What part of the heart's conduction system is delayed or blocked in an AV block?
The AV junction (area around the AV node / bundle of His)
On an EKG, what is the large, wide complex beat that comes earlier than expected
Premature ventricular contraction (PVC): early, wide QRS with no preceding P wave (or retrograde P), compensatory pause.
From where in the heart does a junctional rhythm originate?
The AV junction (area around the AV node / bundle of His).
 What is the rate of this EKG?
What is the rate of this EKG?
Rate - about 100 bpm
Identify the AV block type when every P wave is followed by a QRS but PR intervals are consistently prolonged.
First-degree AV block (prolonged PR interval, >0.20 seconds0.20 seconds, but every P followed by QRS).
What are two EKG features that help you recognize ventricular tachycardia?
run of wide QRS complexes at rapid rate (often >100 bpm100 bpm), monomorphic or polymorphic, dissociated or absent P waves.
What happens to the P wave when a rhythm is junctional and impulses travel retrograde?
P waves may be absent, inverted in leads II/III/aVF, or occur before/within/after the QRS depending on timing (retrograde atrial activation).
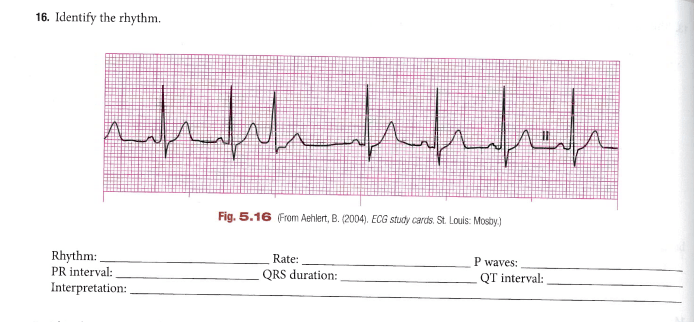
What do you notice about the P waves of this EKG?
They are upright - 1 QRS is missing a p wave. (PJC)
Which AV block shows progressively lengthening PR intervals until a beat (QRS) is dropped? (Longer, Longer, Longer...drop, then you have a ...)
Second-degree Mobitz type I (Wenckebach): progressive PR lengthening then dropped QRS.
Define ventricular fibrillation and describe why it is immediately dangerous.
Ventricular fibrillation: chaotic, disorganized electrical activity with no effective QRS complexes or pulse; immediately life‑threatening because there is no coordinated ventricular contraction and no cardiac output.
Name two reasons a junctional escape rhythm might appear (physiologic or pharmacologic).
Causes: sinus node dysfunction (sinus arrest), enhanced AV nodal automaticity, medication effects (digitalis toxicity, beta blockers, calcium channel blockers), ischemia affecting the sinus node.
 What is the rate of this EKG? Also, what do you notice about the P waves?
What is the rate of this EKG? Also, what do you notice about the P waves?
P waves are inverted. Rate is above 100 bpm
Describe the ECG finding for a complete (third-degree) AV block.
Third-degree (complete) AV block: atria and ventricles beat independently; P waves and QRS complexes have no relationship, and ventricular rate is usually slow (escape rhythm).
What key difference on an EKG distinguishes idioventricular rhythm (accelerated idioventricular rhythm) from ventricular tachycardia?
Idioventricular rhythm (IVR) usually has a slower regular wide QRS escape rate (commonly 40–100 bpm40–100 bpm for accelerated IVR) and lacks the fast rate and reentry features of VT; VT usually faster and more sustained.
How would you differentiate a junctional rhythm from a sinus rhythm on the EKG when heart rate is normal?
Junctional rhythm often has absent/inverted P waves or P waves that occur after QRS and a narrow QRS; sinus rhythm has upright P waves before each QRS with normal PR interval. Look for P-wave morphology/timing.
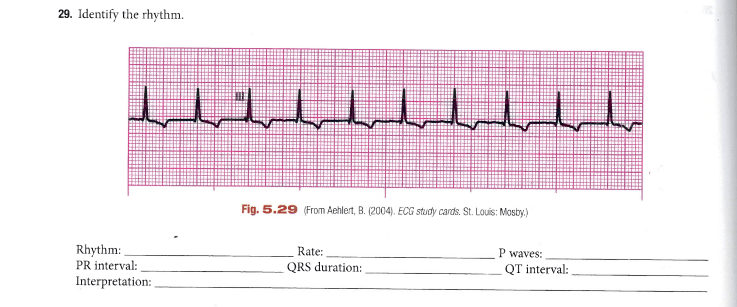
What do you notice about the QRS complexes in this EKG strip?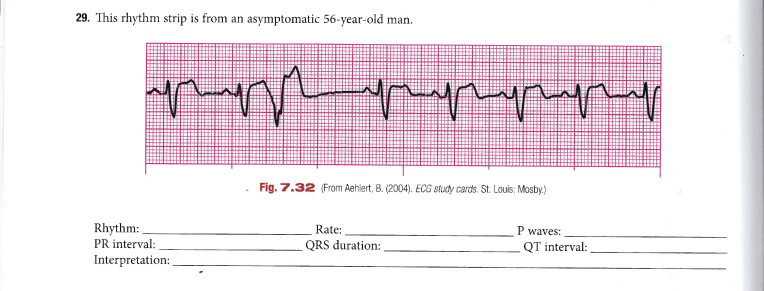
One of the QRS complexes is early and wide (Ventricular). Premature Ventricular Contraction
- Explain one potential clinical sign or symptom a patient might show with a high-degree AV block and why it occurs.
Symptoms: syncope, dizziness, fatigue, hypotension, or bradycardia-related fainting due to low cardiac output from slow ventricular rate or loss of atrial contribution to ventricular filling.
Describe how monomorphic and polymorphic ventricular tachycardia differ on the EKG
Monomorphic VT: QRS complexes look similar each beat (single focus). Polymorphic VT: QRS morphology varies beat to beat (multiple foci or changing conduction).
Describe the EKG appearance and likely clinical significance of accelerated junctional rhythm compared to a junctional escape rhythm.
Accelerated junctional rhythm: junctional rate faster than typical escape (commonly 60–100 bpm60–100 bpm or up to 100 bpm100 bpm) with junctional morphology; clinically may cause palpitations or indicate increased automaticity (e.g., digitalis effect, ischemia) compared to slower junctional escape which is compensatory for sinus failure.

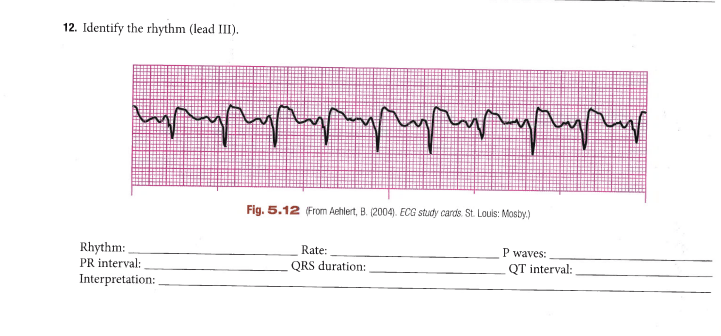
What do you notice about the orientation of the QRS and T waves? What do you notice about the rate towards the end of the EKG strip?
The QRS and T waves are in opposing directions. The rate increases at the end of the strip (VT)