82-year-old man presents with an inferior ST elevation on ECG and is taken for urgent cardiac catheterization during which a drug-eluting stent is placed in the right coronary artery. During the procedure, he has bradycardia and is given atropine without much improvement. After catheterization, dyspnea and bradycardia persist, and his BP is 85/55 mm Hg.
What is the best next step?
What is "temporary transvenous pacing"
Heart block early after acute inferior MI is usually due to ischemia in the atrioventricular node rather than infarction of the conduction system and, as such, usually resolves within 5 to 7 days. The best therapy for symptomatic bradycardia is insertion of a temporary transvenous pacemaker.
Atropine can block the effects of vagal activity but is not effective for ischemia; the minimal response to atropine in the catheterization laboratory in this case suggests that ischemia is the mechanism and that repeat administration is not likely to be effective
An 81-year-old woman is admitted to the ICU with suspected sepsis after collapsing at a nursing facility. Whole-body, point-of-care ultrasonography is performed with the goal of identifying a source of sepsis or alternative explanations for hemodynamic instability. A high-resolution, linear transducer is used to examine the anterior abdomen.
What finding likely accounts for the ultrasound image obtained?
What is "perforated hollow viscus"
In this case, ultrasonography appears to show a fluid-filled viscus, free peritoneal fluid, then a reverberation artifact typical of intraperitoneal free air. This transition to reverberation artifact is similar to the “lung point” seen with pneumothorax and is termed a “peritoneal point” (or “abdominal point”)
65-year-old woman presented to an outside hospital with a profound right hemiparesis, right facial droop, aphasia, and right hemineglect. She was last seen well at 11 PM the previous evening and was therefore not considered eligible for IV tissue plasminogen activator (tPA). She had a CTH done which did not show any hemorrhagic stroke. She is now transferred to your Joint Commission–certified comprehensive stroke center for further care, arriving at 10 AM.
What is the next appropriate intervention?
What is "obtain CT angiography and perfusion scanning".
This patient is a candidate for interventional thrombectomy if her core infarct is small and she shows evidence of a large vessel occlusion (LVO). This analysis can be accomplished with CT angiography and either CT or MRI perfusion scanning.
In 2018, two trials addressed this issue directly. The DAWN trial and the DEFUSE 3 trial tested patients who present with stroke symptoms between 6 and 24 h, provided there was evidence of a LVO by CT arteriography and evidence of a large perfusion/injury mismatch by either CT perfusion scan or MRI perfusion scan. Intervention produced better functional recovery to independence. NNT of 3!
A 65-year-old woman undergoes a Whipple procedure for an intraductal papillary mucinous neoplasm. She comes to the ICU 1 h after postoperative extubation but with persistent hypotension. On examination in the ICU, her systolic BP is 90 mm Hg and heart rate is 110/min. She is somnolent and tachypneic and has a distended abdomen. You perform intubation quickly and note that on the assist-control volume-control mode of ventilation with a tidal volume of 350 mL, set rate of 12, FiO2 of 0.4, and PEEP of 5 cm H2O, the peak and plateau pressures are both above 40 cm H2O. She has escalating vasopressor requirements and is now anuric. A bladder pressure is obtained after intubation, and the intraabdominal pressure (IAP) is measured at 37 mm Hg.
What is the most appropriate next step in management?
What is "decompressive laparotomy"
Acute abdominal compartment syndrome is a rare but dreaded complication of abdominal surgeries. It occurs in 10% to 30% of patients who are nontraumatically injured and critically ill. IAP is defined by the end-expiratory pressure in the abdomen in the supine position in a fully relaxed patient. Abdominal perfusion pressure is the difference between the mean arterial pressure and IAP. A sustained IAP greater than 12 mm Hg is diagnostic of intraabdominal hypertension. Physiologic consequences of intraabdominal hypertension include clinical signs of impeded venous return, dangerously elevated pulmonary peak and plateau pressures despite full relaxation, and acute onset oliguria. These signs should raise concern about the development of abdominal compartment syndrome.
Abdominal compartment syndrome with intraabdominal hypertension greater than 25 mm Hg on bladder pressure measurement should be treated with decompressive laparotomy
Earlier forms of this medication used for diabetes were found to cause significant lactic acidosis. What is the name of the currently approved biguanide which was approved by the FDA March 3, 1995?
What is "metformin"
The biguanides are derived from the French lilac Galega officinalis, which has been used since the Middle Ages to treat polyuria. Previous biguanides phenformin and buformin were developed in the 1950s but were withdrawn from the market in the 1970s because of a common side effect of lactic acidosis.
Metformin was developed at the same time, and it has been in use in Europe since the 1950s but was not approved for the US market until 1995.
A 79-year-old woman presents with dyspnea, orthopnea, and paroxysmal nocturnal dyspnea. She has a history of hypertension treated with diuretics and calcium channel blockers, paroxysmal atrial fibrillation, carpal tunnel syndrome, and osteoarthritis. On physical examination she has bilateral crackles, a sustained point of maximum impulse, and 3+ bilateral edema. Chest radiography shows cardiomegaly with bilateral pulmonary congestion. CBC count, serum electrolyte levels, glucose levels, and serum protein levels are all normal. Two months prior, she presented to an outpatient office with dyspnea on exertion. An echocardiogram showed left ventricular hypertrophy with low normal systolic performance, and stress testing showed no evidence of myocardial ischemia.
What is the most likely cause of this patient's heart failure?
What is "cardiac amyloidosis"
This patient has clinical hallmarks of cardiac amyloidosis, with a characteristic clinical presentation, physical examination with biventricular heart failure, and echocardiogram. Previous carpal tunnel syndrome is another clue.
Cardiac amyloidosis is increasingly recognized as a cause of heart failure and also atrial fibrillation, as accumulation of amyloid within the heart increases diastolic stiffness, raises intracardiac diastolic pressures, and leads to increased atrial size. Cardiac involvement is usually due to either AL or ATTR amyloidosis. Clinical features that raise the suspicion for the diagnosis include manifestations of restrictive cardiomyopathy with signs of right heart failure, such as JVD, hepatomegaly, and lower extremity edema, and signs and symptoms of left heart failure.
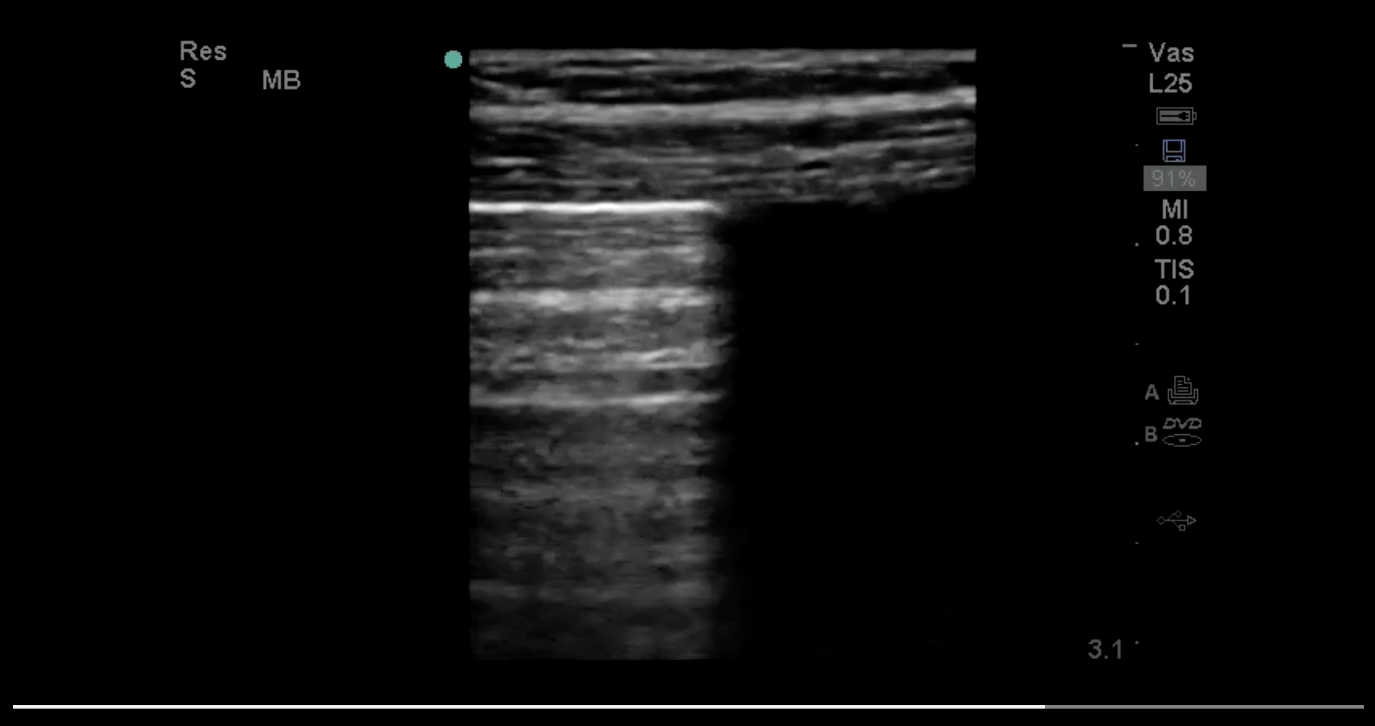
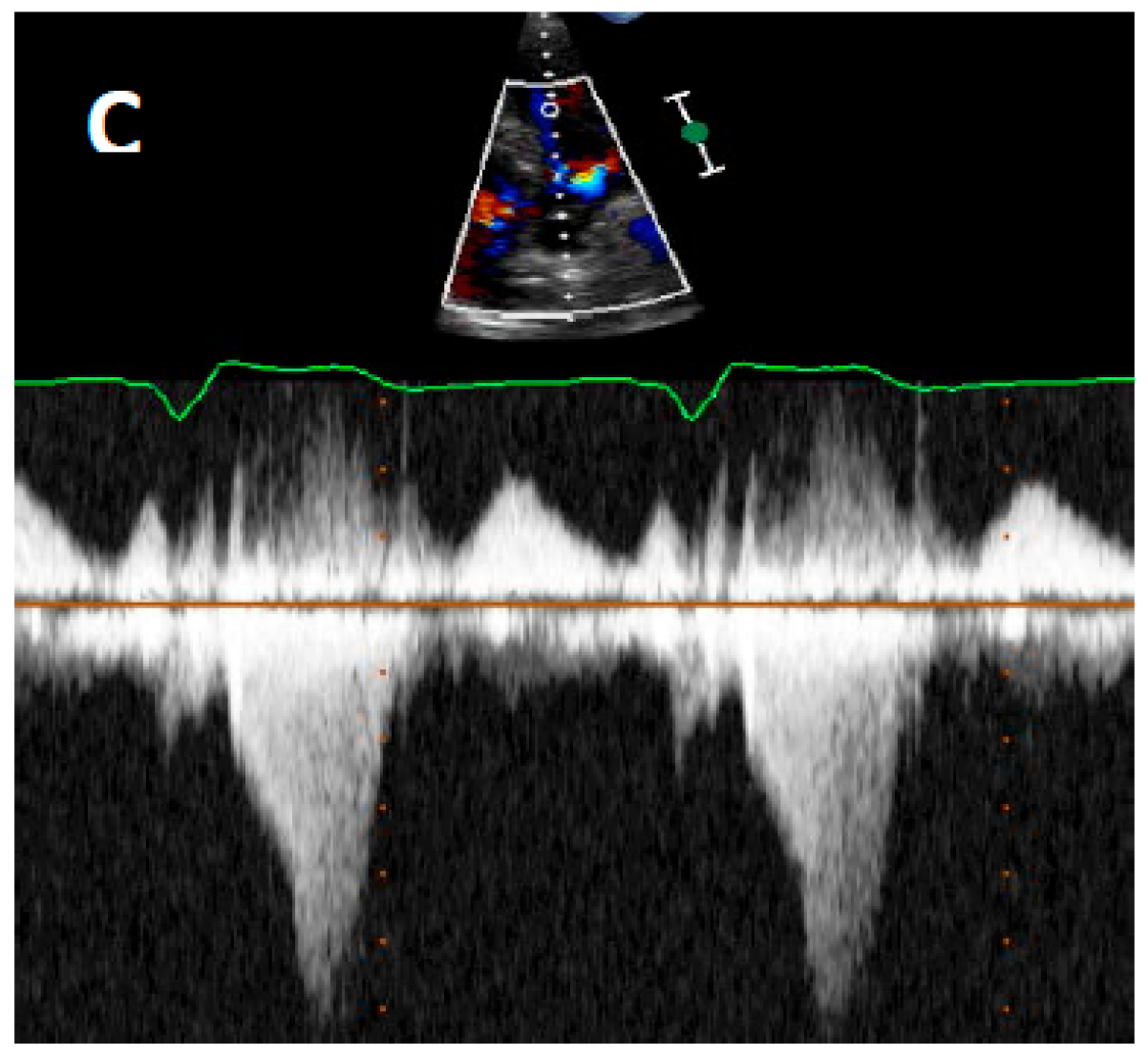
What is the name of the ultrasound finding featured in this video and what does it describe?
What is "lung pulse which describes atelectasis"
In a study, this finding has 93% sensitivity and 100% specificity for apnea or lack of ventilation of the visualized lung. It also indicates that the parietal and visceral pleura are in contact.
Lung pulse is the term used to describe pulsation of the lung due to the mechanical movement of the heart that is appreciable at the pleural surface via ultrasonography. The rate of lung pulse corresponds to heart rate. For lung pulse to be present, three conditions are necessary: absence of lung sliding; contact between the two surfaces of the pleura; and apnea of the visualized part of the lung.
A 62-year-old woman presents with sudden onset of left-sided weakness and slurred speech. She has a history of diabetes, hypertension, and hyperlipidemia and had been admitted to another hospital a month prior with a myocardial infarction, after which she stopped smoking. She is afebrile with a BP of 156/92 and a heart rate of 64/min. Physical exam is notable for clear lungs, no murmurs, trace edema, and a facial droop with weakness of the left upper and lower extremities. Her ECG is shown in Figure 1. Head CT shows a subacute, left occipital infarct and a new, right frontal infarct with hemorrhagic conversion.

What diagnostic test is most likely to determine the etiology of her stroke?
What is "TTE"
The key to this case is the recognition that the patient presented with an acute stroke but had evidence of strokes in two different arterial territories. In this setting, a cardioembolic etiology should be suspected.
The patient's history of recent myocardial infarction along with poor R wave progression on the ECG suggests the possibility of an anterior infarction with an apical thrombus. This can be diagnosed with transthoracic echocardiography. TTE can also detect valvular lesions with embolic potential and look for a patent foramen ovale as a potential substrate for paradoxical emboli.
Event monitoring to detect paroxysmal atrial fibrillation is warranted in cryptogenic stroke, but cardioembolic sources and large artery atherosclerosis need to be ruled out before deeming a stroke cryptogenic.
A 65-year-old woman with a history of rheumatoid arthritis had a radical hysterectomy for endometrial carcinoma. Her estimated blood loss during the procedure was 500 mL for which she received 2.5 L of lactated Ringer's solution via a left subclavian venous catheter. The next morning, she is a little dyspneic and in pain but is otherwise doing OK. Both her subclavian catheter and her nasogastric tube are removed per protocol. Later in the afternoon, she becomes progressively more short of breath and is transferred to the ICU. On arrival, her vital signs are as follows: BP, 120/85 mm Hg; heart rate, 110/min; respiration, 35/min; temperature, 36.2°C; and urine output, 0.2 mL/kg/h. A CXR reveals a left sided pleural effusion. She undergoes a thoracentesis.

What additional tests would indicate the appropriate diagnosis?
What is a "pleural fluid creatinine and serum creatinine"
There are only a handful of conditions that typically cause transudative pleural effusions. Less common conditions include iatrogenic infusion of crystalloids into the pleural or peritoneal space and urinothorax. Nephrostomy tube placement, pelvic trauma, and surgery in the pelvis or retroperitoneum can occasionally be complicated by injury to the renal calyces, ureters, or bladder. When this occurs, urine can flow into the peritoneal or retroperitoneal spaces and find its way into the lower pressure pleural space. The majority of such patients, like the patient in this case, are oliguric. The pleural fluid characteristics depend not only on the characteristics of the urine leaking into the pleural space but also on the effects of local tissue trauma. Although urinothoraces are classically transudates, they may be exudative in up to 40% of cases. Also, urinothoraces may be bloody, neutrophilic or lymphocytic, and have low or high pH and glucose. Therefore, the only characteristic that reliably differentiates a urinothorax from other causes of pleural effusion is the ratio of pleural fluid to serum creatinine of >1
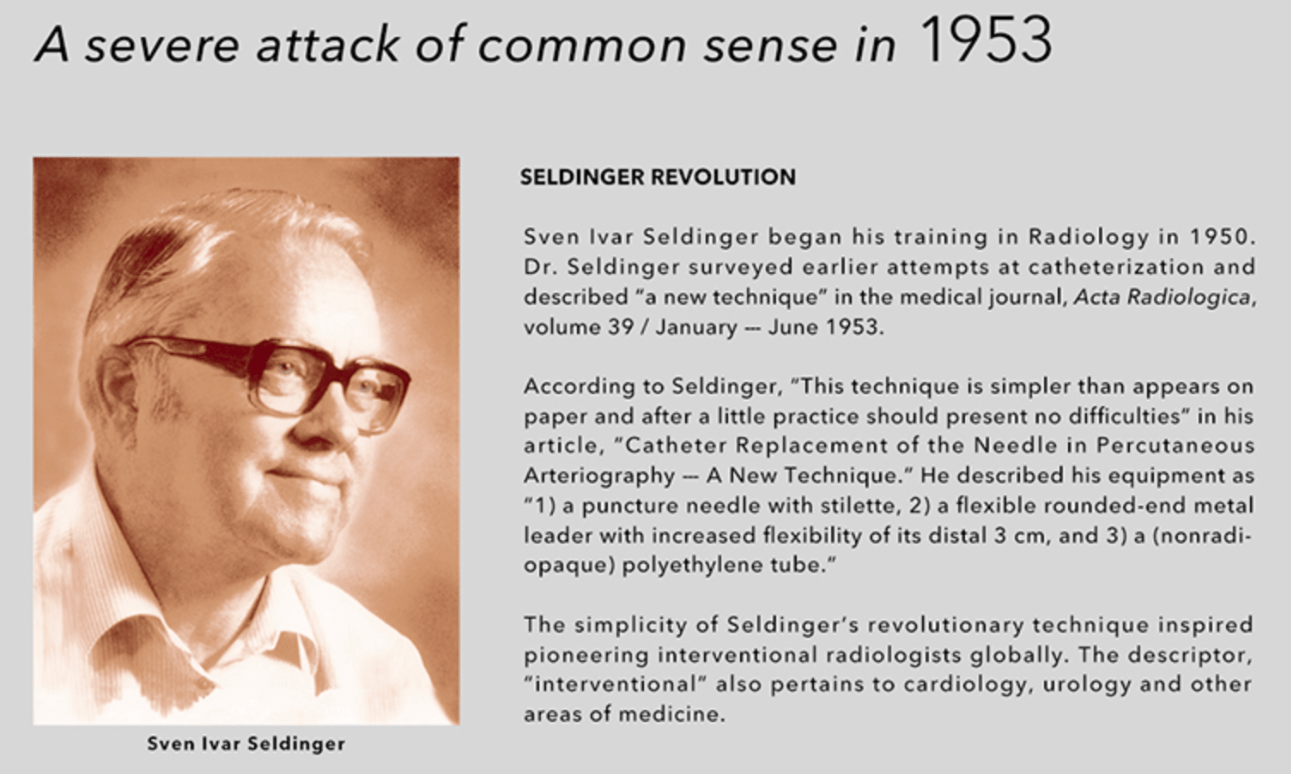
In June of 1953 this Swedish born radiologist described a novel technique for vascular access. The equipment required was described as 1) puncture needle with stilette 2) flexible rounded end metal leader with increased flexibility of its distal 3 cm 3) a (non radiopaque) polyethylene tube.
What is the name of the technique?
What is "Seldinger technique"
A 64 YOF had a DES placed for NSTEMI. The next morning, she presents with tachycardia and shortness of breath and is noted to be in atrial fibrillation with a rate between 110-130/min. She is taken back to the catheterization laboratory, where the stent is shown to be patent.
Following the repeat catheterization, she is agitated and confused. Her BP is 100/75 mm Hg, heart rate is 150-160/min, respirations are 36/min, and temperature is 39.6°C. She has bilateral crackles on lung exam, with a rapid irregular heart rhythm with an S3 gallop. The abdomen is mildly tender, and there is bilateral pedal edema.
Which of the following is most likely to produce clinical improvement now and WHY?
A. Saline Bolus
B. IV propanolol
C. IV Amiodarone
D. IV Diltiazem
What is "IV propanolol"
The patient developed fever, altered mental status, rapid atrial fibrillation, and heart failure after coronary angiography, a constellation of findings that should suggest the possibility of thyroid storm,
Thyroid storm in a patient with subclinical hyperthyroidism can be precipitated by administration of iodinated contrast material (Jod-Basedow syndrome), as it was in this case. The pathophysiology of thyroid storm probably results from a combination of effects of thyroid hormone and sympathetic activation. As such, tachycardia is usually treated with nonselective β-blockers. In the setting of heart failure, β-blockers should be given with some caution, but rate control often increases BP and improves cardiac output in this setting. Propranolol is the classic β-blocker employed in thyroid storm because, in addition to inhibiting the peripheral effects of hyperthyroidism, it also inhibits conversion of thyroxine (T4) to triiodothyronine (T3), but esmolol is an alternative,
The patient was mildly hypotensive with a low pulse pressure, but fluid administration is not helpful in the presence of frank heart failure (choice A is incorrect). Diltiazem can slow heart rate but has negative inotropic effects and does not address the underlying hypersympathetic state (choice D is incorrect). Amiodarone contains iodine and is contraindicated in patients with thyroid disease (choice C is incorrect)
78-year-old woman is admitted with septic shock. Goal-directed echocardiography shows this parasternal long-axis. What is the structure identified by the "X"?
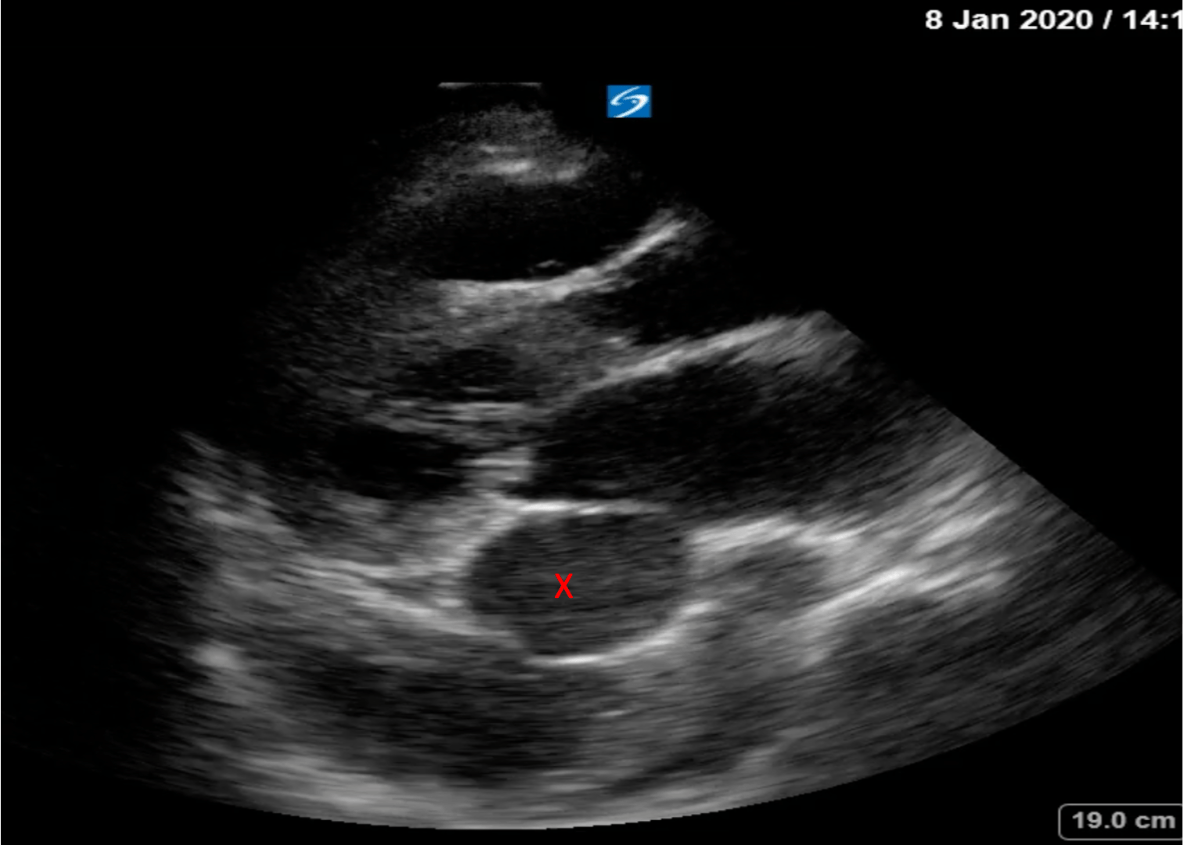
What is "enlarged coronary sinus"

An enlarged coronary sinus should always raise suspicion for a left-sided superior vena cava (SVC), seen in roughly 0.5% of the population. The CS also enlarges due to elevated right atrial pressures, partial anomalous pulmonary venous return to the CS, and coronary arteriovenous fistula or when it abnormally receives a hepatic vein. An enlarged CS is usually asymptomatic and discovered incidentally during echocardiographic imaging, device implantation, or surgery.
A 29-year-old man is involved in a high-impact motor vehicle crash during which he sustains significant trauma to his head, chest, abdomen, and pelvis. He is taken to a level I trauma center, where on examination he has a Glasgow Coma Scale score of 9, BP of 72/38 mm Hg, and pulse of 46/min. Assessment by physical examination is difficult related to his markedly altered level of consciousness.
Based on this clinical presentation, what is the expected pathology and WHY?
What is a "cervical spine fracture"
Acute injury to the cervical spinal cord is frequently accompanied by specific cardiovascular abnormalities and can lead to neurogenic shock. The neuroanatomy important in understanding this is that the CNS’s regulation of the sympathetic nervous system lies within pathways in the lateral brain stem, cervical cord, and upper segments of the thoracic cord (above T6). Consequently, injuries to the spinal cord above T6 will compromise descending control of preganglionic cardiac sympathetic pathways. This results in reduced sympathetic tone which leads to relative vagal parasympathetic predominance.
The corresponding cardiovascular signs are hypotension (due to elimination of sympathetic arteriolar tone) and bradycardia (as a result of disrupted cardiac sympathetic influences and unopposed vagal input).
A 55-year-old woman presented to the emergency department with a fever, nausea, and abdominal pain. A CT scan of the abdomen demonstrated a dilated gall bladder and a dilated bile duct with a concern for obstructing stones, so the patient started piperacillin-tazobactam and underwent emergency endoscopic retrograde cholangiopancreatography (ERCP) in the operating room.
The patient underwent intubation for the procedure with use of etomidate and succinylcholine and received propofol during the ERCP. After the ERCP, the patient underwent extubation without difficulty and remained hemodynamically stable but with a persistently elevated temperature, now up to 40.2 °C in the postanesthesia care unit. Because of the elevated temperature, the patient received additional IV fluids and an acetaminophen suppository, and she was transferred to the ICU for observation.
When the patient arrived in the ICU, she was confused, minimally responsive, and had spasms of her face and jaw, and she had a heart rate of 115/min, respiratory rate of 24/min, BP of 110/50 mm Hg, SpO2 of 94% with 4 L of oxygen via nasal cannula, and a temperature of 41.5 °C. Arterial blood gas measurements were a pH of 7.21, PCO2 of 53 mm Hg, PO2 of 80 mm Hg, and HCO3 of 18 mEq/L (18 mmol/L). The patient is administered an additional liter of fluid, and external cooling measures are initiated.
What is the most important next step in management of this patient?
What is administer IV dantrolene for malignant hyperthermia
Malignant hyperthermia (MH) should be suspected in this patient because of the rapidly increasing temperatures associated with muscle rigidity of the face and jaw (trismus) after receiving succinylcholine (a depolarizing muscle relaxant).
MH is a rare (1:10,000 and 1:250,000) autosomal dominant disorder that is life-threatening and is caused by exposure to volatile anesthetic agents and depolarizing muscle relaxants (such as succinylcholine).
Patients with MH develop unexplained temperature increases, tachycardia, increases in end-tidal carbon dioxide, increases in minute ventilation, and muscle rigidity. Patients can also develop acidosis, hyperkalemia, and rhabdomyolysis owing to uncontrolled hypermetabolism. Once MH is suspected, steps should be taken immediately to reverse the reaction. These steps include the removal of the offending agent, external cooling measures, and IV dantrolene
In 1990 a 2 year old Danish girl with croup was sedated with this medication for 4 days and ultimately developed metabolic acidosis, heart failure, hypotension, and hepatomegaly.
What is the medication and what is the syndrome described above?
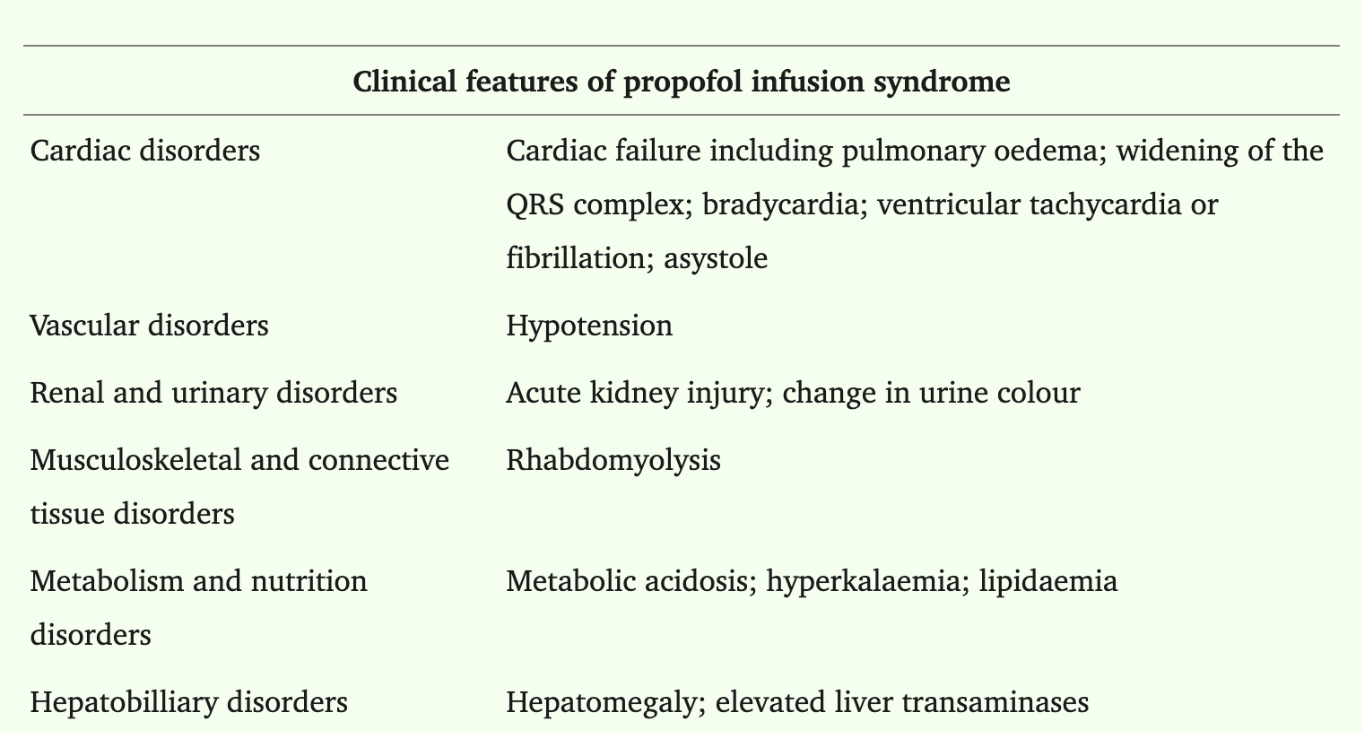
What is Propofol and Propofol Infusion Syndrome or PRIS
This is the first case of PRIS described in the literature. This patient received 10mg/kg/hr of propofol for 4 days and ultimately died. The first adult patient died from PRIS in 1998.
DAILY DOUBLE
Vital signs include a temperature of 37°C, HR 180/min, BP of 111/72 mm Hg, and RR of 22/min. A 12-lead ECG (Figure 1) and six-lead rhythm strip (Figure 2) are obtained.

What is the arrhythmia and what is the best treatment for it?
what is "atrial fibrillation with pre-existing WPW, best treatment is with ibutilide and procainamide
Inspection shows that the tachyarrhythmia is irregularly irregular. Furthermore, the widths of the QRS are also irregular and vary between beats (best seen in the six-lead rhythm strip or lead V4 of the 12-lead ECG). These three criteria, namely wide complex tachyarrhythmia, irregularly irregular rhythm, and varying widths of the QRS complexes, should prompt consideration of preexcited atrial fibrillation or atrial fibrillation in a patient with an accessory conduction pathway.
Patients with preexcitation syndrome have an accessory conduction pathway that directly connects the atria with the ventricles and bypasses the atrioventricular (AV) node. If conduction occurs through this accessory pathway, the ventricles are activated sooner than when the impulse travels through the AV node. This activation, which is referred to as preexcitation, results in the classic ECG findings of shortened PR interval and widened QRS complex due to a delta wave.
 The goal of medical treatment is to both slow conduction through the accessory pathway and convert the atrial fibrillation or flutter back to sinus rhythm. Preferred agents include ibutilide and procainamide
The goal of medical treatment is to both slow conduction through the accessory pathway and convert the atrial fibrillation or flutter back to sinus rhythm. Preferred agents include ibutilide and procainamide
Blocking the AV node risks increasing conduction of atrial impulses to the ventricle through the accessory pathway, resulting in an increased ventricular rate and potentially exacerbating hemodynamic instability. Adenosine selectively blocks the AV nodal pathway and may precipitate ventricular fibrillation. Although amiodarone may slow conduction through the accessory pathway with chronic administration, it does not slow accessory pathway conduction with acute IV administration, and its β-blocking properties make it a primarily AV nodal-blocking agent in the acute setting, making it a nonpreferred agent in preexcited atrial fibrillation.
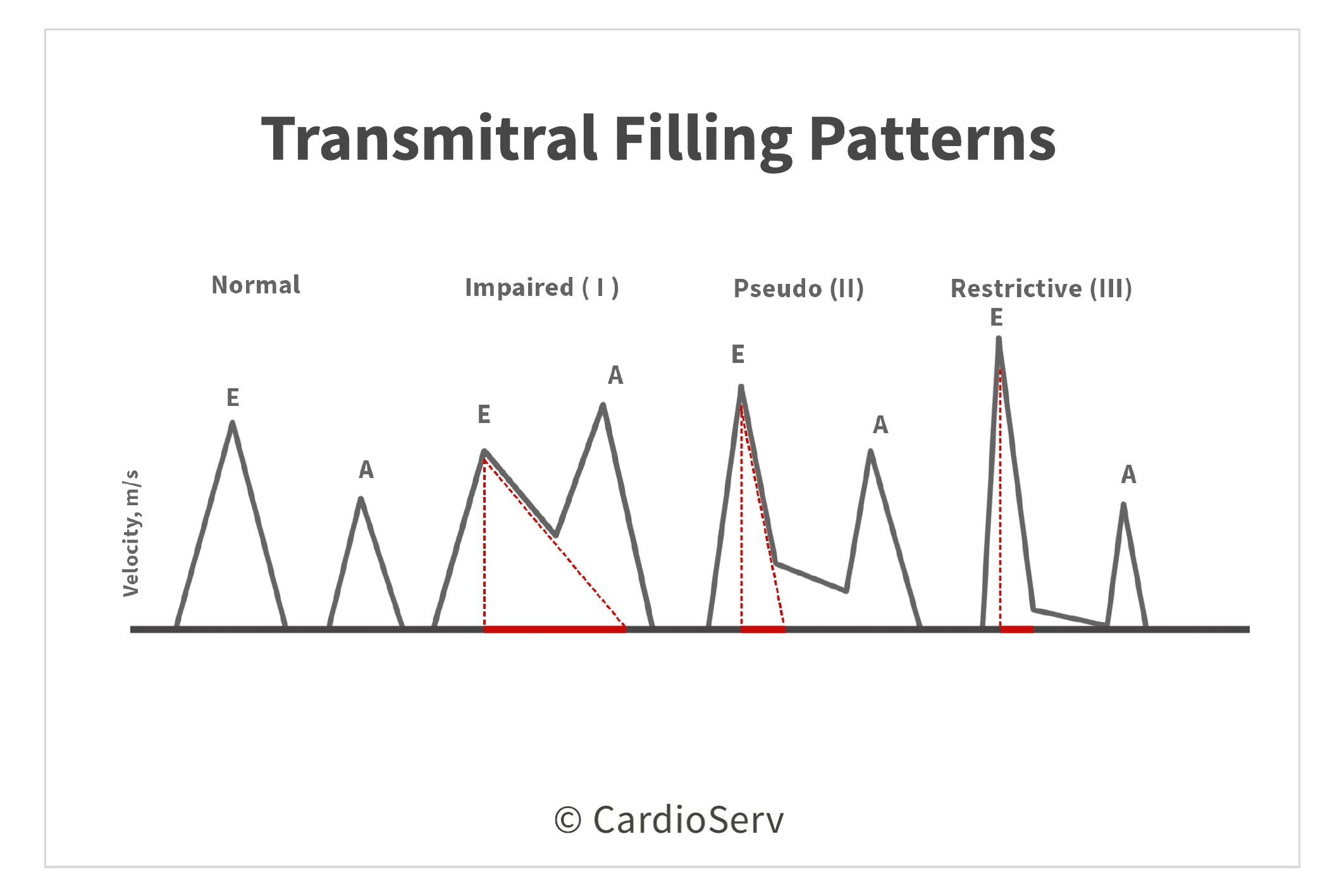
Transthoracic echocardiography is performed with the apical four-chamber view shown (Figure 1) using pulse wave Doppler. Flow shown at the arrow represents which one of the following?

What is "early diastolic transmitral flow"
The initial wave (E wave) represents early transmitral flow velocities that follow mitral valve opening consequent to the fall in left ventricular pressure as the ventricle relaxes (diastole). The second wave (A wave) shows transmitral flow related to atrial contraction. Flow velocities, the relationship of E and A velocities, and acceleration and deceleration times provide information about diastolic function.
A 60-year-old woman presents with the acute onset of headache. The initial CT scan is shown (Figure 1). An external ventricular drain (EVD) is placed. Which intervention has been shown to decrease the risk of mortality?

A. Manage EVD clamped with removal of 10cc of CSF every hour.
B. Manage EVD set above the tragus of the ear with passive drainage at high intraventricular pressure
C. Administer intrathecal tPA until 85% reduction in intraventricular blood is achieved
D. Remove the EVD 1 day after insertion to prevent infection
What is "administer intrathecal tPA"
In fact, there has been no randomized clinical trial to compare the two most common paradigms of EVD management: closed-drain vs open-drain management. In the closed-drain model, the catheter stopcock is closed to the outside drainage bag (this allows sensing intracerebral pressure in the closed system). When the pressure increases (or at a prespecified interval), fluid is drained from the EVD. In the open-drain model, the outlet of the EVD is set at a specific height above the tragus of the ear, and fluid is drained when the pressure in the cerebral ventricles exceeds the back pressure derived from gravity from the elevation of the catheter outlet.
The most recent development in the treatment of IVH has been the administration of tPA into the cerebrospinal fluid to aid in the dissolution of blood clots, allowing for drainage of unclotted blood from the ventricles. Interestingly, multiple studies have shown improved mortality with the use of tPA. CLEAR III, shows that in the group of patients with >20 mL of intraventricular blood in whom 85% of the blood can be cleared from the ventricular space, functional outcome is also improved.
You are called to a rapid response in the day surgery clinic to evaluate a 66-year-old man undergoing elective knee arthroplasty surgery under general anesthesia with adjunctive regional peripheral nerve blockade. The patient has a history of type 2 diabetes well controlled with metformin, and mild renal insufficiency secondary to diabetic nephropathy. He is a former tobacco user. There is no history of alcohol use. He has no known allergies.
The arthroscopic procedure had just started with induction and administration of bupivacaine for peripheral nerve blockade and was followed by a single tonic-clonic seizure 5 min later and subsequent hypotension partially responsive to fluid administration.
On examination, BP is 80/48 mm Hg, pulse is 120/min, respirations are 24/min, and pulse Spo2 is 94% with 0.4 FiO2 via laryngeal mask airway. There is no cyanosis. There is no stridor. Lungs are clear without wheezing, and cardiac examination reveals tachycardia. Point-of-care glucose is 122 mg/dL (6.77 mmol/L).
What is the diagnosis and what is the recommended treatment?
What is "local anesthetic systemic toxicity and the treatment is lipid emulsion"
LAST is a rare but well described complication of LA treatment, and in composite studies, from retrospective reviews of registries, the incidence is estimated at 0.27 episodes per 1,000 peripheral nerve blocks (0.03%). The outcome can be fatal. The initial treatment of choice includes lipid emulsion. bupivacaine is the riskiest choice but LAST has been described with lidocaine.
LAST is primarily due to inadvertent intravascular injection and systemic absorption of LA. Clinically, findings of LAST usually develop immediately to within 15 min after injection, although delayed LAST can occur in the setting of longer-acting administered agents and in individuals with low body mass. The primary findings in LAST include neurologic and cardiac effects. Neurologic effects are the most common and can be mild, such as oral numbness, tinnitus, or a metallic taste, and can progress to anxiety, agitation, dysarthria, mental status changes, audiovisual changes, twitching, somnolence, seizures, loss of consciousness, coma, and respiratory arrest. Seizures are one of the most common presenting features and develop in 53% to 77% of those with LAST. Cardiovascular findings can include mild or profound hypotension; hypertension; tachycardia or bradycardia; ventricular arrhythmias; asystole; and, in extreme cases, cardiac arrest.
One-third of cases begin with neurologic findings and progress to cardiovascular, but about one-fifth of cases have only cardiovascular involvement.
September 12, 1957 Dr. E. Donnall Thomas described the first instance of a "successful" hematologic procedure wherein patients were treated with chemotherapy and radiation prior the procedure, 2 patients had some short term success, and at the 100 day mark all 6 patients died.
What was the procedure?
What is "allogeneic hematopoietic stem cell transplant"
Only two patients engrafted, and all died by 100 days post the transplantation. At that time, little was known about histocompatibility antigens, and no one tried to match donors and recipients.
As an aside, I skimmed this paper and the bone marrow was obtained from dead patients or from rib resections of patients undergoing other procedures! For example, a patient who had a "The donor marrow was obtained from a rib removed at thoracotomy."
45 YOF with Flu A ARDS is on VV-ECMO via a RIJ dual-lumen catheter with 3.5 L/min of blood flow, 3 L/min of sweep gas flow, and 100% FdO2. She has been improving on minimal vent settings. Her HR is 94/min, and BP is 105/60 mm Hg. Pulse oximetry (left index finger) is 93%. She is awake and interactive and resting comfortably in bed, breathing at a rate of 15/min. One hour after returning from CT scanning, she develops acute hypoxemia with SpO2 of 62%. Heart rate is 145/min, and BP is 155/90 mm Hg. Respiratory rate is 32/min, and she appears distressed.
Arterial blood gas analysis shows a pH of 7.22, PCO2 of 35 mm Hg, and PO2 of 47 mm Hg. Arterial lactate is 6.8 (0.5-2.0) mg/dL (0.75 [0.06-0.22] mmol/L). The blood in the drainage and return circuits of the ECMO machine appears dark red. A preoxygenator (P1) blood gas shows a pH of 7.12, PCO2 of 44 mm Hg, and PO2 of 32 mm Hg, while that after the oxygenator shows a pH of 7.15, PCO2 of 42 mm Hg, and PO2 of 35 mm Hg. Figure 1 shows the P1 and postoxygenator (P2) pressures in the ECMO circuit.
What action should be taken at this point to alleviate the patient’s hypoxemia?

What is "change oxygen source for the oxygenator"
The patient does not have any increase in oxygenation across the oxygenator (ie, P1 and P2 PO2 values are almost identical). Two potential causes of this are poor functioning of the oxygenator (usually due to clot formation on the oxygenator surface) or inadequate oxygen supply to the oxygenator.
The relatively normal difference between the P1 and P2 pressures (20 mm Hg pressure difference) (Figure 1) suggests that the oxygenator is functioning appropriately and is not burdened with significant clot or P2 obstruction. A pressure gradient of 70 mm Hg or more has been cited as a threshold that should prompt oxygenator exchange. Additionally, even with a failing oxygenator, some oxygen transfer should persist.
Recirculation describes a large proportion of the oxygenated blood from the return cannula being drawn again into the ECMO circuit (via the drainage cannula), without being circulated throughout the body. The patient may become hypoxemic because of receiving little oxygenated blood from the ECMO. This can occur with high blood flows through the ECMO circuit or when the drainage and return cannulas are too close together in femorojugular venovenous configurations. It is less common when dual-lumen cannulas are used. When recirculation occurs, the blood in the P1 limb of the ECMO circuit has high PO2 levels, which are only slightly below those in the P2 limb of the ECMO circuit. This is not the case in this patient who has low PO2 values in both P1 and P2 limbs of the ECMO circuit.
Systemic oxygenation of patients on VV ECMO is a confluence of blood returning from the ECMO circuit and venous blood returning from the body and is directly related to the ratio of ECMO flow to cardiac output. Increasing the blood flow through the ECMO circuit will provide a larger volume of oxygenated blood to mix with the deoxygenated venous blood and should raise systemic oxygenation. However, in this patient, the oxygenator is not providing oxygenated blood due to a poor oxygen source. Increasing the blood flow in this scenario will not improve systemic oxygenation and may even worsen the patient’s hypoxemia
A 64-year-old woman with a history of hypertension and diabetes is admitted with flank pain, fever, and shock. Imaging reveals a renal stone at the right ureteropelvic junction with associated hydronephrosis. Urgent percutaneous nephrostomy is planned once initial stabilization is achieved. She is intubated, ventilated, and sedated. Vital signs include a heart rate of 128/min, BP of 94/70 mm Hg, respiratory rate of 32/min (controlled), and temperature of 38.8°C. Point-of-care echocardiography yields this parasternal long-axis view

Based on this information, what is the likely cardiac abnormality and what would be the recommended therapy?
What is "intraventricular outflow tract obstruction and fluids should be given aggressively for hypotension. If vasopressors required, phenylephrine or vasopressin preferred"
Early septic shock is often characterized by hypovolemia, reduced left ventricular afterload, and increased inotropy, conditions that favor intraventricular flow obstruction (IVO). Left ventricular hypertrophy may contribute, especially in patients with hypertrophic obstructive cardiomyopathy (HOCM), but IVO is seen in roughly 20% of all patients in early sepsis. Dynamic obstruction is usually localized to the left ventricular outflow tract (LVOT) and due to systolic anterior motion of the mitral valve as flow acceleration tends to draw the anterior leaflet into the LVOT (Bernoulli effect)

27-year-old man with a history of two previous motor vehicle crashes due to alcohol intoxication is an unrestrained driver in a single-vehicle collision with a road barrier that ejected him from the car. In the field, he is unconscious with a Glasgow Coma Scale score of 4 and undergoes intubation. In the ED, a CT scan of the head shows a large right frontal contusion and anterior temporal contusions in both hemispheres. The frontal horns of his lateral ventricle are compressed. Because of his low GCS score and focal lesions, he has an intracranial pressure monitor placed for management of increased intracranial pressure. His intracranial pressure on placement is 40 mm Hg. His heart rate is 90/min, and his BP is 180/80 mm Hg (mean arterial pressure, 113 mm Hg).
What is the best intervention to improve the patient's outcome?
What is "lower ICP through IV mannitol or 23.4% hypertonic saline"
ICP values >20 mm Hg have consistently shown worse outcome. The calculated value for perfusion to the brain is called the cerebral perfusion pressure (CPP), which is calculated as mean arterial pressure (MAP) minus ICP.
Lowering CPP to below 70 mm Hg in patients who achieve these values without augmentation has not been tested and may have consequences in peri-contusion ischemic tissue. The Traumatic Brain Injury Guidelines suggest “avoiding aggressive attempts to maintain CPP above 70 mm Hg with fluids and pressors may be considered because of the risk of adult respiratory failure”
An external ventricular drain (EVD) is the preferred method of lowering ICP in patients with traumatic brain injury when it can be achieved safely. In this patient, the frontal horns of the lateral ventricles are compressed; EVD placement carries a high risk of failure and injury
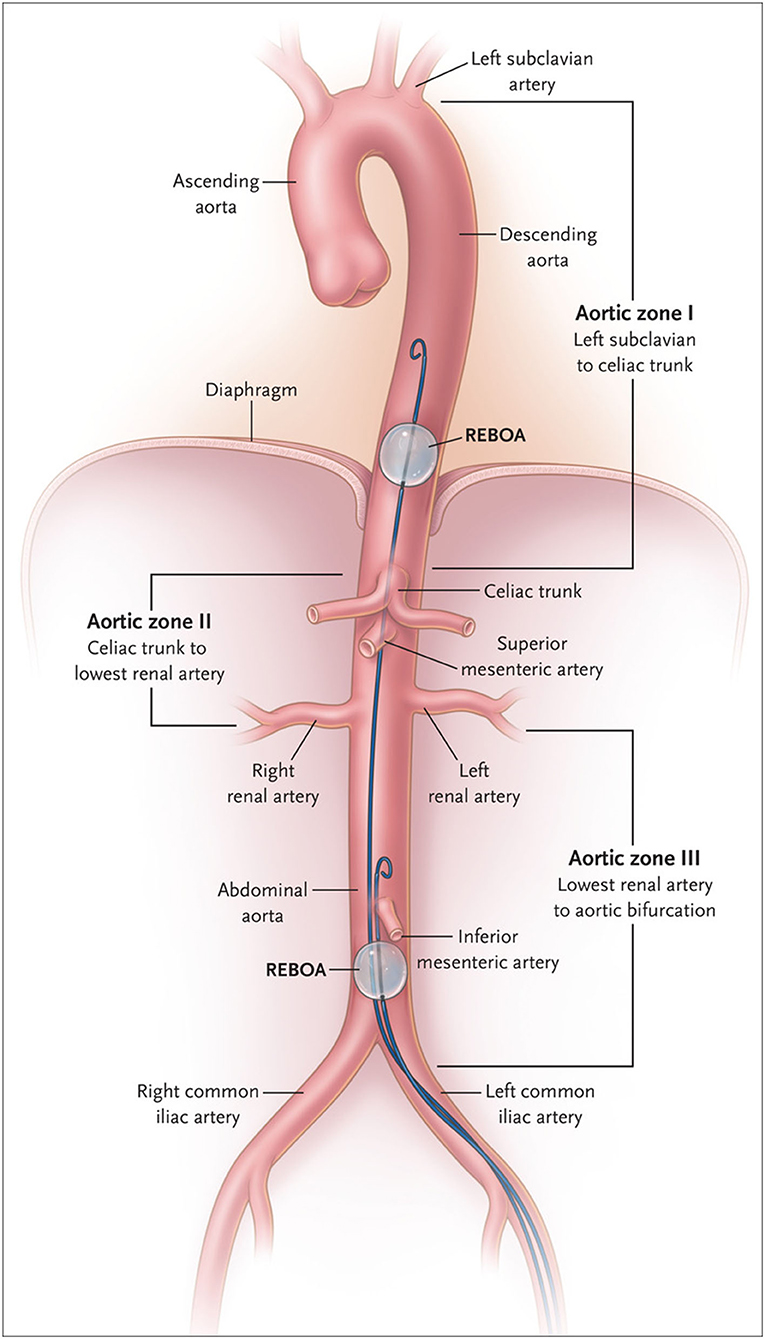
A 25-year-old man is brought to the emergency department after being struck by an automobile while riding his bicycle. He has severe torso trauma with bleeding and has abject shock despite use of blood products according to the local massive transfusion protocol by the treating team. Heart ultrasonography shows no evidence of pericardial effusion. Bilateral tube thoracostomy has been performed, with ongoing bleeding from both chest tubes. The focused assessment with sonography in trauma (FAST) examination is positive, suggesting intraperitoneal hemorrhage. The team is preparing to perform resuscitative endovascular balloon occlusion of the aorta (REBOA).
On the basis of best evidence, what can be said about this planned action?
What is "REBOA is associated with increased mortality due to bleeding"
Aortic occlusion with a peripherally inserted catheter has been proposed to limit flow of blood to the pelvis and distal extremities temporarily, to allow time to accomplish definitive hemostasis. REBOA was proposed to accomplish this task. However, the UK-REBOA trial randomly assigned 90 patients with exsanguinating hemorrhage due to torso trauma to REBOA or standard care. Contrary to expectations, REBOA did not improve survival or other important end points, and, notably, it led to an increase in mortality due to bleeding (32% vs 17%)
In 1930, three physicians described a bundle-branch block with short P-R interval in healthy young people prone to paroxysmal tachycardia.
What is the tachycardia and draw it out.
What is "Wolf Parkinson White"
