Passive vs active motion: What is the significance of a patient displaying weakness in one of these types of motion?
Narrows down the differential diagnosis
Bonus: Since our patient had limited active ROM but intact passive ROM, how would our differential be narrowed?
What laboratory findings support the diagnosis of dermatomyositis?
↑↑ creatine kinase, ↑ aldolase, ↑ myoglobin, ↑ LDH, ↑ AST, ↑ ALT (indicate muscle damage and inflammation)
Positive ANA (commonly seen in autoimmune diseases, although nonspecific)
Anti-Jo-1 Antibodies (specific for dermatomyositis)
Bonus: What is the typical biopsy finding in dermatomyositis that helps confirm the diagnosis?
Bonus: Which type of T cell is primarily involved in this inflammatory response?
Which cytokines and immune cell types are prominently involved in the inflammation seen in dermatomyositis, polymyositis, and SLE, and how do their roles differ across these autoimmune conditions?
Type 1 interferons, TNF alpha, IFN-gamma, IL-1, IL-6
Bonus:
Give a general idea of what each cytokines purpose is
How does levothyroxine (L-thyroxine) restore thyroid function in patients with hypothyroidism, and what mechanisms lead to the potential adverse effects of thyrotoxicosis with long-term use?
It is a synthetic form of T4 which helps restore normal thyroid function by compensating for the body’s low thyroid hormone levels.
Bonus:
What are some of the potential adverse effects of this drug?
A 48-year-old woman presents with a 3-month history of progressive muscle weakness, particularly in her hips and shoulders. She also reports a rash seen below. Laboratory tests show elevated creatine kinase (CK) levels. What would be your highest differential and what is the name of this rash?
Dermatomyositis; Gottron papules
Bonus: How do you know this is Gottron papules?
How does the muscle biopsy in polymyositis differ from that in dermatomyositis?
Polymyositis shows endomysial inflammation with CD8+ T cells and muscle fiber necrosis.
The perifascicular atrophy in dermatomyositis is due to vascular involvement and hypoperfusion, primarily affecting the muscle fibers at the edges of each fascicle. This often leads to proximal muscle weakness similar to polymyositis, but with the addition of characteristic skin findings (e.g., heliotrope rash, Gottron’s papules) and a higher likelihood of systemic features due to vascular involvement.
Bonus: How does this feature correlate with the clinical presentation?
The key cells involved in creating the inflammation seen in polymyositis?
CD8+ T cells
The T cells recognize the MHC 1 molecules expressed by the muscle cells and this leads to the death of those muscle fibers. Since this process is mediated by these CD8+ T cells, the findings vary from other kinds of myopathies. There can be regions of necrotic and regenerating muscle fibers scattered throughout the fascicle. However, non-necrotic myofiber invasion may also be seen.
Bonus:
What part of the muscle is affected by this disorder?
Explain the pathogenesis of each of the 2 drugs that we stopped. (Colchicine and Statin)
Colchicine impairs transport of organelles which puts people at a risk for myopathies. Statins can cause the production of an antibody which can contribute to the development of an immune-mediated necrotizing myopathy.
What are the autoantibodies that typically present with myositis?
ANA, anti-Jo-1, anti-SRP, anti-Mi-2
Do the autoantibodies differentiate what kind of myositis a patient may have?
What findings would you expect on a muscle biopsy in Duchenne muscular dystrophy, and why might biopsy not be necessary if genetic testing is available?
A muscle biopsy in Duchenne muscular dystrophy shows muscle fiber degeneration and necrosis, replacement with adipose and connective tissue (pseudohypertrophy), and reduced or absent dystrophin on immunostaining.
Biopsy may not be necessary if genetic testing confirms a dystrophin deletion.
Bonus: Why is Duchenne muscular dystrophy often diagnosed earlier than Becker muscular dystrophy?
Bonus: How can an echocardiogram be useful in the management of patients with Duchenne muscular dystrophy?
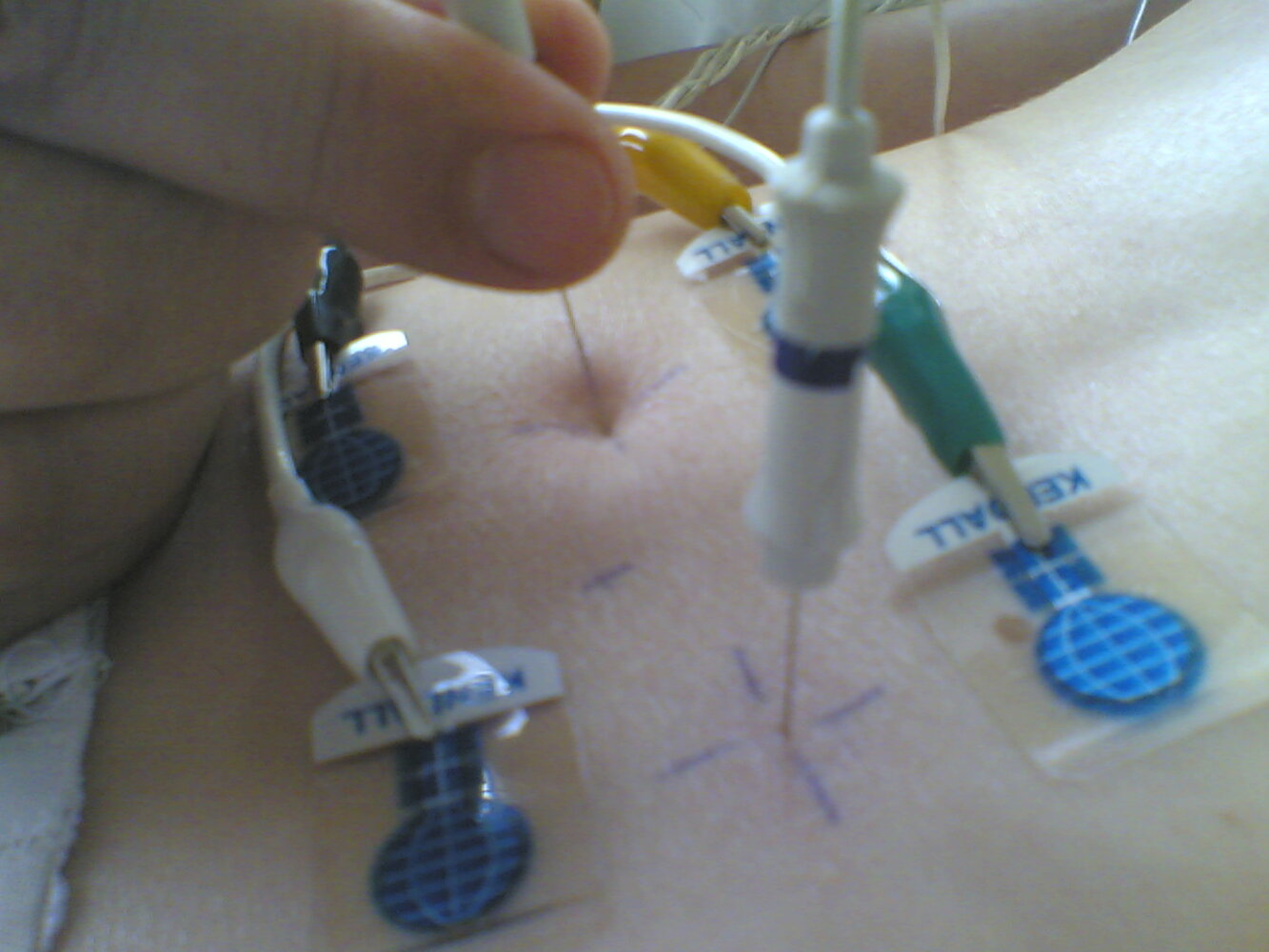
The key cells involved in creating the inflammation seen in dermatomyositis?
CD4+ T cells
Bonus:
What part of the immune system is responsible for the actual killing of these muscle fibers?
What part of the muscle is affected by this disorder?
Riddle: I am the cause and the cure of myositis. What am I?
Answer: corticosteroid
Cause: corticosteroid-induced myositis
Cure: first-line treatment for myositis
A 40-year-old woman presents with generalized muscle weakness and photosensitivity. She has a reddish-purple rash on her eyelids. Her laboratory tests reveal elevated CK levels and a positive ANA test, but anti-dsDNA is negative.
What is the most likely diagnosis?
A) Dermatomyositis
B) Systemic Lupus Erythematosus (SLE)
C) Polymyositis
D) Sjögren's Syndrome
A) Dermatomyositis
How does EMG differentiate between myopathic and neuropathic conditions?
In myopathic conditions, EMG typically shows short-duration (high frequency), low-amplitude motor unit potentials with increased spontaneous activity (such as fibrillations).
In neuropathic conditions, EMG shows long-duration (low frequency), high-amplitude motor unit potentials with reduced recruitment, reflecting nerve damage rather than muscle damage.
Bonus: What does increased spontaneous activity, such as fibrillations and positive sharp waves, on EMG indicate about muscle health?
Bonus: What does a short-duration, low-amplitude motor unit potential indicate?
What role do protein aggregates play in the development of inclusion body myositis, and how does this differ from the pathology seen in dermatomyositis and polymyositis?
Abnormal protein processing associated with aging and subsequent deposition of toxic polymers can cause muscle damage and can also trigger inflammation in the muscle fibers. The amyloid deposits are also thought to play a role in upregulating IL-6 which can further amplify the immune response.
Some myofibers appear to be injured by invading cytotoxic T cells, while others have no apparent cause for their morphological abnormalities and have been called degenerative.
What is the mechanism of corticosteroids, specifically glucocorticoids?
Answer:
Inhibit Phospholipase 2, which inhibits leukotrienes & prostaglandins. Both are inflammatory mediators.
Inactivates Nf-Kb, which is a transcription factor for activating many pro-inflammatory genes
Increase transcription of pro-inflammatory cytokines; i.e. IL-10
A 40-year-old woman with a history of interstitial lung disease presents via telemedicine with muscle weakness. She is positive for anti-Mi-2 antibodies and positive ANA antibodies. You suspect a myositis. Which of the following should be your next step as a physician?
A) Ask her to come in - explain to her that she has dermatomyositis and advise her to do an occult test as she has a higher risk of malignancy
B) Ask her to come in - examine her skin to determine if she is presenting with any skin abnormalities
C) Order creatine kinase to further differentiate the type of myositis the patient has
D) Ask her to come in - explain to her that she has polymyositis and advise her to do an occult test as she has a higher risk of malignancy
Answer: B
The MAIN differentiation in clinical presentation between polymyositis and dermatomyositis is skin involvement.
What genetic mutation causes both Duchenne and Becker muscular dystrophies, and how does this mutation differ between the two conditions?
Both Duchenne and Becker muscular dystrophies are caused by mutations in the dystrophin gene on the X chromosome.
In DMD, there is typically a deletion or frameshift mutation that results in the complete absence of functional dystrophin, leading to more severe symptoms.
In BMD, there is usually an in-frame mutation that allows for the production of a partially functional dystrophin protein, resulting in milder symptoms.
Bonus: How do the symptoms of muscle weakness differ between patients with Duchenne muscular dystrophy and those with Becker muscular dystrophy?
Bonus: What are the most common complications in both Duchenne muscular dystrophy and Becker muscular dystrophy, and how does the age of onset differ between the two?
What are the characteristic skin findings in dermatomyositis, and how does the underlying pathophysiology contribute to these manifestations?
Cytokine release and vascular involvement of the immune response can lead to ischemia in the skin and muscles. This leads to inflammation in the perivascular area which can present as skin lesions.
What are the mechanisms of action of prednisone in controlling inflammation, and what long-term adverse effects may occur with its use?
Prednisone binds to glucocorticoid receptors, moves to the cell nucleus, and modulates gene expression by increasing anti-inflammatory proteins and reducing pro-inflammatory proteins.
Long-term use can lead to corticosteroid-induced myopathy, which manifests as proximal muscle weakness, and muscle atrophy due to altered protein synthesis and breakdown.
Additional adverse effects include osteoporosis, hyperglycemia, hypertension, weight gain, and an increased risk of infection.
Bonus: What are some strategies that can help mitigate the complications associated with long-term prednisone use in dermatomyositis patients?
Bonus: Why is it recommended to taper prednisone gradually in dermatomyositis, and what risks are associated with abrupt discontinuation?