What is the general pathophysiology of calcipenic rickets?
Low vitamin D --> Low Ca+2 --> Defective osteoid mineralization
What is this?

Rachitic Rosary
What is Genu Varum?
Bow legged
What is the prognosis of Rickets?
Normal life with excellent outcomes if caught and treated with typical recovery being within weeks to months. If left untreated can lead to long-term bone deformities and impaired growth
Which team scored the most points ever in a single Super Bowl?
The San Francisco 49ers (55 points in 1990)
How does osteoid mineralization occur?
- Osteoid formation: Osteoblasts secrete osteoid, composed primarily of type I collagen (about 94%) and ground substance.
- Preparation for mineralization: Matrix vesicles bud off from osteoblasts and accumulate calcium and phosphate ions. Alkaline phosphatase on the surface of matrix vesicles breaks down pyrophosphate, an inhibitor of mineralization.
- Initial mineral formation: Hydroxyapatite crystals begin to form inside the matrix vesicles.
- Crystal growth:The hydroxyapatite crystals grow and rupture the matrix vesicles, allowing them to spread into the surrounding osteoid.
- Mineral propagation:The initial crystals serve as nucleation sites for further crystal growth within the collagen fibrils of the osteoid.
- Continued mineralization: Osteoblasts continue to regulate the process by controlling local concentrations of calcium and phosphate, as well as producing proteins that promote or inhibit mineralization.
- Maturation: Over time, the mineral content increases, and the bone becomes fully mineralized.
Key factors influencing this process include:
- Adequate levels of calcium and phosphate
- Proper function of vitamin D to promote calcium absorption
- Appropriate balance of mineralization promoters (e.g., alkaline phosphatase) and inhibitors (e.g., pyrophosphate)
- Normal collagen structure to serve as a scaffold for mineral deposition
What is occurring here?

Epiphyseal cupping
What are risk factors for rickets?
Vitamin D deficiency (low sunlight exposure, dark skin, excessive breast feeding)
Living in norther latitudes
Mom having vitamin D deficiency during pregnancy, and/or premature birth
Medical conditions (celiac disease, IBS, CF, CKD)
Medications (certain anti-seizure and antiviral meds)
Inadequate calcium intake/absorption
Why are labs repeated in the management of rickets?
To monitor Treatment Efficacy, prevent Complications (like hypercalemia), guide Treatment Duration, assess Parathyroid Hormone (PTH) Levels, monitor Vitamin D Levels, detect Potential Renal Complications.
Lab tests are typically repeated every 3-4 weeks during the intensive phase of treatment and less frequently during the maintenance phase.
A clowder
Diagram the vitamin D pathway
*Scott and Albert cannot assist*

What are the differences between calcipenic rickets and hypophosphatemic rickets.
- Underlying cause:
- Calcipenic rickets: Primarily caused by vitamin D deficiency or impaired vitamin D metabolism/action.
- Hypophosphatemic rickets: Caused by renal phosphate wasting, often due to genetic defects or excess phosphatonins like FGF23.
- Serum calcium levels:
- Calcipenic rickets: Low or low-normal serum calcium.
- Hypophosphatemic rickets: Normal serum calcium.
- Serum phosphate levels:
- Calcipenic rickets: Low or low-normal phosphate, secondary to hyperparathyroidism.
- Hypophosphatemic rickets: Significantly low phosphate, primary defect.
- Parathyroid hormone (PTH) levels:
- Calcipenic rickets: Elevated PTH (secondary hyperparathyroidism).
- Hypophosphatemic rickets: Normal or mildly elevated PTH.
- Vitamin D metabolites:
- Calcipenic rickets: Low 25-hydroxyvitamin D; variable 1,25-dihydroxyvitamin D.
- Hypophosphatemic rickets: Normal 25-hydroxyvitamin D; normal or low 1,25-dihydroxyvitamin D.
- Calcipenic rickets: Primarily treated with vitamin D supplementation. Hypophosphatemic rickets: Treated with phosphate supplements and often calcitriol
What are the PE findings for a patient suspected to have Rickets?
Thickened wrists and ankles, bowed legs or knock knees, delayed closure of fontanelles, frontal bossing, craniotabes, rachitic rosary, muscle weakness, waddling gait
Why do breastfed infants need vitamin D supplementation?
Breast milk is low in vitamin D and can be even lower if mom has vitamin D deficiency. Infants are born with a natural vitamin D storage however can become depleted if not supplemented with diet, sunlight, and supplementation.
What is the team mascot in High School Musical?
Wildcats
Diagram the involvement of PTH, ALP, Phosphorus, and calcium in calcium regulation.
PTH is a key regulator of calcium homeostasis:
- Bone effects:
- Stimulates osteoclast activity, increasing bone resorption and releasing calcium into the bloodstream
- Kidney effects:
- Stimulates the production of 1,25-dihydroxyvitamin D (calcitriol)
ALP plays a crucial role in bone mineralization:
Hydrolyzes pyrophosphate: Pyrophosphate is an inhibitor of bone mineralization. By breaking down pyrophosphate, ALP promotes the formation of hydroxyapatite crystals
- Increases local phosphate concentration:
- ALP's enzymatic activity generates inorganic phosphate, which is necessary for bone mineralization
- Marker of bone turnover
Phosphorus is closely linked to calcium regulation:
- Forms hydroxyapatite with calcium
- Inverse relationship with calcium
- Regulated by PTH
- Affects vitamin D activation:
- Low phosphate levels stimulate 1α-hydroxylase, increasing the production of active vitamin D (calcitriol)
Calcium itself plays a role in its own regulation:
- Negative feedback on PTH:
- High serum calcium levels suppress PTH secretion
- Low serum calcium levels stimulate PTH secretion
- Affects vitamin D metabolism:
- Low calcium levels stimulate the production of calcitriol
- Bone mineralization:
- Serves as a primary component of hydroxyapatite crystals in bone
- Extracellular calcium sensing:
- Calcium-sensing receptors in the parathyroid glands and kidneys detect changes in serum calcium levels and modulate PTH secretion and calcium excretion accordingly
Explain why serum calcium levels are low-normal in calcipenic rickets.
- Compensatory mechanisms:
- As calcium levels start to drop, PTH secretion increases, which:
a) Enhances calcium reabsorption in the kidneys
b) Mobilizes calcium from bone stores
c) Stimulates production of 1,25-dihydroxyvitamin D to increase intestinal calcium absorption5
- As calcium levels start to drop, PTH secretion increases, which:
- Stage of disease:
- In early stages of vitamin D deficiency rickets, serum calcium is often maintained within the normal range.
- Hypocalcemia typically occurs only when skeletal calcium stores are severely depleted
- Type of rickets: In phosphopenic rickets, serum calcium and PTH levels are usually normal. Calcipenic rickets may have low or normal calcium levels, depending on the stage and severity
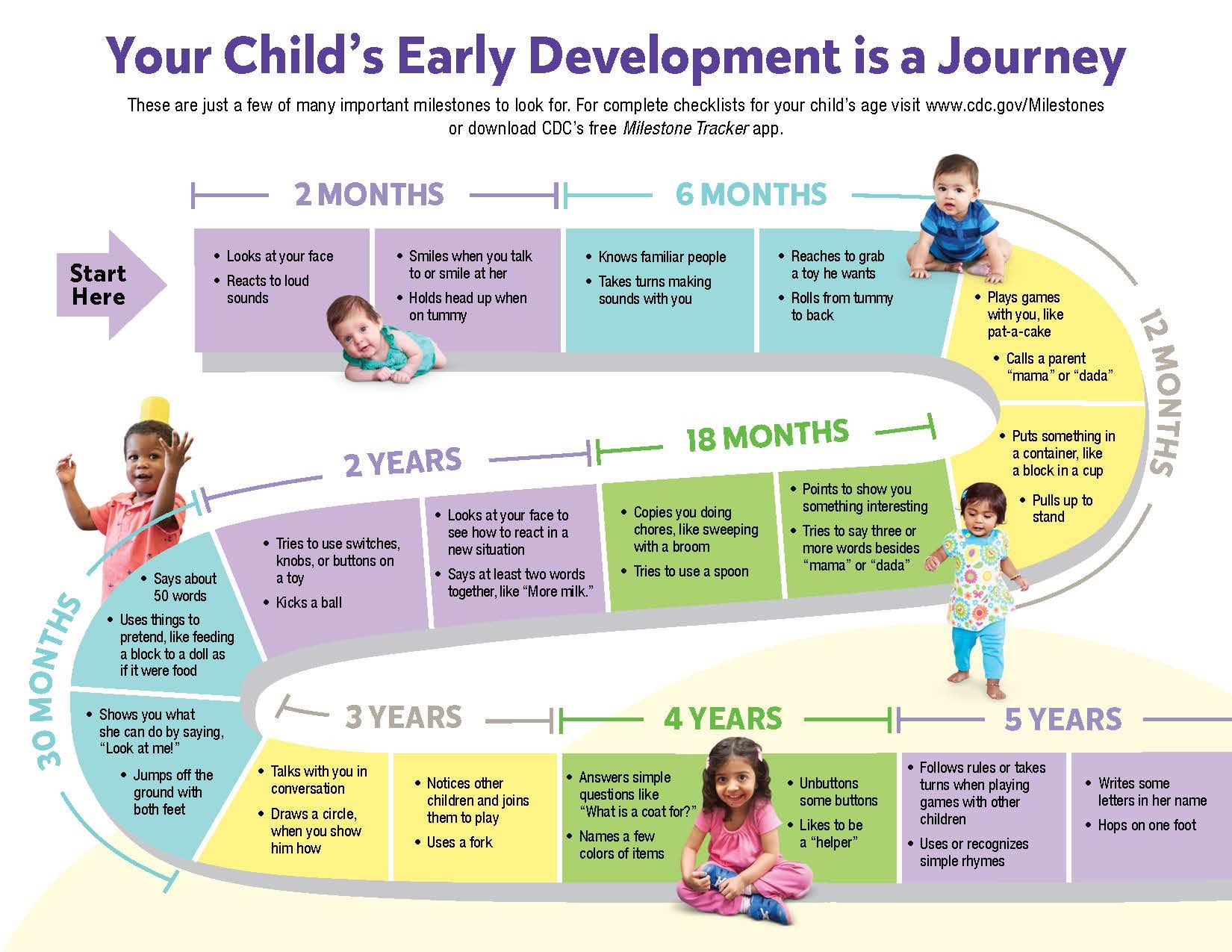
What are the developmental milestones for infants/children?
What is the treatment for calcipenic rickets?
- Vitamin D Supplementation:
- High-dose vitamin D (either D2 or D3) is administered, either by:
a) Daily dosing: 2000-6000 IU per day for 2-3 months
b) Stoss therapy: A single large dose of 100,000 to 600,000 IU, given orally or intramuscularly
- High-dose vitamin D (either D2 or D3) is administered, either by:
- Calcium Supplementation:
- Oral calcium supplements, usually 500 mg per day, are given in conjunction with vitamin D
- Crucial to prevent symptomatic hypocalcemia and ensure adequate bone mineralization
- Maintenance Therapy:
- After the initial treatment phase, patients are typically maintained on 400-600 IU of vitamin D daily
- Dietary Counseling:
- Patients and families are educated about vitamin D-rich foods and the importance of sunlight exposure
- Treatment Duration:
- The intensive phase usually lasts for 2-3 months, followed by a maintenance phase
What element has the highest atomic number that occurs naturally?
Uranium
What are the roles of vitamin D analogs in rickets?
25-Hydroxyvitamin D (25-OHD): 25-OHD is produced in the liver by hydroxylation of vitamin D, primarily by the enzyme CYP2R1 (25-hydroxylase)
Role in Calcipenic Rickets: Low serum 25-OHD levels are indicative of vitamin D deficiency rickets
Pathophysiological Implications: In calcipenic rickets, 25-OHD levels are typically low, indicating insufficient vitamin D intake or production, low 25-OHD leads to reduced substrate availability for the production of the active form, 1,25-OH2D.
1,25-Dihydroxyvitamin D (1,25-OH2D): 1,25-OH2D is produced in the kidneys from 25-OHD by the enzyme CYP27B1 (1α-hydroxylase)
Role in Calcipenic Rickets: 1,25-OH2D is the active form of vitamin D, crucial for calcium absorption and bone mineralization
Pathophysiological Implications: In calcipenic rickets, despite potentially normal or high 1,25-OH2D levels, there's insufficient total active vitamin D to maintain calcium homeostasis, the body attempts to compensate by increasing PTH, which stimulates 1α-hydroxylase to produce more 1,25-OH2D from the limited 25-OHD available
Why are ALP levels elevated in rickets?
- Increased osteoblast activity:
- Increased bone turnover and osteoblast activity as the body attempts to compensate for poor bone mineralization.
- Osteoblasts produce ALP, so increased osteoblast activity leads to higher ALP levels in the blood.
- Compensatory mechanism:
- ALP plays a crucial role in bone mineralization by hydrolyzing pyrophosphate, an inhibitor of mineralization.
- In rickets, where mineralization is impaired, the body increases ALP production as a compensatory mechanism to promote mineralization.
- Vitamin D deficiency:
- In nutritional rickets caused by vitamin D deficiency, low calcium levels stimulate parathyroid hormone (PTH) secretion.
- Elevated PTH further stimulates osteoblast activity and ALP production.
- Bone remodeling:
- Rickets causes softening and weakening of bones, leading to increased bone remodeling.
- This remodeling process involves heightened osteoblast activity, contributing to elevated ALP levels.
- Marker of disease severity:
- ALP levels often correlate with the severity of rickets, with higher levels indicating more severe disease.
- Age-related factors:
- In growing children, ALP levels are naturally higher due to bone growth.
- Rickets can exaggerate this elevation, particularly in infants and young children.
What are symptoms associated with calcipenic rickets?
- Bone pain and tenderness, especially in the spine, pelvis, and legs
- Delayed growth and development
- Muscle weakness and fatigue
- Skeletal deformities, such as:
- Bowed legs or knock knees
- Thickened wrists and ankles
- Curved spine
- Breastbone projection
- Softening of the skull (craniotabes)
- Dental problems:
- Delayed tooth eruption
- Weak tooth enamel
- Increased risk of cavities
Difficulty walking or waddling gait, Delayed motor skills development, Large forehead or frontal bossing, Widened joints, especially at wrists and ankles, Fragile bones that are prone to fractures, Seizures due to low calcium levels (severe), Poor growth, resulting in shorter than average height, Abnormally curved spine (scoliosis or kyphosis), Large abdomen, Late closure of the fontanelles (soft spots) in infants
Why is it recommended that calcium and vitamin D are taken together and how does it affect ALP?
- Improved bone mineralization: Vitamin D enhances calcium absorption in the intestines, while calcium supplementation provides the raw material needed for bone mineralization. As bone mineralization improves, the need for compensatory ALP production decreases.
- Reduction of secondary hyperparathyroidism: Vitamin D and calcium supplementation help normalize serum calcium levels, reducing PTH secretion and subsequently lowering ALP levels.
- Normalization of osteoblast activity: As calcium and vitamin D levels normalize, osteoblast activity returns to normal, reducing excessive ALP production.
- Correction of vitamin D deficiency: Vitamin D supplementation directly addresses the underlying cause of nutritional rickets. As vitamin D levels normalize, the overall bone metabolism improves, reducing the need for elevated ALP levels.
- Suppression of bone turnover: Calcium and vitamin D supplementation help reduce excessive bone turnover, leading to a decrease in ALP production.
- Improvement of phosphate metabolism: Vitamin D also helps normalize phosphate levels, which are often low in rickets. Improved calcium-phosphate balance contributes to better bone mineralization and reduced need for compensatory ALP production.
What city in South America is also known as "The Lost City of the Incas?"
Machu Picchu