How would you classify this wound?
Deep tissue injury
How long does the intermediate status of a cystectomy and diversion patient last?
Until 7pm POD1
How frequently must telemetry box batteries be changed?
Every shift, prior to shift change (6a/6p)
Which of the following creatinine levels would make you question your patient's kidney function?
A. 1.0 mg/dL
B. 0.98 mg/dL
C. 4.23 mg/dL
D. 0.64 mg/dL
4.23 mg/dL
Which of the following is NOT considered a symptom of a UTI for a patient WITHOUT an IUC?
A. Retention
B. Dysuria
C. Frequency
D. Urgency
Retention
True or False: A urostomy pouch is appropriate for use on a high output ostomy.
False!
What stage would you classify this wound?
Unstageable
What is the frequency of measuring intake and output for the cystectomy and diversion IBED?
Q2 hours urine output
Q4 hours for remaining I/Os
What is the rhythm disturbance noted in this telemetry monitoring?
Premature Ventricular Contraction (PVC)
Your patient's lab results show a magnesium of 1.6 mEq/L. What intervention would you anticipate for your patient?
IV magnesium repletion
Which of the following is the correct indication to chart for the continuation of an IUC on a colorectal patient who is awaiting a VCUG?
A. IUC to be removed
B. provider driven
C. acute urinary retention
D. routine Post-Op care
B. provider driven
How frequently should patient's ostomy appliances be changed?
Every 4 days
Primary responsibility of the nurse! Please make sure to check orders for if your patient has been signed off by our WOCN team.
How would you classify this wound?
Moisture Associated Skin Damage
What is the frequency of vital signs for a cystectomy and diversion during IBED status?
Vitals - Q2
Temperature - Q4
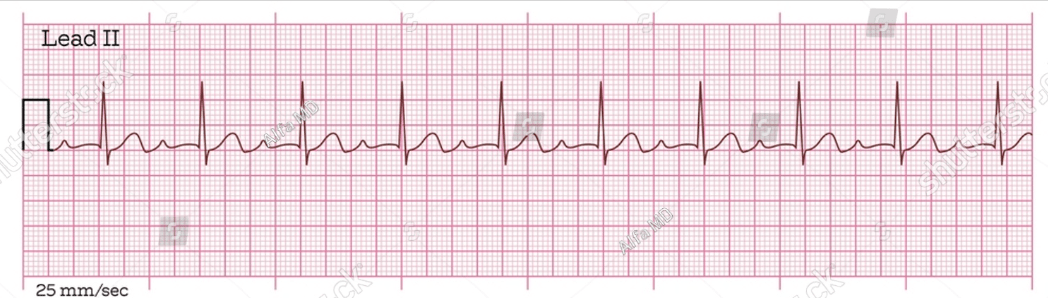
Identify the rhythm shown below.

Atrial Fibrillation
If this was a new patient finding, what would be the nurses next course of action?
Your patient's potassium results on their AM labs at 6.2 mEq/L. After notifying the provider, what is the primary response of the bedside nurse and why?
Obtain EKG to assess for cardiac dysrhythmias
Your patient had an IUC placed preoperatively 2 days ago. When emptying the urine bag, you notice the urine is cloudy and has a foul odor What is your next step?
Continue to monitor for additional symptoms
What ostomy accessory is most likely to resolve leakage problems?
An ostomy belt!
How would you classify this wound assessment?

Stage 2: Shallow open ulcer with pink/red wound bed or intact/open serum filled blister
What is the appropriate range of colostomy/ileostomy output per day?
500-1500ml/day
What abnormality in this strip, if newly onset, would necessitate further investigation?
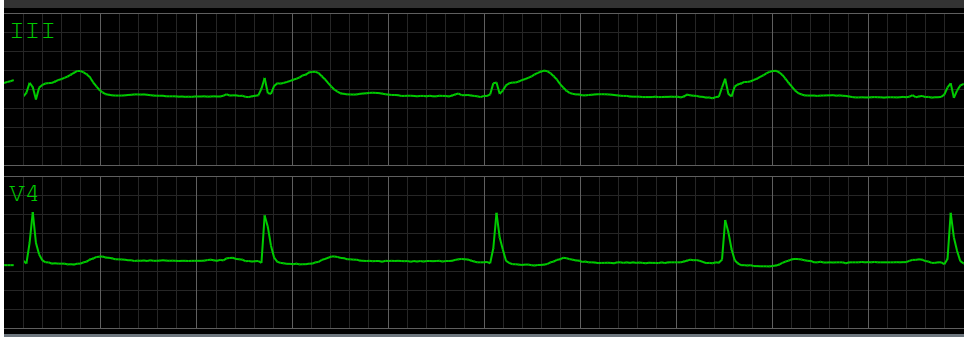
ST elevation
If this was a new patient finding, what would be the nurses next course of action?
What is considered to be the ideal potassium and magnesium value for the colorectal and urology surgical population?
Potassium - 4.0 mEq/L
Magnesium - 2.0 mEq/L
How frequently should you perform an intermittent catheterization on a patient prior to placing/replacing a foley in the instance of retention?
How long should the foley be kept in once replaced?
48hrs....TIME BASED!!
Foley should be maintained another 24hrs and then another void trial should be completed
What kind of patient may benefit from a convex stoma wafer?
Patient's whose stomas are located in creases, folds, or craters
What type of wound would you use honey gel to treat?
Open nonsurgical wounds (shallow and deep)
If you were told in report that your patient was POD1 from a LAR with a DLI, what procedure would this patient have undergone?
low anterior resection (LAR) with a diverting loop ileostomy (DLI)
Your patient's EKG shows the rhythm below. Upon measuring the waveform, you notice the PR interval is 0.20s. What rhythm would you document this patient to be in?
1st degree heart block
What is the rationale behind treating a patient's hyperkalemia with dextrose and insulin?
Drive potassium back into the patient's cells
DAILY DOUBLE - Case Study:
You are receiving report at 7am and are told that your post-op day 3 laparoscopic colectomy has a foley. When reviewing the patient's orders before starting med pass, you notice that the foley is provider driven with an indication of routine post-op care. What might be the next appropriate step by the nurse?
Reach out to the provider to question the maintenance of the foley/if it can be removed.
If the provider states that there is a clinical reason (i.e. VCUG) to maintain the foley, please request they change the ordered indication to best match the provided reasons.
What kind of patient would benefit from the use of stoma powder under their appliance wafer?
Patients with moist, red denuded skin under appliance.