What structure connects the oropharynx to the trachea
Larynx
What are the most common pathogens for the common cold?
parainfluenza viruses, respiratory syncytial virus (RSV), human metapneumovirus, coronaviruses, and adenoviruses
What is the pathogen associated with tuberculosis?
Mycobacterium tuberculosis.
What is ventilation?
involves the movement of atmospheric air to the alveoli for provision of O2 and removal of CO2. Minute ventilation is the volume of air exchanged per minute and is determined by both the amount of air exchanged with each breath (tidal volume) and the respiratory rate (breaths/minute).
A client is prescribed albuterol, 2 puffs every 6 hours. After teaching the client about the drug and its administration, the nurse determines that the teaching was successful when the client states that they will allow how much time between each puff?
3-5 minutes
The client should allow 3-5 minutes to elapse between each puff of the inhaled medication.
What structures are consistent with the tracheobronchial tree?
trachea , bronchi, bronchioles
What are the clinical manifestations of the common cold?
begins with a feeling of dryness and stuffiness, affecting mainly the nasopharynx. This is followed by excessive production of nasal secretions and tearing of the eyes, which is often referred to as rhinitis. Usually, the secretions remain clear and watery. The mucous membranes of the upper respiratory tract become reddened and swollen. Often, there is postnasal dripping, which irritates the pharynx and larynx, causing sore throat and hoarseness. The affected person may experience headache and generalized malaise.
What is pathophysiology for a positive tuberculin test?
results from a cell-mediated immune response and implies that a person has been infected with M. tuberculosis and has mounted a cell-mediated immune response. It does not mean that the person has active TB.
What is required for adequate ventilation perfusion MATCHING?
Adequate oxygenation of the blood and removal of CO2 also depend on adequate circulation of blood through the pulmonary blood vessels (perfusion) and appropriate contact between ventilated alveoli and perfused capillaries of the pulmonary circulation (ventilation and perfusion matching) (
A 76-year-old client diagnosed with COPD has been taking ipratropium. The nurse knows what change in the client’s health status is most likely to require an adjustment in the client’s drug regimen?
The client begins taking a diuretic for hypertension.
- The client is diagnosed with benign prostatic hyperplasia.
- The client loses 15 lb (6.8 kg) over 8 weeks
The client develops a venous ulcer.
The client is diagnosed with benign prostatic hyperplasia.
Anticholinergics can produce urinary hesitancy and urinary retention, conditions that would aggravate the signs and symptoms of benign prostatic hyperplasia. Weight loss, venous ulcers, and the use of diuretics do not contraindicate the safe use of anticholinergics.
Where does gas exchange take place?
Terminal bronchioles and alveoli
Describe the pathogenesis of influenza?
three types of infections:
an uncomplicated upper respiratory infection (rhinotracheitis),
viral pneumonia,
respiratory viral infection followed by a bacterial infection.
Influenza initially establishes upper airway infection. In doing this, the virus first targets and kills mucous-secreting, ciliated, and other epithelial cells, leaving holes between the underlying basal cells and allowing extracellular fluid to escape.
This is the reason for the “runny nose” that is characteristic of this phase of the infection.
If the virus spreads to the lower respiratory tract, the infection can cause severe shedding of bronchial and alveolar cells down to a single-cell–thick basal layer.
What is the primary cell affected by M. Tuberculosis?
Macrophages
What is hypoxemia ?
can result from an inadequate amount of O2 in the air, a disorder of the respiratory system, dysfunction of the neurologic system, or alterations in circulatory function.
What is an example of a short acting Beta 2 agonist
What is the MOA and adverse effects
albuterol
Fast onset of actionRapid bronchodilation
CNS stimulation (excitability)
Cardiovascular stimulation (tachycardia)
What are type I alveolar cells
The type I alveolar cells, also known as type I pneumocytes, are extremely thin squamous cells with a thin cytoplasm and flattened nucleus that occupy about 95% of the surface area of the alveoli. They are joined to one another and to other cells by occluding junctions.
How is community acquired pneumonia diagnosed?
It is defined as an infection that begins outside the hospital or is diagnosed within 48 hours after admission to the hospital in a person who has not resided in a long-term care facility for 14 days or more before admission
What is the leading cause of lung cancer?
Smoking accounts for 80% of cases.
What is this clinical manifestation and why?

Clubbing may also be evident in people with chronic obstructive pulmonary disease (COPD) because there is long-term hypoxia. This is readily seen during a peripheral cardiovascular inspection when the provider assesses peripheral oxygenation/perfusion since the angle of the nail is 180 degrees or greater
what patient education is needed for corticosteroids?
Patient Teaching & Education
Patients should be advised that corticosteroids are not used to treat an acute asthma attack. They can cause immunosuppression and suppress signs of infection. Corticosteroids can also cause an increase in blood glucose levels. Patients may experience weight gain, swelling, increased fatigue, bruising, and behavioral changes. These occurrences should be reported to one’s healthcare provider.[6]
What are Type II alveolar cells
The type II alveolar cells, also called type II pneumocytes, are small cuboidal cells located at the corners of the alveoli. Type II cells are as numerous as type I cells, but because of their different shape, they cover only about 5% of the alveolar surface area. The type II cells synthesize pulmonary surfactant, a substance that decreases the surface tension in the alveoli and allows
What occurs during the first stage of pneumococcal pneumonia?
the alveoli become filled with a protein-rich edema fluid containing numerous organisms (Fig. 30-6). Marked capillary congestion follows, leading to massive outpouring of polymorphonuclear leukocytes and red blood cells.
Referred to as the red hepatization stage
What the four categories lung cancer is divided into?
squamous cell lung carcinoma (25% to 40%),
adenocarcinoma (20% to 40%),
small cell carcinoma (20% to 25%),
large cell carcinoma (10% to 15%)
Name the types of pleural effusions?
a transudate or exudate, purulent (containing pus), chyle, or sanguineous (bloody)
What is the class and adverse effect of Monteleukast ?
Montelukast can cause headache, cough, nasal congestion, nausea, and hepatotoxicity
Mechanism of Action
Montelukast blocks leukotriene receptors and decreases inflammation.
Indications for Use
Montelukast is used for the long-term control of asthma and for decreasing the frequency of asthma attacks. It is also indicated for exercise-induced bronchospasm and allergic rhinitis.
Nursing Considerations Across the Lifespan
The medication is safe for children 12 months and older. It is available in granule packets and chewable tablets, as well as regular tablets.
A client with a cough has been prescribed 400 mg of benzonatate daily by a physician. The on-hand availability of benzonatate is a 100 mg softgel capsule. How many capsules will the nurse have to administer to the client daily?
4 capsules
What are the clinical manifestations of a pleural effusion?
Fluid in the pleural cavity acts as a space-occupying mass; it causes a decrease in lung expansion on the affected side that is proportional to the amount of fluid collected. Characteristic signs of pleural effusion are dullness or flatness to percussion and diminished breath sounds. Hypoxemia may occur due to the decreased surface area and is usually corrected with supplemental oxygen. Dyspnea, the most common symptom, occurs when fluid compresses the lung, resulting in increased effort or rate of breathing. Pleuritic pain usually occurs only when inflammation is present.
The nurse is caring for a client who is scheduled to receive acetylcysteine. The nurse should notify the primary health care provider before administering the medication if the client has which conditions?
bronchospasm
The nurse is visiting a female client in her home for treatment of a wound. The client is concerned that her husband, a truck driver, is bothered by his seasonal allergies. What is the mechanism of action and adverse events associated withdiphenahydramine
blocks histamine
Adverse effects: sedation and drowsiness
identify the respiratory abnormality in the CXR on the right?
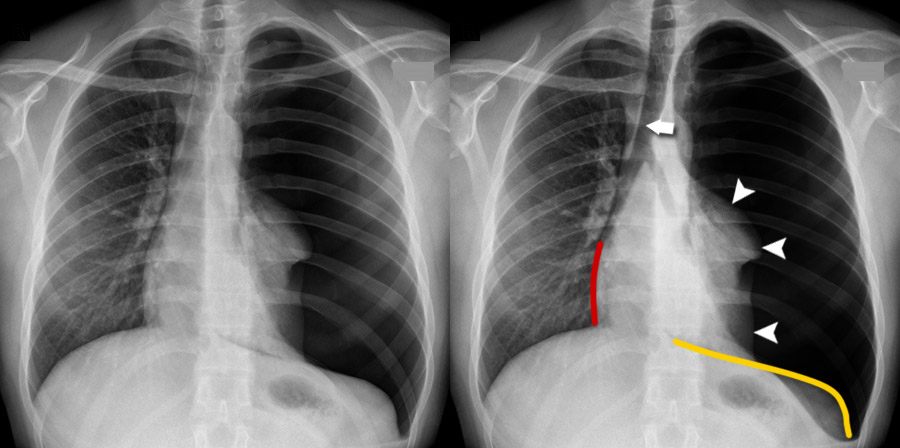
Tension Pneumothorax
the structures in the mediastinal space shift toward the opposite side of the chest
A client prescribed a second-generation H1 receptor antagonist asks what advantage this class of medication has over the first-generation H1 receptor antagonists in managing their allergic rhinitis
faster action
fewer adverse effects such as drowsiness
incomplete expansion of a lung or portion of a lung. It can be caused by airway obstruction, lung compression such as occurs in pneumothorax or pleural effusion, or increased recoil of the lung due to loss of pulmonary surfactant. The disorder may be present at birth (i.e., primary atelectasis) or develop during the neonatal period or later in life (i.e., acquired or secondary atelectasis).
A client prescribed nasal pseudoephedrine has received medication education. What response by the client suggests the nurse needs to provide follow-up information regarding the medication?
It will take about an hour for me to get any relief after taking pseudoephedrine.
What are symptoms of labored breathing?
Shortness of breath
Diaphoresis
Pursed-lip breathing
Tachypnea or bradypnea/irregular breathing rhythm Use of accessory muscles
Tachycardia
Abdominal breathing
Cyanosis