Describe nursing considerations for iron deficiency anemia
NURSING CONSIDERATIONS:
•Discuss side effects of oral iron supplements (staining teeth, poor taste, constipation) but educate on the importance of compliance
*Iron supplements should be taken on an empty stomach
Describe clinical manifestations and diagnostic studies for Hodgkin’s Lymphoma
-Clinical Manifestions:
•“B Symptoms”: Fever, weight loss (unintentional, > 10% of body weight), drenching night sweats
•Painless enlarged lymph nodes
•May have presents of mediastinal mass which may cause cough
-Diagnostic Studies:
•Hallmark: presence of Reed-Sternberg cells on CBC
•Imaging: CT, MRI, PET of are of concern
•Nodular biopsy
● Describe what results would be seen on the newborn screening for a
newborn with congenital hypothyroidism
●Newborn screening reveals low T4 and high TSH
Identify interventions for hypercyanotic spells
●Plan interventions to allow maximal rest for the child; keep the child as stress-free as possible
Describe the four defects that make up the Tetralogy of Fallot (TOF)
○VSD
○Right Ventricular Outflow obstruction (pulmonic stenosis)
○Right Ventricular Hypertrophy
○Overriding Aorta
Identify normal intracranial pressure vs. elevated ICP as well as sign/symptoms of increased ICP in children
•Normal ICP: 5-15 mm Hg
•Elevated ICP defined as ICP > 20mm Hg for 5 minutes or longer
•Signs and Symptoms:
Headache, Irritability, Lethargy
Vomiting, High-pitched cry
Increased head circumference, bulging fontanelles *highlighted yellow*
Papilledema/visual disturbances, downcast “sunset” eyes
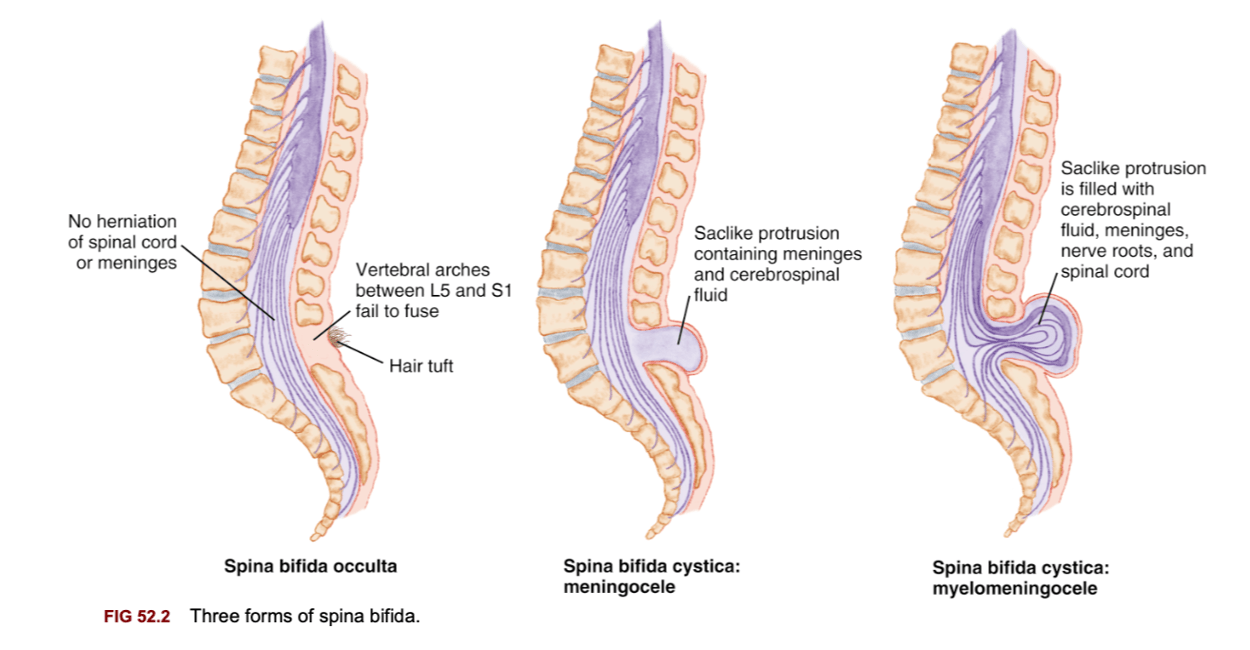
Describe spina bifida and how it is managed as well as what determines the degree of deficit
•Congenital neural tube defect
•Incomplete closure of vertebrae and neural tube during fetal development
•3 types: Occulta, meningocele, or myelomeningocele (most common)
•Etiology unknown but likely genetic disposition and maternal folic acid deficiency highly associated
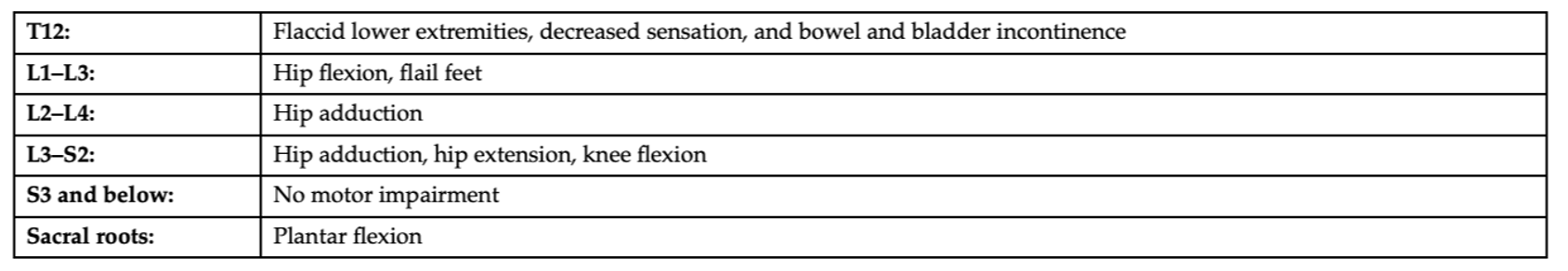
•Motor impairment and degree of deficit depends on level of lesion (Fig 52.3)
Compare different types of seizures and seizure activity vs. status epilepticus
Seizures
•Misfiring of cortical neurons of the brain
•Classified as general or focal
•General arise from cortex
•Focal arise from one specific area of cortex
•Multiple etiologies – genetic, symptomatic, idiopathic conditions
•Absence Seizures
•Staring spells
•Child cannot “snap out of it” or respond during spells
•Febrile Seizures
•Most common type of childhood seizure; ages 6 months to 5 years
•Typically occurs with fever > 101F
•Seizure Diagnostics
•CT/MRI if suspected lesion/mass
•EEG or Video EEG to monitor neural activity (may be 2-24hrs long)
•Monitor for electrolyte derangements
•Seizure Treatment
Antiepileptic medications, ketogenic diet, vagus nerve stimulation
STATUS EPILEPTICUS:
•Medical emergency: prolonged seizure activity > 5 minutes OR recurrent seizures for > 5 minutes with no return to baseline in between seizures
•Most common in children < 5 years old and in children with febrile seizures < 3 years old
•Prolonged seizure activity leads to lactic acidosis & increased ICP
•May require sedation/intubation
Describe diagnostics for sickle-cell anemia
•Diagnostics:- Hemoglobin Electropheresis: predominance of hemoglobin S with no hemoglobin A
-CBC- Hgb < 10 at baseline, HCT 20-29%; Retic: elevated 5-15%
Morphology: Howell-Jolly bodies, nucleated RBCs, sickled cell shape
Understand manifestations, management, and prognosis of neuroblastoma
-Manifestations:
•Vary based on severity of disease: Firm abdomen, may palpate abdominal mass, gait changes, dark circles under eyes, poor weight gain, opsomyoclonus
-Management & Nursing Considerations
•Surgical removal, Chemotherapy, radiation, Immunotherapy (immune modulators- Dinatuximab), Autologous SCT
•High risk disease survival rate approx. 20-25%
•Neuroblastoma has a high relapse rate
Understand clinical manifestations of congenital hypothyroidism in a
newborn as well as an untreated infant
●Symptoms in the newborn
○Long gestation (>42 weeks)
○Large, hypoactive infant
○Delayed meconium passage
○Feeding problems: poor suck reflex
○Prolonged physiologic jaundice
○Hypothermia
●Symptoms in untreated infant: large protruding tongue, coarse hair, sleepiness, flat expression, hypotonia, constipation
Describe the most common congenital heart disease
●Most common anomaly is ventricular septal defect (VSD)
●An opening in the septum between the ventricles allows blood to shunt between the left and right ventricles
●Increased pulmonary blood flow
●Clinical manifestations
○Thin, small infant, loud/harsh murmur, palpable thrill, liver/heart/spleen enlargement, feeding difficulties, diaphoresis
Understand Rheumatic fever, its manifestations, diagnosis, and
therapeutic management
●Develops after infection of the upper respiratory tract; usually 2-6 weeks after Group A streptococcal (strep) infection
●Most serious complication is rheumatic heart disease
●Clinical manifestations
○chorea , fever, carditis, erythema marginatum, abdominal pain
○Polyarthritis or migratory joint pain
○Aschoff bodies: rash on trunk or inner aspects of the upper arms or thighs that gives rise to red lesions with blanched centers
■Found in the heart, blood vessels, brain and serous surfaces of the joints and pleura
●Therapeutic management
○Treat any remaining group A streptococcal bacteria, relieve symptoms, control inflammation
○Treatment with penicillins for 10 days
Describe methods for monitoring and relieving increased ICP
•Monitoring Elevated ICP:
•ex: external ventricular drain (EVD)
•Treating Elevated ICP:
•Drain CSF
•Craniotomy for decompression
•Treat underlying cause (ex: debulk mass)
•Patient positioning: elevate HOB 30 degrees
•Passive hypocapnia
Understand causes of hydrocephalus, how it is managed, and risk factors associated with VP shunts
•Imbalance between production and absorption of CSF
•Increase in CSF = ventricles become dilated and brain is pressed against skull
•If sutures are open, bulging skull will enlarge to compensate, if sutures are fused, ICP increases
•Congenital, acquired, our known etiology
•Congenital: arachnoid cysts, aqueductal stenosis, tumors, chiari malformations
•Acquired: maternal infection, meningitis, subarachnoid hemorrhage.
•Goal: Drain fluid from ventricles to an area it can be reabsorbed
•Ventriculoperitoneal (VP) shunt: drains from ventricle of brain to peritoneal cavity
•Shunt malfunction is common (85% of patients need revision): under/over draining or child growth
•Shunt infection: monitor closely for fever, assess risk
•Children with VP shunts receive 1-3 CTs per year- consider radiation exposure
Understand nursing implications for seizures and status epilepticus
•Remain with patient during seizure
•Time the seizure and observe/record characteristics
•Ensure adequate oxygenation/perfusion
•Maintain safe environment
•Do not restrain the child
•Turn the child on their side, they may need suction if vomiting occurs
•Do not put anything in the patient’s mouth while seizing
•Allow for rest after seizure (post-ictal phase)
•Patients with seizure history should *always* have a PRN antiepileptic ordered
•Epilepticus
•As the seizure activity approaches 5 minutes, notify provider
•Prepare to administer antiepileptic drugs
•Consider code cart at bedside
Describe management and nursing considerations for sickle-cell anemia
-Nursing management/Considerations:
•Monitoring for infection (patients with SCA are immunocompromised); often on Penicillin V prophylaxis
•Fevers are an emergency in children with SCA (typically > 100.4F)
•Often on folic acid supplementation
•Pain may be controlled with NSAIDs and acetaminophen but often requires opioid management ; often needs admission for pain management
•Have non-judgmental attitude towards pain tolerance/need for opioids
•Patients on PCA should always be on continuous monitoring
•Consider bowel regimen for patients on high dose opioids
•In severe disease, may take Hydroxurea- which stimulates fetal hemoglobin production (Hgb F), decreasing Hgb S- this drug is immunosuppressive
•Close assessment of hepatosplenomegaly
•Close neurologic monitoring for increased risk of stroke
•Assess for any new changes in pain or new onset of pain (especially chest pain)
•Encourage maintaining daily routine as best as possible during VOD
•
Describe the major difference between neuroblastoma and Wilm’s tumor
NEUROBLASTOMA =
-TUMOR CAN ORIGINATE ANYWHERE
-MOST COMMON IS THE ABDOMEN, ABOVE ADRENAL CORTEX
WILM'S TUMOR=
-MOSTLY UNILATERAL RENAL TUMOR
Describe signs/symptoms of phenylketonuria (PKU) as well as patient
education and dietary considerations
●Signs and symptoms
○Frequent vomiting , Failure to gain weight , Irritability, Musty odor of urine, blonde haired, blue-eyed children & fare skin tones, may have microcephaly
●Dietary Management
○Strict low-phenylalanine diet
○Special formulas for infants
■Lofenalac
■Phenex-1
○Phenyl-free milk substitute after age of 2 years
○Avoid foods high in phenylalanine
■Includes high-protein foods such as meat, milk, dairy products and eggs
○Offer foods low in phenylalanine
■Includes vegetables, fruits, juices, cereals, breads and starches
○Diet should be followed until ages 6-8 years old when brain growth is complete to prevent cognitive deficits
Understand cyanotic vs. acyanotic defects
○Acyanotic= Increased pulmonary blood flow; obstruction to blood flow from ventricles
○Cyanotic =Decreased pulmonary blood flow; mixed blood flow
ACYANOTIC HEART DEFECTS:
●VENTRICULAR SEPTAL DEFECT (VSD)
● ATRIAL SEPTAL DEFECT (ASD)
●PATENT DUCTUS ARTERIOSUS (PDA)
● COARCTATION OF THE AORTA (COA)
AORTIC STENOSIS
CYANOTIC HEART DEFECTS:
1.Hypoplastic Left Heart Syndrome (HLHS)
2.Tetrology Of Fallot (TOF)
3.Truncus Arteriosus
4. Transposition of Great Vessels
Define systemic hypertension and primary causes in pediatrics
●Consistent elevation of BP (exceeds 95th percentile for age, height, and gender on three separate occasions)
○Primary CAUSE (idiopathic; not related to underlying disease)
○obesity, family history of HTN, emotional stress
○More common in adolescents/older children
Understand Cushing’s Triad and therapeutic management of cerebral edema/herniation
Cushing's Triad: Bradycardia, Respiratory Changes, and Hypertension
Treatment:
•Hypertonic fluid resuscitation (3% normal saline: pediatrics 3-5ml/kg)
•Loop diuretics
•**Avoid by slow correction of electrolyte derangements**
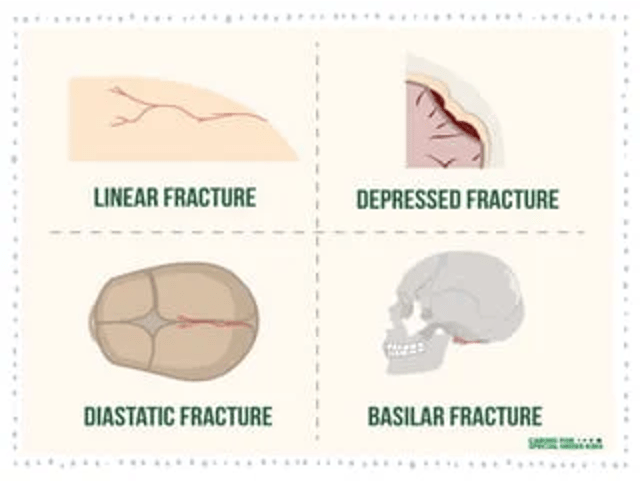
Understand clinical findings associated with basilar skull fracture
•Basilar: Fracture at base of skull
•+Battle sign, racoon eyes, rhinorrhea, otorrhea, TMs bulging with blood

Understand signs/symptoms of acute chest syndrome
•New onset of chest pain in SCA always warrants a chest x-ray
•Decrease in O2 saturations, increased RR, or increased WOB warrants notifying the provider
Describe treatment difference between Ewing’s Sarcoma and Osteosarcoma
•Ewing’s IS radiosensitive (Osteosarcoma is not)
Describe how type 1 Diabetes Mellitus is diagnosed in children and its
accompanying assessment findings
●Diagnosis
●Based on the presence of class symptoms and an elevated blood glucose level
●Hemoglobin A1C > 6.5%
●Fasting blood glucose > 126 OR 2-hour fasting glucose > 200 OR a one time glucose > 200 with clinical manifestations
●Children are usually diagnosed and admitted once parent notices a changes, which is typically when the child is in diabetic ketoacidosis (DKA)
●Glycosylated hemoglobin (HgbA1c) is performed every 3 months
●Goal is to be less than 6%
●Assessment
○Polydipsia, Polyphagia, Polyuria
○Enuresis in previously continent child
○Irritability, fatigue, weight
○Hyperglycemia, headaches, vaginitis in girls (Candida)
○Dehydration, slow wound healing
Describe manifestations of patent ductus arteriosis (PDA)
●Clinical manifestations:
○Characteristic machinery-like murmur
○Respiratory distress with signs of heart failure in infants, thrill palpated, bounding peripheral pulses, widened pulse pressure, failure to thrive, fatigue
Understand benefits and appropriate use of echocardiogram vs.
electrocardiogram
●Electrocardiography (ECG, EKG)
-Provides a graphic representation of the heart’s electrical activity
-Used to detect ischemia, injury, necrosis, bundle-branch block, fascicular blocks, conduction delay, chamber enlargement and arrhythmias
-Perform when child is quiet/still; no lotions on skin
●Echocardiography
○A graphic record of walls, valves, and vessels of heart produced by ultrasound
○May require sedation; follow sedation (NPO) guidelines
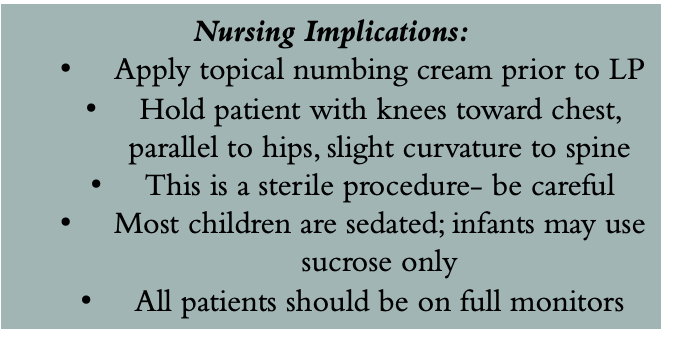
Understand the purpose of a lumbar puncture and nursing implications during the procedure
•Collect CSF for culture, glucose, protein and other diagnostic studies
•Can determine CSF involvement of infection or malignancy
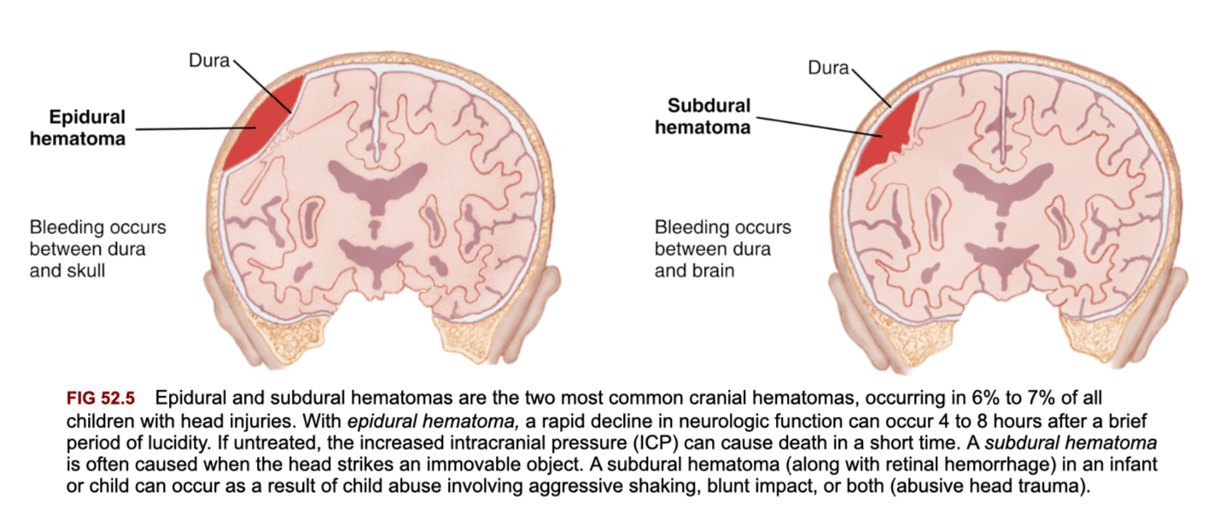
Compare and contrast epidural vs. subdural hematomas and level of head injury based on Glasgow Coma Score
•Epidural
•Blood between dura and skull
•Hemorrhage develops rapidly
•Subdural
Blood between dura and cerebrum
Can be acute or chronic.'
GCS Scores with Head Injury:
•GCS 13-15: Minor injury
•GCS 9-12: Moderate injury
•GCS 3-8: Severe injury
Describe nursing considerations for ITP and hemophillia
•Often no treatment indicated if no active bleeding
•If platelet count < 20 or active bleeding, IVIG infusion
•Avoid contact sports and activities at risk for bleeding, avoid aspirin, NSAIDs, or any other medications that cause bleeding
Understand the hallmark finding of retinoblastoma
LEUKOCORIA, A WHITE PUPIL WHEN LIGHT SHINES INTO THE EYE
•Pain, redness, inflammation of the eye
Vision loss from one eye (often not reported by children
Understand lab findings and manifestations of diabetic ketoacidosis
●Lab Findings:
●Blood sugar is greater than 200 mg/dL
●pH 7.3
●Low bicarbonate (HCO3)
●Ketonuria
Manifestations= Signs of hyperglycemia, Kussmaul's respirations, acetone (fruity breath)odor, N/V, abdominal cramps, increasing lethargy, decreased LOC
Describe manifestations of coarctation of the aorta (COA)
●Clinical manifestations
○Blood pressure is higher in the upper extremities than in the lower extremities
○Bounding pulses in the arms, weak or absent femoral pulses, cool lower extremities
○Headaches, dizziness, fainting, and epistaxis resulting from hypertension
Describe the standard terms for level of consciousness

Understand nursing implications for traumatic brain injury
•Assess ABCs
•Assess and monitor neurologic status
•Monitor for changes/decompensation
•Increased ICP and seizures may develop after injury *know signs of increased ICP*
•Child’s neck must be immobilized to decrease spinal injury
•Cannot be removed by nurse, must be cleared by physician
•Hypothermia (cooling blankets) may be used to decrease swelling of brain tissue
•Low stimulation/active and rest
•Typically refrain from school 3 days post injury or until able to tolerate 30 minutes of stimulation
•NG-tubes and Nasal suction contraindicated in basilar skull fractures
•Monitor fluid and electrolytes
•Damage to hypothalamus can cause DI or SIADH (if posteriori pituitary injury)
•Strict I&O
•Post-Concussion syndrome
•Common in moderate TBI
•Symptoms: Aggression, irritability, headaches, inattention, impaired concentration, dizziness, anxiety; typically resolve within a month post injury
•If Sports Injury:
•Must be cleared by physician, asymptomatic at rest and exertion, have competed any therapy that could improve condition, must allow 7-10 days minimum of rest; must be instructed to quit sports if multiple injuries
•Discharging Home:
•Educate families to bring child to emergency department or call 911 for the following: bleeding from nose/ears that doesn’t stop with pressure application, difficulty breathing, difficulty awakening, changes to pupils/vison, severe headaches, persistent vomiting, seizures, pallor/color change for > 1 hour.
Compare and contrast ALL and AML for childhood leukemia
list (1) diagnostic studies:
Fever:
-Acute Lymphoblastic Leukemia (ALL):
•Most common in pediatrics
•May be T-cell or B-Cell More common in school-age children
•2-3 years of treatment, predominately outpatient
-Acute Myeloid Leukemia (AML):
•Shorter, more intense treatment (6-9 months of mostly inpatient treatment)
•Typically more aggressive with higher relapse rate than ALL
*DIAGNOSTIC STUDIES:presence of blast cells on differential is always malignant
*•Patients are assumed to be immunocompromised at all times, fevers > 100.4F are emergent
Understand laboratory findings and nursing interventions for tumor lysis syndrome
•Lab values: Hyperkalemia, Hyperuricemia, Hyperphosphatemia, Hypocalcemia
•Nursing interventions: monitoring of electrolytes (may have every 6 hour labs or more frequently), continuous VS monitoring, no fluids containing potassium, monitor for cardiac/neuro changes (consider EKG), administer anti-uricemia medications
Describe the treatment for DKA and nursing considerations when
caring for a patient in DKA
●Treatment
●Typically treated in the Pediatric ICU due to need for insulin drip
●Often require dextrose containing IV fluid titration to not drop glucose too rapidly
●*SLOW* Correction of hyperglycemia
●Nursing Considerations
●Patient should be on on continuous, full monitoring
●Hourly or every 2-hour glucose checks
●Strict I&O
●Monitor neuro status closely: change in neurologic status is indicative of too rapid glucose correction which may lead to cerebral edema
Understand mechanism, complications, and management of
hypoplastic left heart syndrome (HLHS)
Inadequate development of left side of heart, predominately left ventricle
●If untreated, death within first few months of life (rapid progressive heart failure)
●Manifestations: grayish blue infant with hypoxia, dyspnea and hypotension
●Management:
●Emergent PGE1 to maintain PDA until surgery
●Surgical: transplant or Norwood/Fontan repair
Describe the implications of flexion and extension posturing

Describe clinical findings and nursing considerations of meningitis
•Infectious process of CNS
•Can be viral, bacterial, or fungal
•Examples of bacterial pathogens: E. Coli, N. Meningitidis, Strep Pneumoniae
•Examples of viral pathogens: Herpes simplex virus, mumps, enterovirus
•Fungal meningitis uncommon but may occur in immunosuppressed
•Clinical Findings
•Neonates: may have poor sucking/feeding, poor muscle tone, weak cry
•Infants & kids: vomiting, diarrhea, fever, headache, appetite changes, altered LOC, nuchal rigidity
•Diagnosed through CSF interpretation
•Acute bacterial meningitis is medical emergency requiring high dose IV antibiotics
•Nursing Considerations
•If N. Meningitidis, all close contacts are treated with oral Rifampin (remember this turns urine orange)