What are the common sites affected by plaque psoriasis?
Elbows, knees, and scalp (extensor surfaces).
What type of epithelium makes up the epidermis of the skin?
Keratinized stratified squamous epithelium.
What type of immune process drives psoriasis?
Chronic, immune-mediated inflammation.
Which shampoo ingredients would target the underlying pathophysiology of scalp psoriasis more effectively?
Coal tar, salicylic acid, or topical corticosteroid shampoos
Coal tar: Slows keratinocyte proliferation and reduces inflammation.
Salicylic acid: Keratolytic; removes scales and enhances penetration of other topicals.
Topical corticosteroids: Suppress cytokine-mediated inflammation and T-cell activity.
Name one key differential diagnosis for scalp psoriasis.
Seborrheic dermatitis.
This is caused by an overgrowth of Malassezia yeasts on the scalp.

Describe the typical appearance of psoriatic lesions.
Well-demarcated erythematous plaques with silvery-white scale.
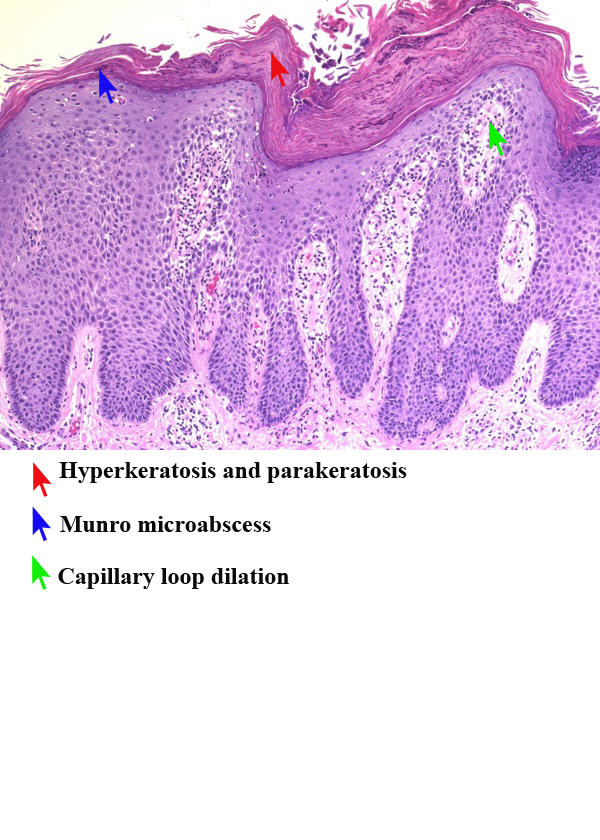
What is acanthosis?
Epidermal hyperplasia (thickening of the stratum spinosum).
Key words: thickened, velvety, and darkened patches of skin

What are key risk factors for psoriasis?
Family history, obesity, infection, smoking, stress
What is the mechanism of topical corticosteroids?
Reduce inflammation by suppressing cytokine production and T-cell activity.
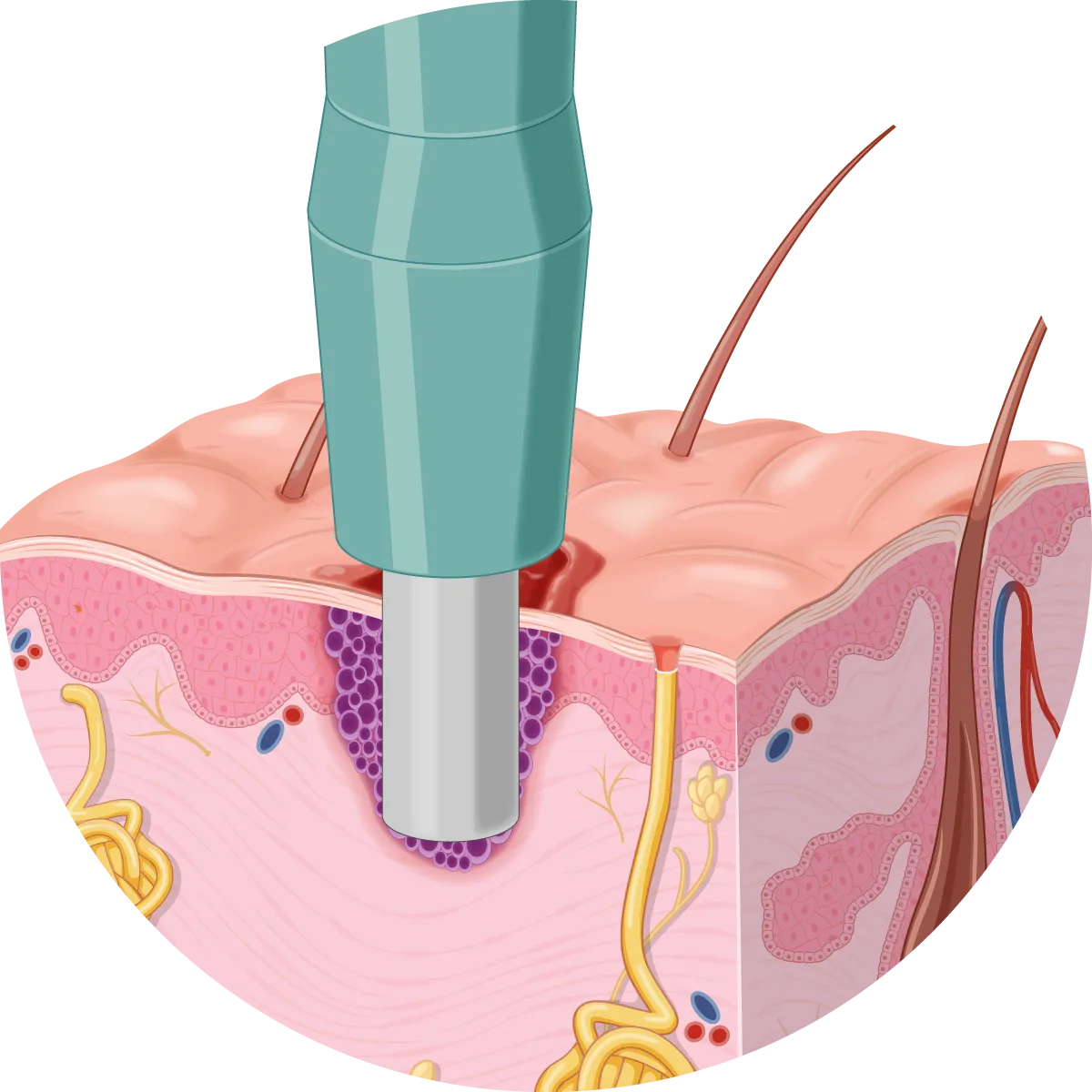
What test can confirm a psoriasis diagnosis?
Skin punch biopsy.
What nail findings are associated with psoriasis, and what do they suggest?
Nail pitting, thickening, and onycholysis (nail separation) - suggest possible psoriatic arthritis.
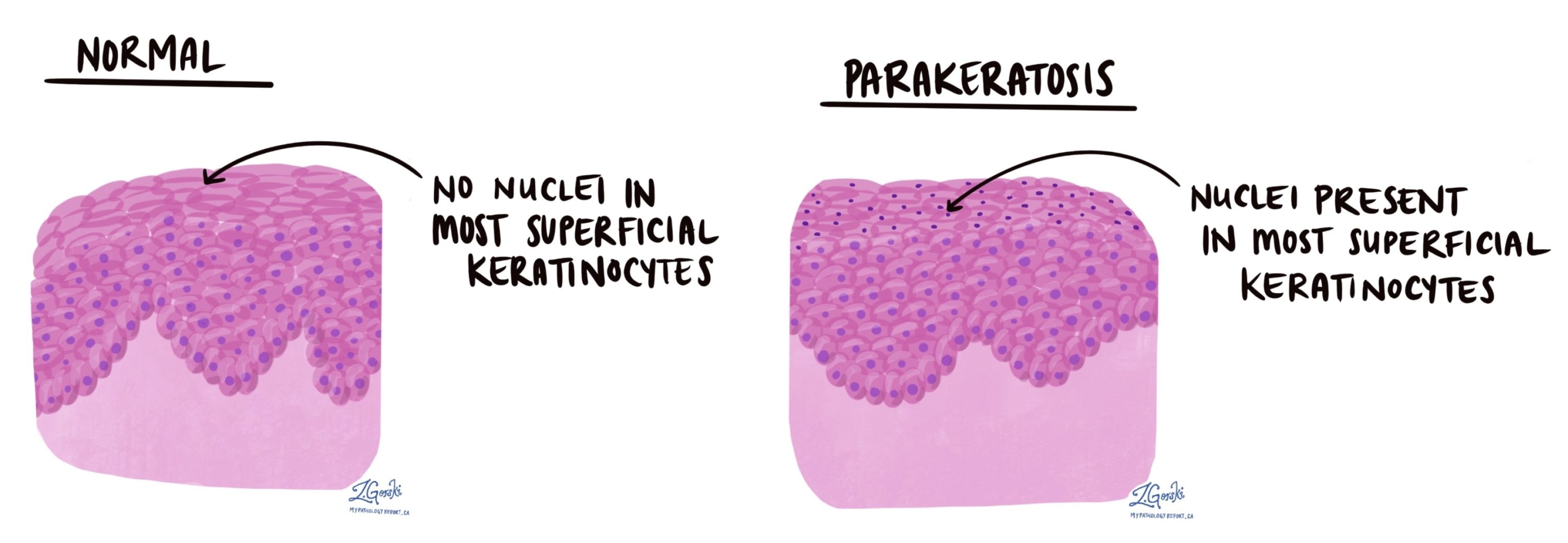
What causes the silvery-white scale on psoriatic plaques?
Parakeratosis: retention of nuclei in the stratum corneum.
Which cytokines are central to the inflammatory cascade in psoriasis?
TNF-α, IL-12, IL-17, and IL-23.
Immune mediated. Not infectious.
What are the major pros and cons of immune-modifying drugs?
Pros: Highly effective, improves quality of life
Cons: High cost, infection risk, insurance barriers, lab monitoring.
How do you differentiate psoriasis from eczema clinically?
Psoriasis = well-demarcated plaques on extensor surfaces
Eczema = poorly defined lesions on flexor surfaces, very pruritic (itchy).
What is the Koebner phenomenon, and how does it relate to this case?
Lesions appear at sites of skin trauma; explains involvement of knees/elbows.
What are Munro microabscesses?
Collections of neutrophils in the stratum corneum.
Compare the acute vs. chronic immune response in psoriasis.
Acute: dendritic cell activation → cytokine release
Chronic: sustained Th1/Th17 (T-cells) activation and keratinocyte proliferation.
How does ustekinumab work?
Monoclonal antibody targeting IL-12 and IL-23 to block Th1/Th17 activation.
The patient in our case used dandruff shampoo for months with no improvement. Why does a diagnosis of Psoriasis become more likely?
Antifungal or dandruff shampoos would typically improve seborrheic dermatitis but not immune-mediated psoriasis.
Differentiate between acute and chronic plaque psoriasis in terms of duration and stability of lesions.
Acute psoriasis describes a temporary, often sudden flare-up of small plaques (such as guttate psoriasis) that can resolve spontaneously. Chronic plaque psoriasis (psoriasis vulgaris) is the most common, long-lasting form characterized by large, persistent, stable plaques that may wax and wane but rarely resolve without treatment.
What is the Auspitz sign, and what histologic feature explains it?
Pinpoint bleeding when scales are removed- due to dilated capillaries in dermal papillae and thinned suprapapillary plates.

Explain how keratinocyte hyperproliferation and angiogenesis cause the visible plaques.
Cytokines stimulate keratinocyte overgrowth and capillary dilation → thickened, red, scaly plaques.
Compare ustekinumab and tacrolimus in terms of mechanism and use.
Ustekinumab = biologic (IL-12/23 blocker)
Tacrolimus = calcineurin inhibitor for localized lesions (esp. face/flexures).
Dr. Wild performed a punch biopsy on Mr. Green even though psoriasis is often a clinical diagnosis. Why was this diagnostic test appropriate, and what additional information does it provide?
A biopsy is indicated for atypical or resistant presentations. It confirms the diagnosis by revealing acanthosis, parakeratosis, and neutrophilic infiltrates, and helps exclude eczema or fungal infections, guiding accurate treatment decisions.