pack-year smoking history reports cough, sputum production, and mild dyspnea with exertion over the past 3 years. Spirometry reveals reduced FEV1 and FVC, with a preserved FEV1/FVC ratio (greater than 0.70 and above the lower limit of normal). His total lung capacity is normal. There is no evidence of interstitial lung disease or emphysema on CT scan of the chest, and his BMI is within normal range.
Based on population studies, which of the following statements regarding this patient is true?
A. This presentation is rare among smokers who undergo spirometry.
B. Lung function in this patient will progress to a reduced FEV1/FVC ratio.
C. The history is typical of a specific genetic variant of COPD.
D. This patient's mortality risk is higher than that of smokers with normal lung function.
D. This patient's mortality risk is higher than that of smokers with normal lung function.
A 34-year-old patient with cystic fibrosis (CF) who is homozygous for Phe508del sequence variation presents for follow-up. The patient has advanced lung disease with baseline FEV1 of 38% predicted, chronic Pseudomonas aeruginosa colonization, pancreatic insufficiency, and CF-related diabetes mellitus. They report stable symptoms and adherence to prescribed medications, including highly effective CF transmembrane conductance regulator (CFTR) modulator therapy, pancreatic enzyme replacement therapy, and an inhaled antibiotic. Given that they are now receiving a CFTR modulator, the patient asks about the utility of airway clearance therapies and other chronic medications.
Which of the following is accurate guidance about adjunctive therapies in the setting of treatment with a CFTR modulator?
A. Inhaled antibiotics are no longer necessary owing to alterations in the airway microbiome.
B. Airway clearance therapies should be continued owing to irreversible structural lung damage.
C. Pancreatic enzyme replacement therapy is not as effective owing to restoration of exocrine pancreas function.
D. Dornase alfa is not effective owing to changes in airway surface hydration.
B. Airway clearance therapies should be continued owing to irreversible structural lung damage.
A 30-year-old man with poorly controlled asthma and chronic rhinitis comes in for evaluation, and he inquires whether immunotherapy will help his asthma. He is maintained on high-dose inhaled corticosteroids, a long-acting β2-agonist, a leukotriene receptor antagonist, a nonsedating antihistamine, and a nasal topical steroid. Despite this, he reports persistent nasal congestion and almost daily use of his rescue inhaler when inside his home. He states he adheres to his medical regimen, and you observe his inhaler technique and find it acceptable. His lung function demonstrates an FEV1 of 55% predicted, with postbronchodilator reversibility. His house dust mite–specific IgE antibody level is high, and his serum eosinophil count is elevated.
Which of the following would you recommend?
A. Use allergen immunotherapy to reduce symptoms as seen in studies of similar patients.
B. Subcutaneous immunotherapy should be started to improve nonspecific airway hyperreactivity.
C. Obtain impermeable pillow and mattress covers to reduce bronchodilator use.
D. Immunotherapy should not be considered at this time because of poor asthma control.
D. Immunotherapy should not be considered at this time because of poor asthma control.
An 18-year-old patient with a history of exercise-induced asthma presents to the ED with dyspnea and right-sided pleuritic chest pain that started while on vacation in Colorado. The pain started gradually while the patient was hiking but has gotten worse over the past 3 days as they drove back home to Texas; it is now so severe that they cannot take deep breaths or sleep. The patient has no cough, fevers, calf pain, or leg swelling. There is no prior history of respiratory infections or smoking. The patient does not take any medications regularly.
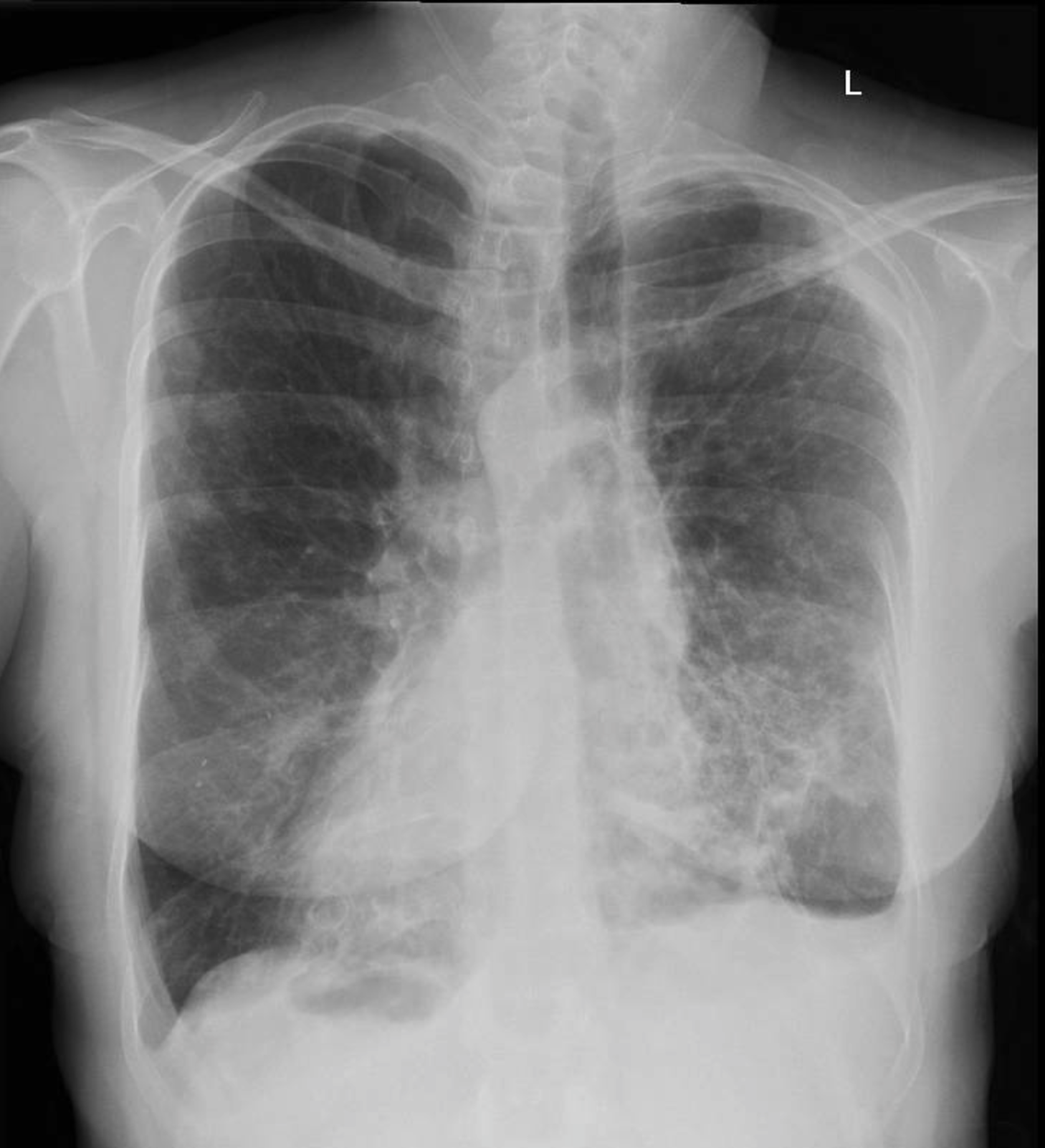
On examination, body temperature is 37 °C, pulse rate is 72/min, respiratory rate is 11/min, BP is 129/76 mm Hg, SpO2 is 97% on room air. The patient is in no respiratory distress, but the chest examination is limited by pain. There are no abnormal breath sounds or adventitious lung sounds, and the examination is otherwise unremarkable. Representative image from chest CT without contrast is shown in Figure 1.
Which is the best next step in caring for this patient?
A. Place a thoracotomy tube urgently.
B. Initiate optimal medical therapy and supportive care.
C. Obtain CT pulmonary angiogram.
D.
Refer to thoracic surgeon for bullectomy.
B. Initiate optimal medical therapy and supportive care.
Placental transmogrification of the lung
A 58-year-old man with COPD is referred to you before an upcoming transcontinental flight. His baseline Spo2 breathing room air is 96%. He endorses dyspnea with minimal exertion but has no symptoms at rest.
On the basis of this information, what should you recommend next for this patient in preparation for his long-haul flight?
A. Hypoxia altitude simulation test
B. In-flight supplemental oxygen not needed
C. Six-min walk test
D. Pulmonary function test
C. Six-min walk test
![]()



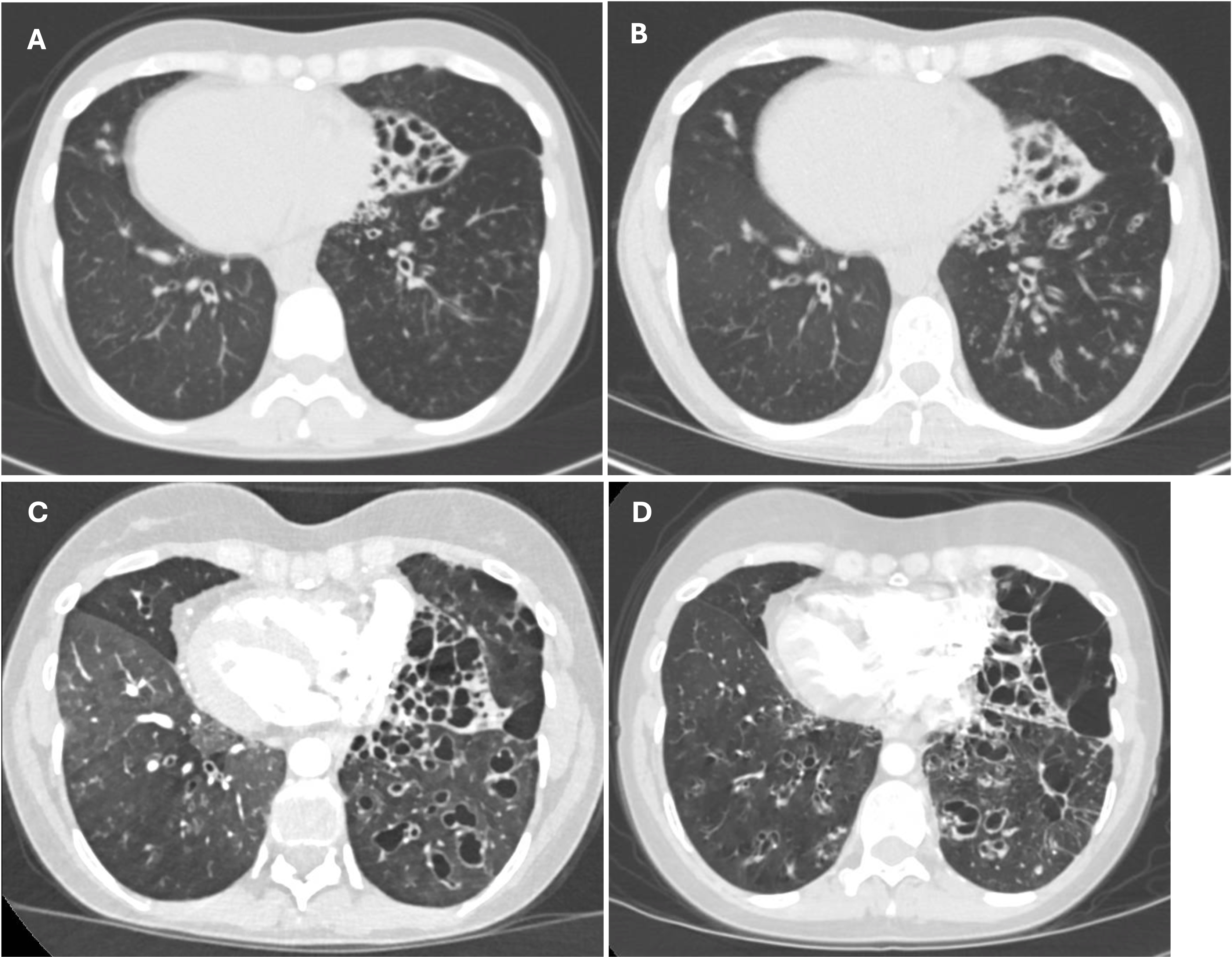
A 41-year-old patient is referred to you for management of bronchiectasis. Bronchiectasis was first diagnosed 12 years ago when she presented with lower respiratory tract infection. Since then, she has had chronic cough productive of yellow-brown sputum and occasional exacerbations. Prior respiratory cultures have grown Staphylococcus aureus. She has had chronic sinusitis for many years (“all my life”) but no other infections. Quantitative immunoglobulin levels have been normal. She is up to date on all indicated vaccinations. Her exercise tolerance is increasingly limited by dyspnea. She has never smoked cigarettes or any other products. She works as a tax accountant. She has not traveled outside the United States in over 2 years. She lives with her husband of 15 years and does not have any children.
Most recent pulmonary function tests show obstructive ventilatory defect with air trapping. Recent chest radiograph is shown in Figure 1. Serial chest CT scans over the past 10 years are shown in Figure 2.
Which of the following is correct about the routine management of the most likely diagnosis?
A. Routine surveillance cultures of expectorated sputum are recommended for all patients.
B. Screening for liver disease with laboratory testing and ultrasound should be done at least every 2 years.
C. Fecal elastase testing should be performed annually.
D. High nasal nitric oxide levels can help to identify exacerbations early.
A. Routine surveillance cultures of expectorated sputum are recommended for all patients.
A 40-year-old truck driver with asthma presents for evaluation of daily symptoms of cough and wheezing. His asthma medications are a high-dose inhaled corticosteroid-formoterol combination inhaler, a long-acting muscarinic antagonist, and prednisone 5 mg daily. Despite good adherence and inhaler technique, he needs to use his combination inhaler two to three times extra most days to relieve symptoms, regardless of the time of year. He has had two exacerbations requiring oral corticosteroids in the past 12 months. He has no other medical problems and does not smoke cigarettes or use recreational drugs. He has not had a change in employment or residence and lives in an urban setting.
Spirometric results show obstruction with reversibility after delivery of a bronchodilator. Fractional exhaled nitric oxide, absolute eosinophil count, and total IgE level are low on several occasions. Radioallergosorbent test results are unrevealing. A chest radiograph demonstrates hyperinflation without airspace opacities.
Which of the following is most likely to lead to improved asthma control?
A. Omalizumab
B. Mepolizumab
C. Benralizumab
D. Dupilumab
D. Dupilumab
A 45-year-old woman with a history of endometriosis presents for evaluation of shortness of breath for the past 4 months. Her symptoms began with an upper respiratory infection that resulted in a dry cough and dyspnea with exertion. She was treated with several courses of oral antibiotics, but her symptoms have persisted. She reports no fever, night sweats, and weight loss. Although she has a history of endometriosis, her symptoms do not correspond with her cycles of menstruation. She reports no history of tobacco or drug use, recent travel, or toxic exposures.
Her physical exam is only notable for diminished breath sounds and mild expiratory wheezing in the anterior left upper lung field. Laboratory analysis is notable for a WBC count of 10,700/µL (10.7 × 109/L), with 8% eosinophils on the differential. The remainder of her laboratory testing, including infectious serologies and cultures, is unremarkable. Spirometry reveals FEV1 is 1.87 L (83% predicted), and FVC is 2.66 L (83% predicted), with an FEV1/FVC of 0.70. An end-expiratory chest radiograph is obtained (Figure 1). This is followed by a chest CT scan with IV contrast (Figure 2). Fluorodeoxyglucose-PET/CT scanning shows no scintigraphic evidence of abnormally increased tracer uptake.
What is the most likely diagnosis?
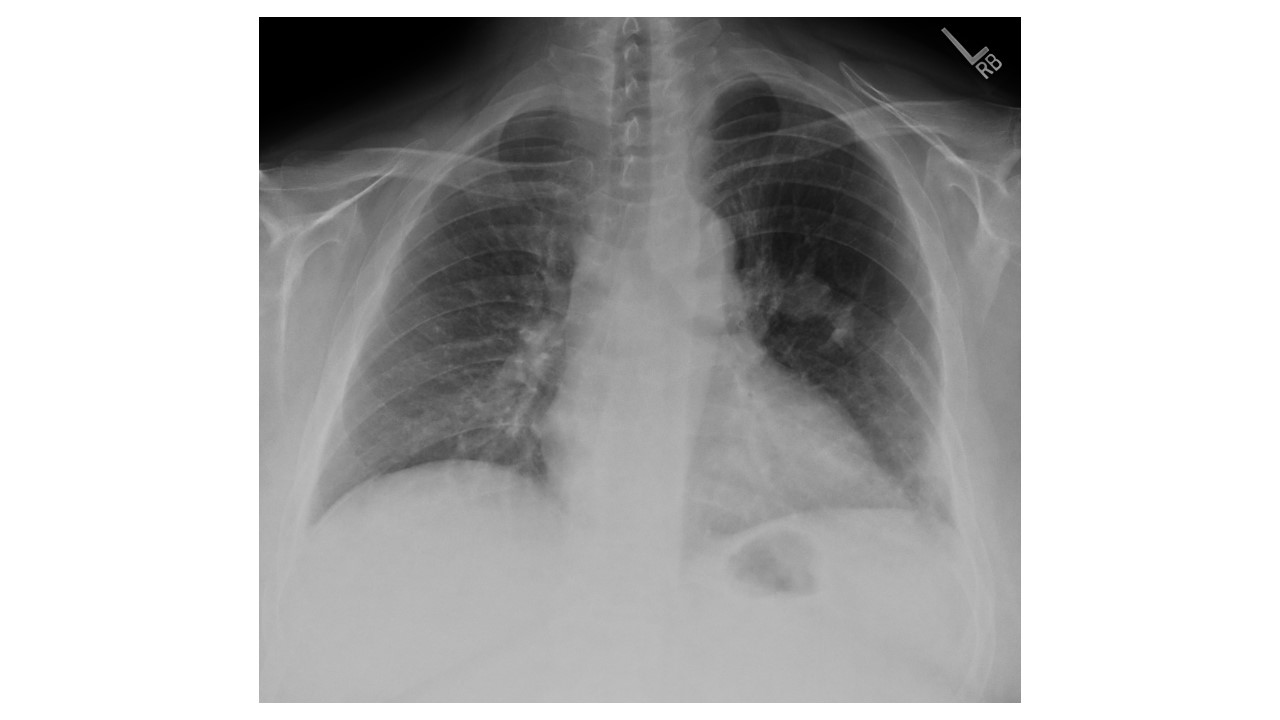
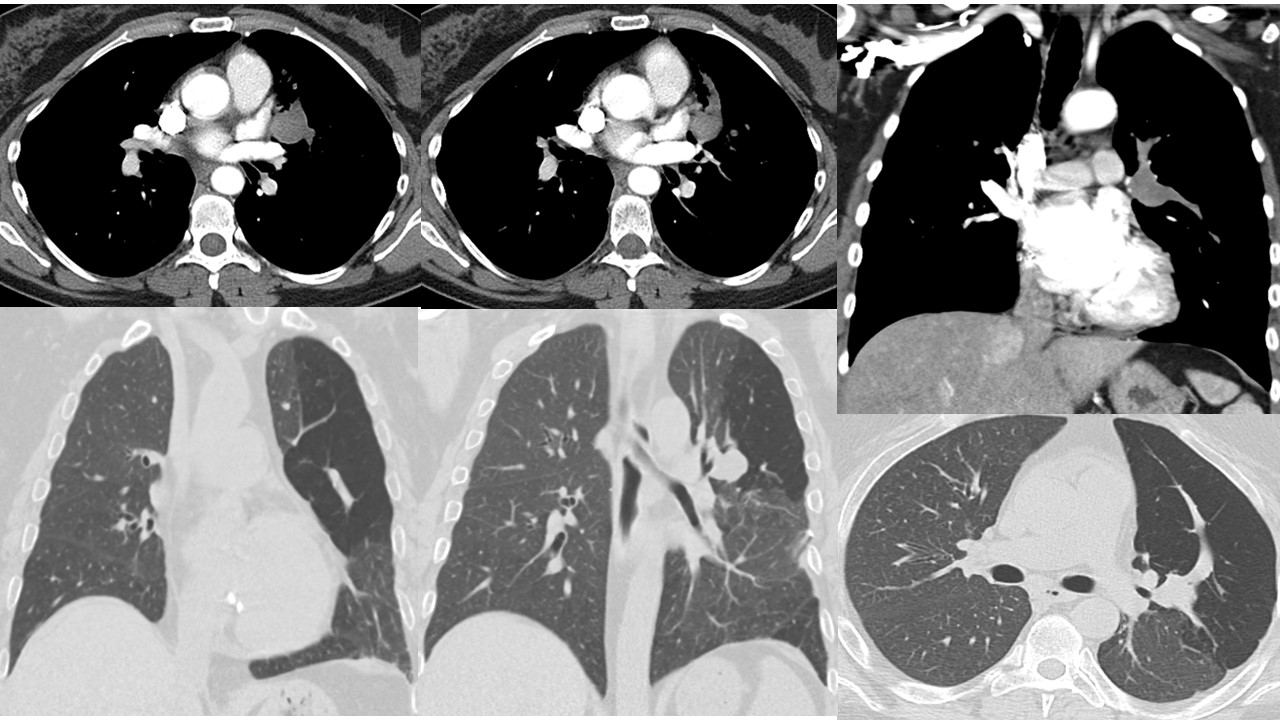
A. Allergic bronchopulmonary aspergillosis
B. Congenital lobar emphysema
C. Arteriovenous malformation
D. Bronchial atresia
D. Bronchial atresia