What artery comes before and after this one?
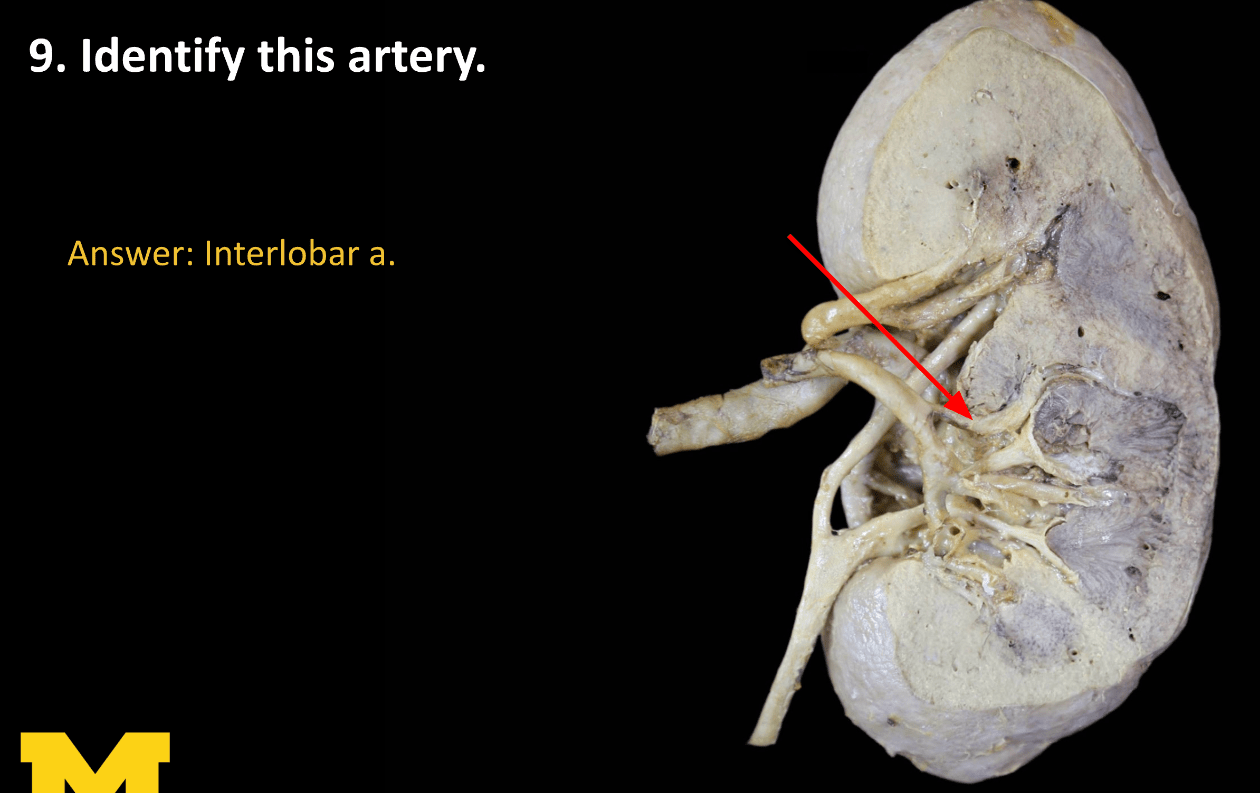
Segmental and arcuate arteries
This congenital condition results from failure of the ureteric bud to develop.
Renal agenesis. If ureteric bud doesn’t develop, it cannot induce the metanephric mesoderm to form nephrons, and therefore, a functional kidney does not develop.
This nephron segment is most vulnerable to ischemic injury (anoxia).
What is the proximal tubule (PCT) / thick ALOH
This hormone increases Na⁺ reabsorption and K⁺/H⁺ secretion in the collecting duct.
What is aldosterone?
What part of the Glomerular filltration barrier has a negative charge and what substance creates this charge?
Basement membrane and heparan sulfate creates negative charge
This pharmacokinetic parameter is not a true volume, but a proportionality constant relating plasma concentration to total body drug amount.
What is Volume of Distribution (Vd)?
This pharmacokinetic parameter describes the volume of plasma cleared of drug per unit time.
What is Clearance (Cl)?
Loop diuretics act on this transporter in the thick ascending loop of Henle.
What is the Na⁺/K⁺/2Cl⁻ cotransporter (NKCC)?
This condition is often caused by ascending bacterial infection (commonly E. coli) and marked by fever, costovertebral angle tenderness, and WBC casts
(Acute pyelonephritis)
This nephrotic syndrome of children shows normal glomeruli on LM, podocyte effacement on EM, and dramatic response to steroids.
What is Minimal Change Disease?
This nephritic disease follows a strep throat or skin infection and shows subepithelial “humps” on EM.
What is Post-streptococcal GN?
Identify this structure and what parts of the nephron are located in it?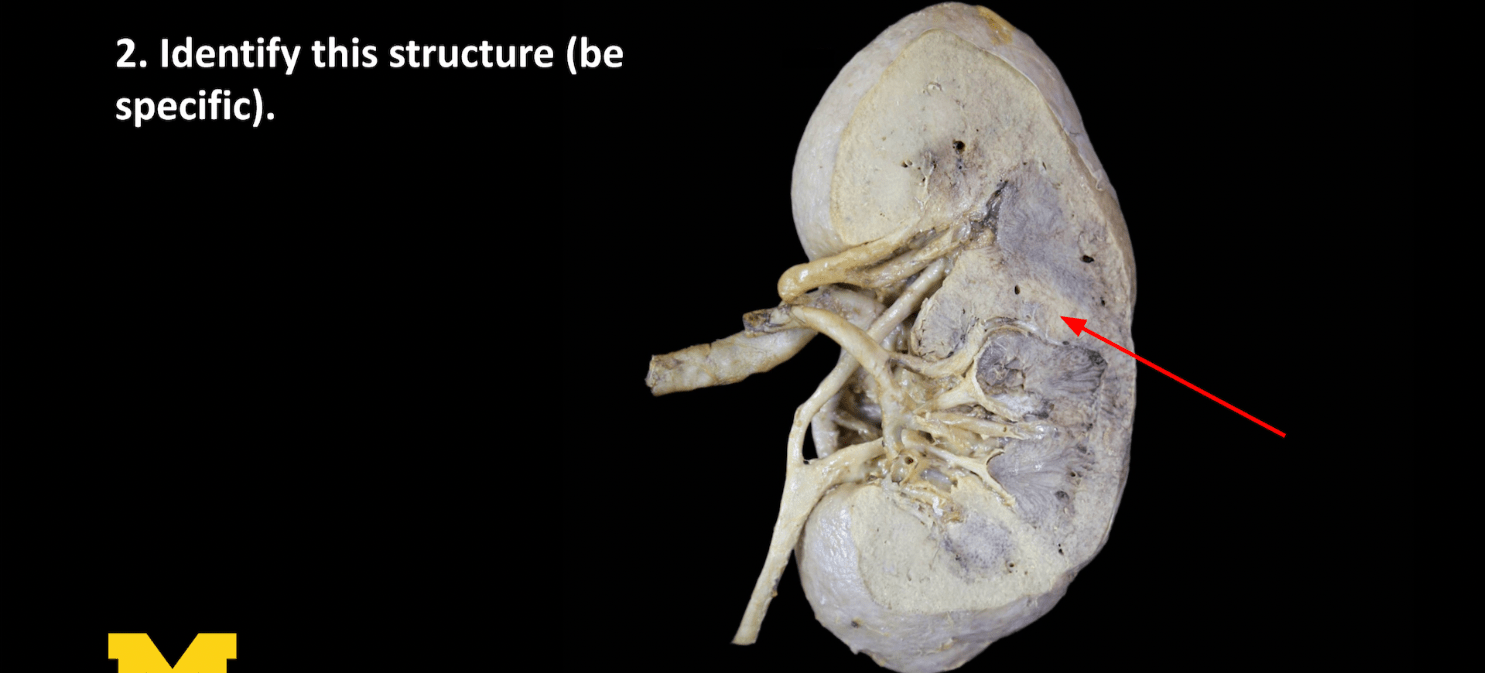
Renal column, which is part of the cortex, so it has the renal corpuscle, PCT, and distal convoluted tubule. DOES NOT include the LOH and collecting duct
Identify this structure AND what condition affects it?
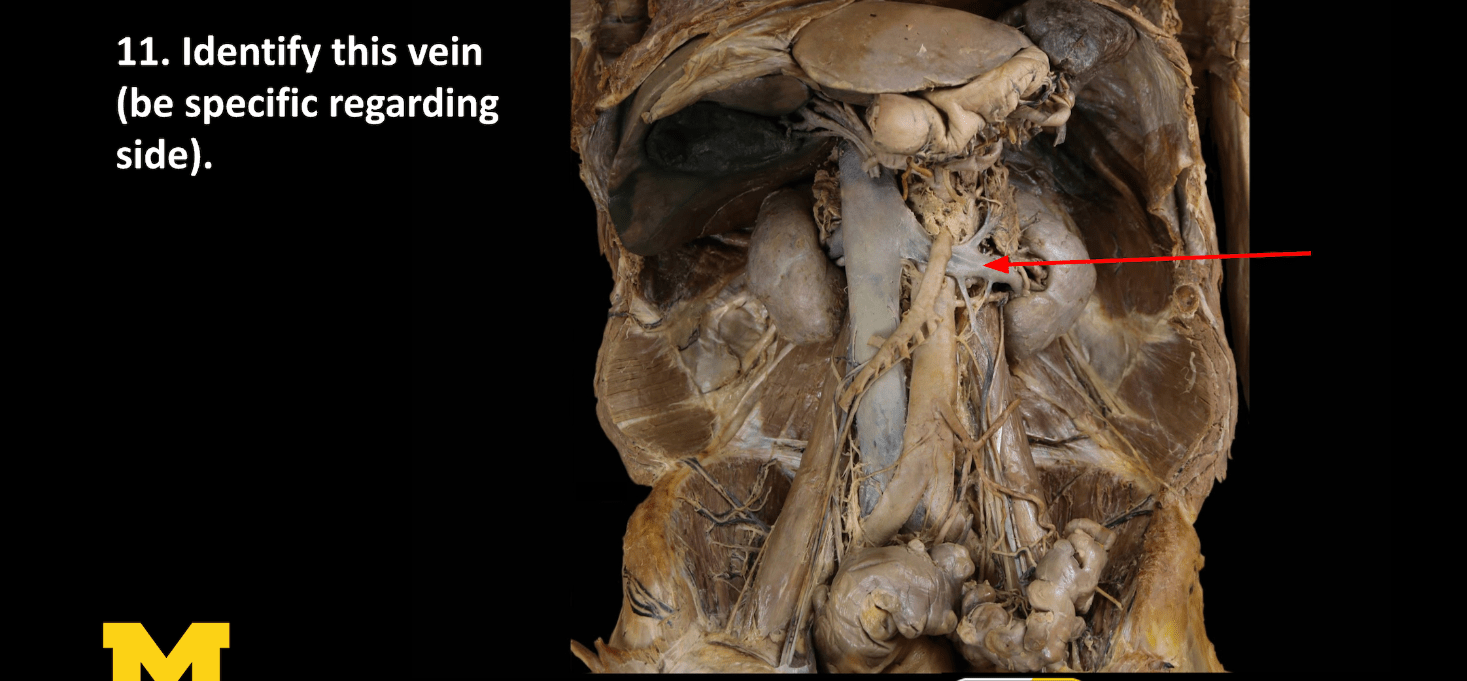
Left renal vein, Nutcracker syndrome
This condition has pulmonary hypoplasia, oligohydramnios, twisted face and skin, extremity defects, renal failure (in utero).
Potter sequence
This part of the kidney receives the highest blood flow and has relatively low metabolic demand, making it resistant to ischemic injury
What is the renal cortex?
Aldosterone acts primarily on these two cell types in the collecting duct.
What are principal cells (Na⁺ reabsorption, K⁺ secretion) and α-intercalated cells (H⁺ secretion)?
This substance’s clearance is used to measure GFR because it is freely filtered but neither secreted nor reabsorbed, while this OTHER substance clearance is used to estimate effective renal plasma flow since it is both filtered and actively secreted, leading to nearly 100% excretion.
Inulin and PAH
A drug that avidly binds to plasma proteins will have this type of Vd.
What is a small Vd (restricted to plasma)?
Organ clearance = blood flow × this parameter.
What is extraction ratio?
Thiazides increase serum calcium levels by stimulating this transporter mechanism.
What is the Na⁺/Ca²⁺ exchanger in the DCT?
Sickle cell disease/trait, Acute pyelonephritis, NSAIDs, and Diabetes mellitus are commonly associated with what condition?
Renal Papillary necrosis
This nephrotic syndrome, linked to HIV and heroin use, shows segmental sclerosis and hyalinosis on LM and responds poorly to steroids.
→ What is FSGS?
SNEAD NOTE: HIV and Heroin are specifically associated with COLLAPSING FSGS (more the factual clinical info than understanding the exact pathology since the histologic features of collapsing FSGS can look a lot like crescentic GN- this can even be hard for renal pathologists to distinguish!)
This syndrome shows linear IgG deposition along the GBM and presents with hematuria and hemoptysis.
What is Goodpasture Syndrome?
A patient with gout should avoid which two diuretic classes due to uric acid retention?
What are loop diuretics and thiazides?
What structure drains INTO the renal papilla and what structure does it drain INTO?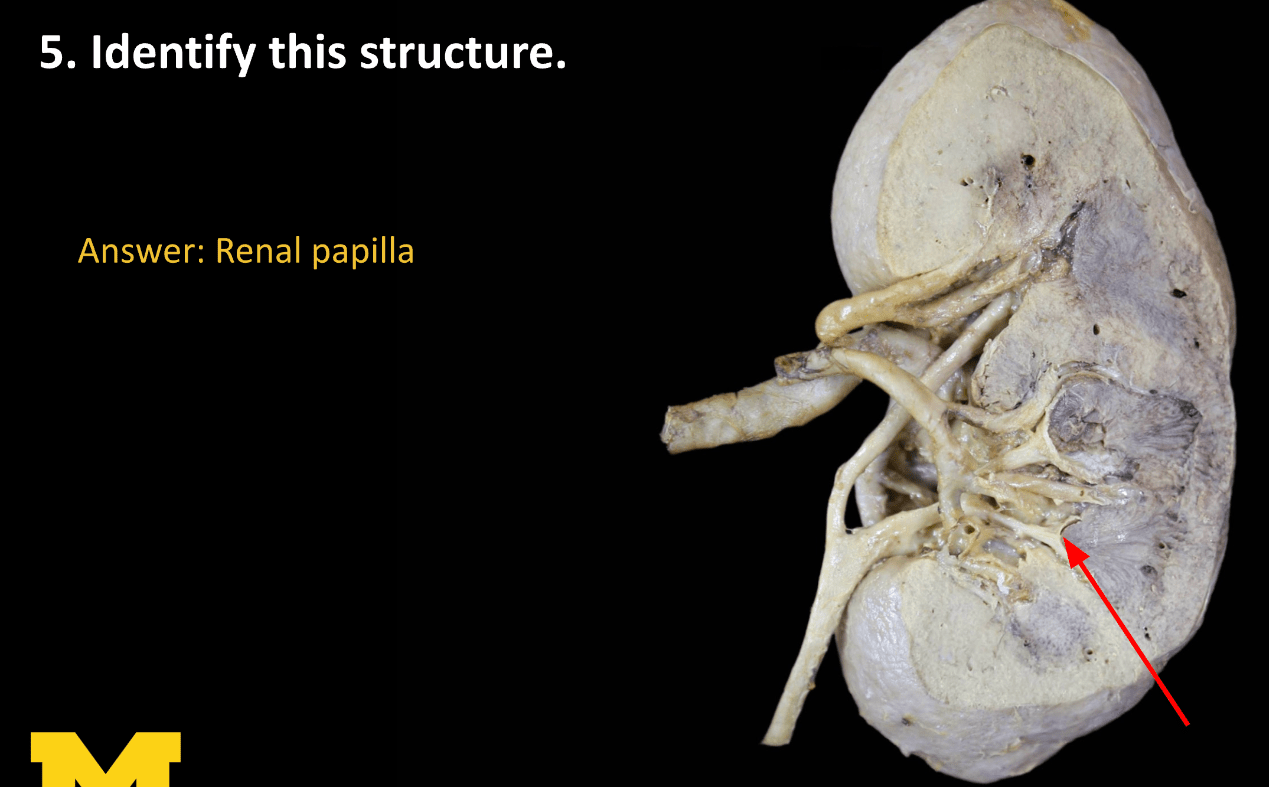
Collecting duct drains into renal papilla and renal papilla drains into minor calyx
This condition is when kidneys get trapped under inferior mesenteric artery and remain low in the abdomen. It is associated with hydronephrosis, renal stones, and chromosomal aneuploidy
Horseshoe kidney
This region of the kidney has much lower blood flow but higher metabolic demand due to active solute transport, making it especially vulnerable to ischemia.
What is the renal medulla?
This hormone inserts aquaporin-2 channels into the apical membrane of collecting duct principal cells.
What is ADH (vasopressin, V₂ receptor)?
This is the effect of an NSAID on RBF, GFR, FF, and Glomerular Oncotic Pressure
NSAID constricts the afferent, so RBF ↓, GFR ↓, FF -varies, GOP -varies
Ms. Smith receives 150 mg IV tobramycin. After 20 min, Cp = 3 mg/L. Assuming no elimination, what is her Vd?
What is 50 L (150 ÷ 3)?
A drug with a high hepatic extraction ratio will have this type of oral bioavailability.
What is low (due to first-pass metabolism)?
NSAIDs can blunt the diuretic effect of loops by inhibiting this local hormone
What is prostaglandin E₂?
There is increased risk for hyperkalemia and uremia in what phase of ATN?
The maintenance phase, as this is when the tubular cells are necrosing. The BUN & Creatinine increase because the GFR decreases, and the kidneys can not sufficiently filter these substances. There is oliguria.
In primary membranous nephropathy, this autoantibody targets a podocyte antigen
anti- PLA2R
This nephropathy presents with episodic gross hematuria after URI or GI illness and shares pathology with Henoch-Schönlein purpura.
What is IgA Nephropathy?
This lesion is pathognomonic for diabetic nephropathy and results from nonenzymatic glycosylation of proteins.
What are Kimmelstiel-Wilson nodules? SNEAD NOTE: the image is very classic, Kimmelsteil- Wilson nodules (also KW nodules) are the round, pregnant – looking sclerotic mesangial nodules
Identify this structure, and where does the homologous structure drain into on the RIGHT side?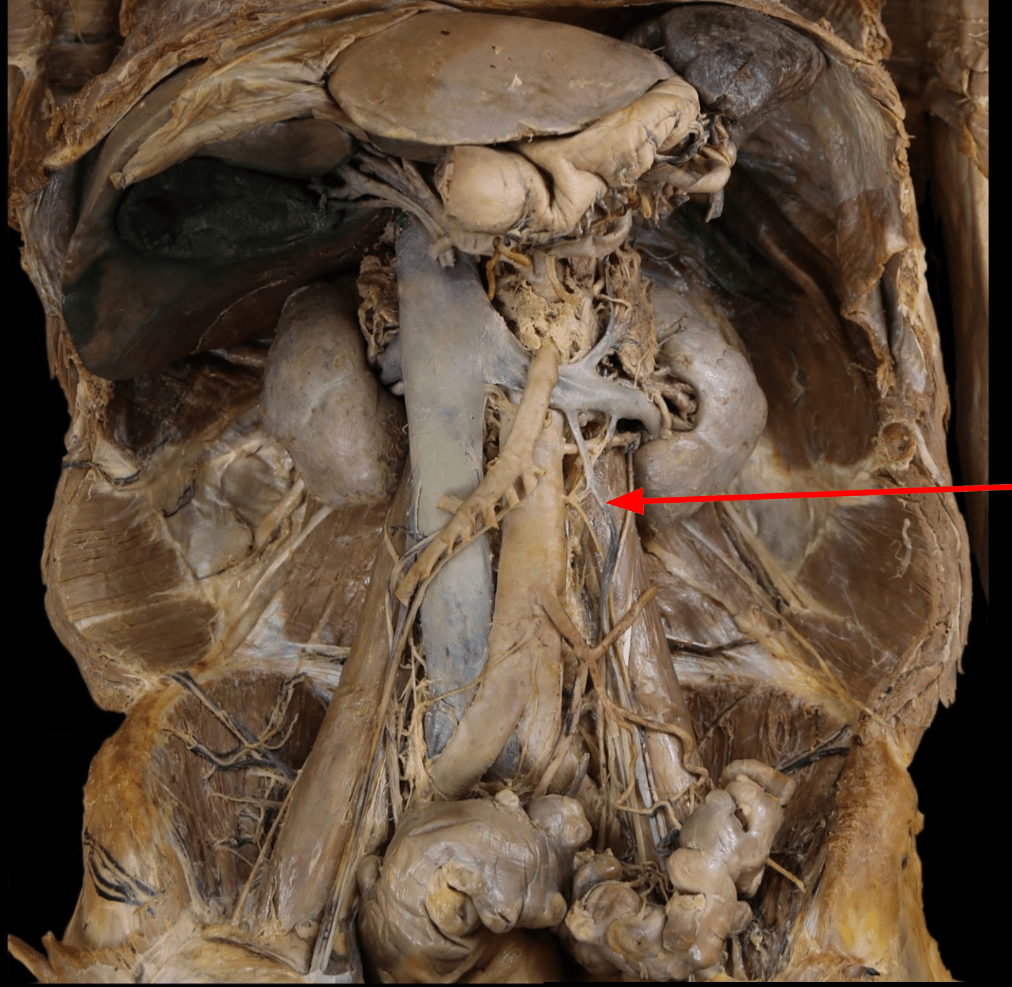
Gonadal vein, on the left drains into the left renal vein and on the right drains into the IVC
These are the three sequential kidney structures that develop in a cranial-to-caudal direction during embryogenesis.
pronephros, mesonephros, and metanephros
Damage to the PCT impairs reabsorption of these 4 key solutes, leading to Fanconi-like syndrome.
What are glucose, amino acids, phosphate, bicarbonate?
In the absence of ADH, the final urine osmolarity relative to plasma is this.
What is hypotonic (dilute urine)?
This is the effect of ACE inhibitors on RBF, GFR, FF, and Glomerular Oncotic Pressure.
Angiotensin II constricts the efferent, so it will dilate with an ACE inhibitor. RBF ↑, GFR ↓, FF ↓, Glomerular Oncotic Pressure ↓
If Vd increases due to tissue binding, what happens to half-life, assuming clearance is unchanged?
What is half-life increases (t½ = 0.693 × Vd ÷ Cl)?
A drug is eliminated at 10 mg/hr, Cp = 4 mg/L. What is Cl?
What is 2.5 L/hr?
Which two diuretic classes can cause metabolic acidosis, unlike loop/thiazides?
What are Carbonic Anhydrase Inhibitors and K⁺-sparing diuretics?
Thyroidization of kidney is associated with what condition?
Chronic pyelonephritis, as the tubules filled with eosinophilic casts, resembling thyroid follicles. SNEAD NOTE: (I could show a gross and a microscopic photo of this since it is so specific and distinctive)
Congo-red–positive glomerular deposits with apple-green birefringence under polarized light are most often due to this systemic disease.
AMYLOID
This X-linked nephritis causes hematuria, hearing loss, and ocular changes with “basket-weave” GBM on EM.
What is Alport Syndrome?
These three glomerular diseases are classically hypocomplementemic.
What are Post-strep GN, Lupus Nephritis, and MPGN (± Dense Deposit Disease)?