This medication inhibits peripheral DOPA decarboxylase.
Carbidopa
This reduces peripheral conversion of levodopa to dopamine, decreasing GI side effects and increasing CNS availability.
A 62‑year‑old man presents with a 3‑year history of progressively worsening slowness, stiffness, and a right‑hand resting tremor. His wife reports years of vivid dream enactment with yelling and punching during sleep, as well as chronic constipation and loss of smell preceding his motor symptoms. On exam, he has cogwheel rigidity, bradykinesia, and hypomimia.
Which pathology is most characteristic of this condition?
A. Ballooned neurons and astrocytic plaques in the cortex
B. Globose neurofibrillary tangles in the brainstem
C. Alpha‑synuclein inclusions in the substantia nigra and locus coeruleus
D. Selective loss of GABAergic neurons in the caudate nucleus
E. Iron deposition in the globus pallidus with an “eye of the tiger” sign
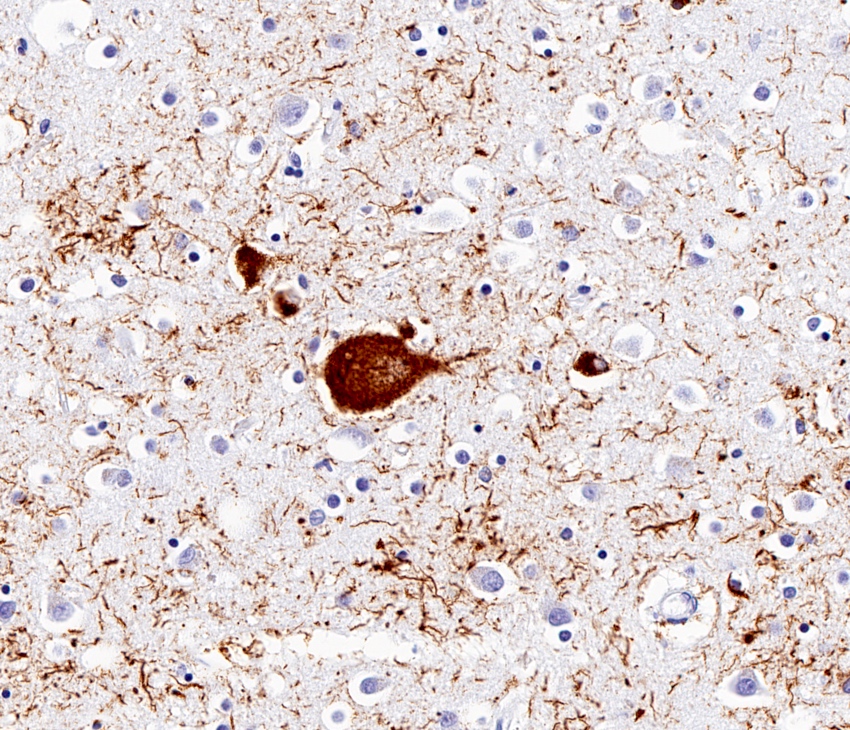
C. Alpha‑synuclein inclusions in the substantia nigra and locus coeruleus
This genetic mutation is the most common single-gene cause of early-onset Alzheimer’s disease, AND
This genetic mutation increases susceptibility to late-onset Alzheimer's Disease.
Early onset: Presenilin 1 (PSEN1) mutations are the most common cause of early-onset AD, autosomal dominant with 100% penetrance.
Late onset: APOE 4. This increases risk by 5-15 fold. Susceptibility gene found on chromosome 19. APOE 2 allele decreases the risk of AD.
Parkinson's Disease. Midbrain on left shows pale substantia nigra.
This disease has the following cardinal symptoms/signs: resting tremor, rigidity, bradykinesia, and postural instability
This medication is the only FDA-approved medication to treat PD-related psychosis.
Bonus points: What is its mechanism of action?
Pimavenserin.
5-HT2A receptor inverse agonist/antagonist
A 70‑year‑old woman presents with parkinsonism, frequent early falls, and difficulty looking down. Examination reveals impaired vertical gaze and poor smooth pursuit. MRI demonstrates midbrain atrophy with preservation of the pons. Her symptoms show minimal response to levodopa.
Which additional finding is most consistent with this diagnosis?
A. Visual hallucinations and occipital hypometabolism
B. Early limb apraxia with asymmetric cortical atrophy
C. Autonomic dysfunction with a “hot cross bun” sign
D. Tufted astrocytes with tau‑positive inclusions
E. Caudate atrophy with anticipation across generations
D. Tufted astrocytes with tau‑positive inclusions
A loss-of-function of frataxin gene leads to this disease.
Friedreich Ataxia (FA)
- Presents in teenage years with progressive ataxia, dysarthria/dysphagia, sensory loss due to axonal neuropathy, high-arched feet, and weakness with relatively intact cognition.
- Cardiomyopathy is the most common cause of death.
- Can be treated with the synthetic coenzyme Q analogue. idebenone.
- Genetics: Autosomal recessive. Due to a loss-of-function mutation of the frataxin (FXN) gene caused by a trinucleotide repeat of GAA (>66).
- Imaging: Atrophy of the cervical cord and medulla, with some minimal cerebellar atrophy
Identify the abnormality and associated disease

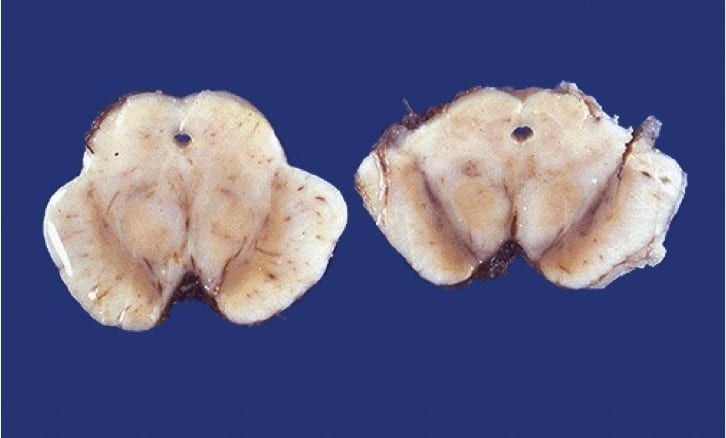
Bilateral caudate atrophy. Classic for Huntington's Disease.
DOUBLE JEOPARDY
Stiff Person Syndrome leads to increased tone of axial muscles, especially paraspinal muscles. In order to diagnose it, clinicians can order tests to identify the following antibodies.
Anti-glutamic acid decarboxylase (GAD) antibodies (anti-GAD65) and anti-amphiphysin antibodies
Anti-GAD65 can suggest an autoimmune etiology.
Anti-amphiphysin are associated with the paraneoplastic form.
DOUBLE JEOPARDY
Name 2 of the 3 FDA-approved for Parkinson’s disease–related dementia.
Rivastigmine, donepezil, galantamine.
- Rivastigmine: Acetylcholinesterase and butyrylcholinesterase antagonist
- Donepezil: Acetylcholinesterase inhibitor
- Galantamine: Acetylcholinesterase inhibitor and nicotinic modulator
A 16‑year‑old boy presents with sudden, brief episodes of dystonic posturing and choreoathetoid movements lasting less than one minute. Episodes are triggered when he stands up quickly or is startled. He sometimes feels a brief nonspecific warning just before attacks. Neurologic examination between episodes is normal.
Which is the most appropriate treatment?
A. Acetazolamide
B. Tetrabenazine
C. Carbamazepine
D. Botulinum toxin injections
E. Low‑dose levodopa
C. Carbamazepine. Others would be oxcarbazepine or phenytoin.
Paroxysmal Kinesigenic Dyskinesia (PKD) presents in adolescence with sudden brief (usually less than one minute) attacks of dystonia and/or choreoathetosis triggered by sudden movements, such as going from sitting to standing or being startled.
Some cases have PPRT2 mutation.
This is the number of trinucleotide repeats needed for full penetrance of Huntington's Disease. Include the trinucleotide name.
Trinucleotide repeats >40 CAG leads to full penetrance of the disease.
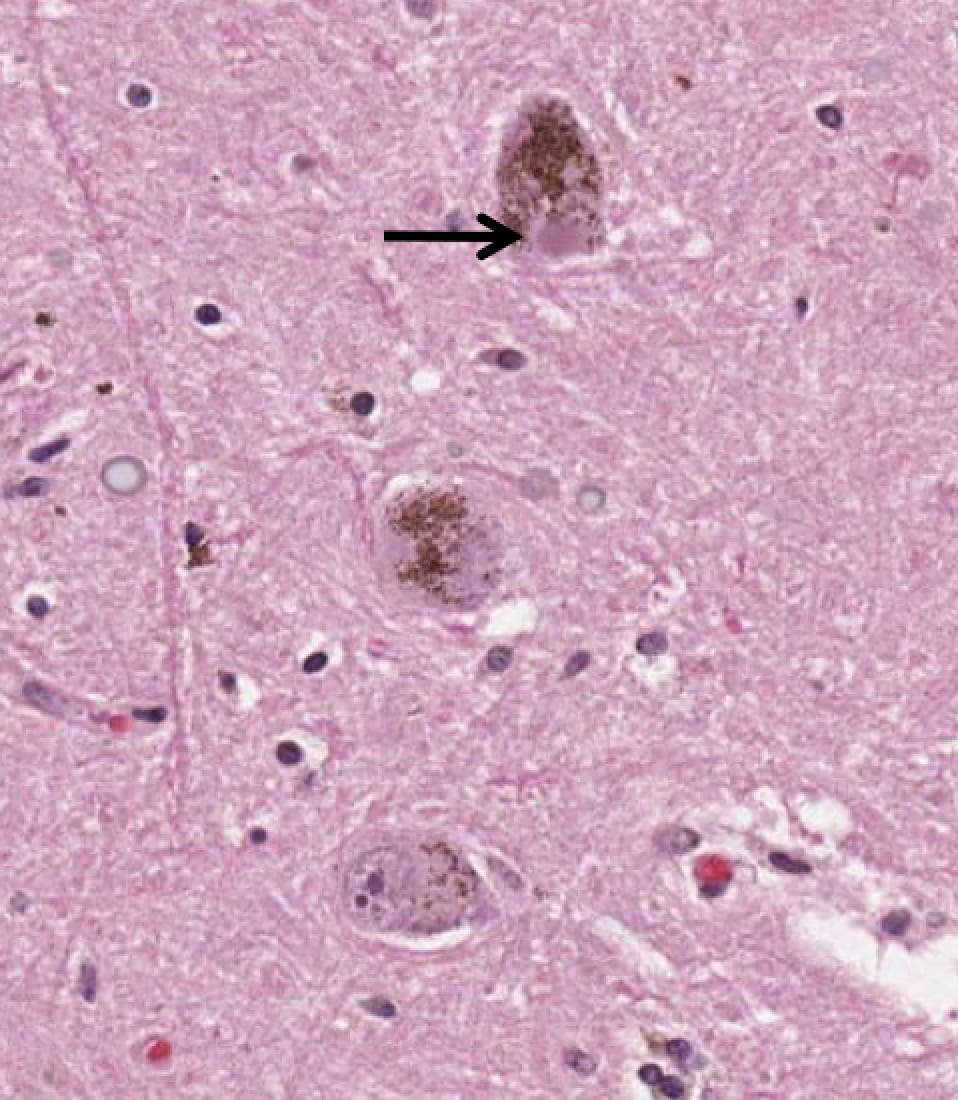
Lewy Body (alpha-synuclein inclusions), primarily seen in substantia nigra and locus coeruleus in Parkinson's Disease.
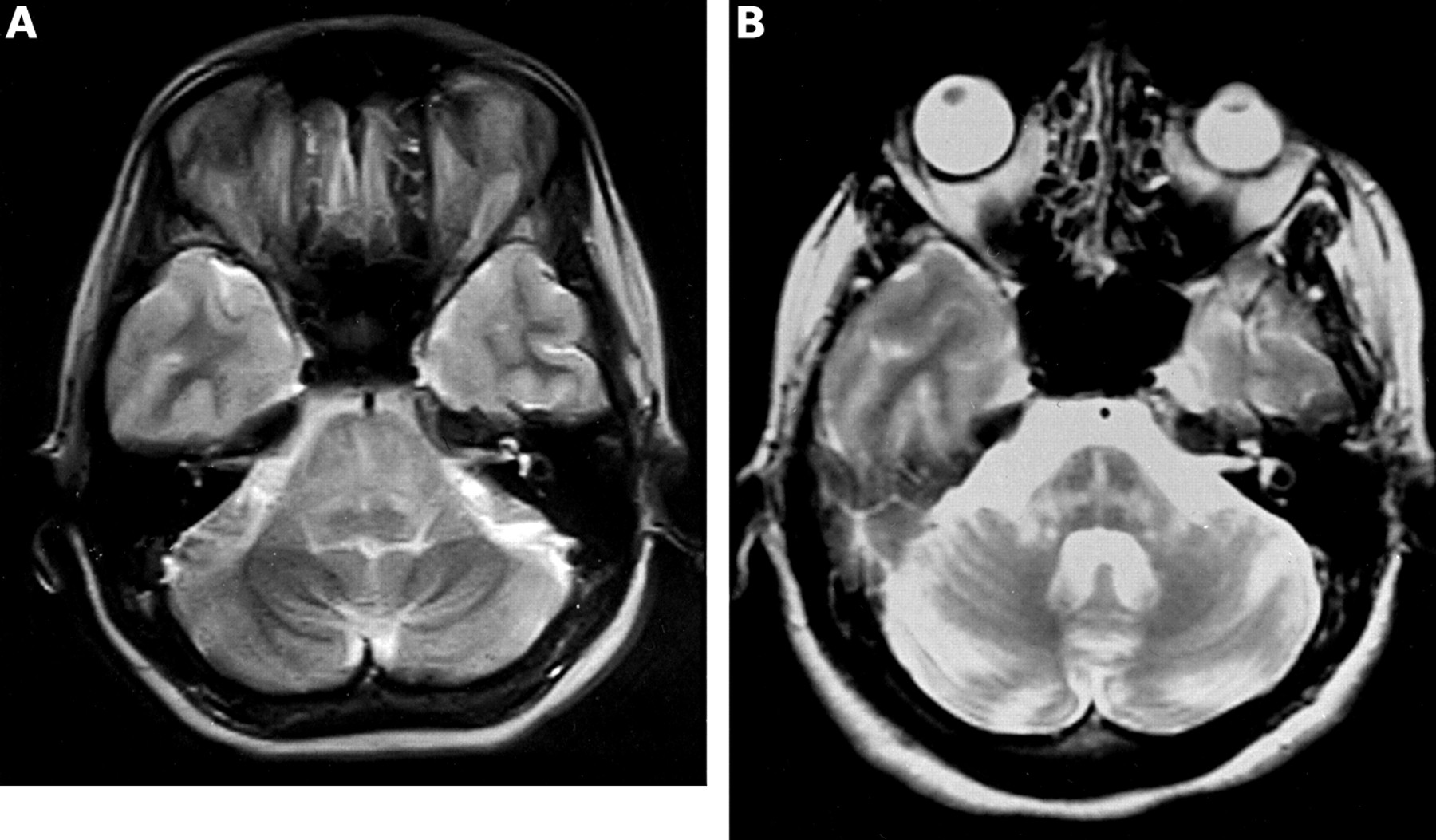
This is the name given to the imaging sign of degeneration and loss of pontine neurons and transverse pontocerebellar fibers.
(1) The name of the sign
(2) The associated disease
(1) Hot cross bun sign, (2) Multiple Systems Atrophy (usually MSA-C)
When given to a patient with Parkinson's, these class of medications are most strongly associated with impulse control disorders.
Direct dopamine agonists
- Bromocriptine, pramipexole, ropinirole, rotigotine, and apomorphine
These stimulate dopamine receptors (especially D3) in mesolimbic pathways, increasing risk of impulsive behaviors.
A 62-year-old woman presents with progressive difficulty finding words, frequent pauses in speech, and impaired repetition of long sentences, while her single-word comprehension and grammar remain intact. MRI shows left posterior temporal and inferior parietal atrophy. Which variant of primary progressive aphasia best fits this presentation?
A. Non-fluent/agrammatic variant
B. Semantic variant
C. Logopenic variant
D. Progressive apraxia of speech
C. Logopenic variant.
This variant is defined by word-finding pauses, impaired repetition of long sentences, and relatively preserved single-word comprehension and grammar, with atrophy in the left posterior temporal and inferior parietal regions.
The non-fluent/agrammatic variant features effortful speech and agrammatism, the semantic variant has impaired single-word comprehension and object knowledge, and progressive apraxia of speech is a motor speech disorder rather than a language disorder.
This gene is implicated in autosomal dominant frontotemporal dementia and ALS.
A. MAPT
B. PRNP
C. C9ORF72
D. FUS
E. ATP7B
C. C9ORF72
Note: MAPT mutations also associated with FTD, but not with ALS.
Identify the abnormality and associated disease.
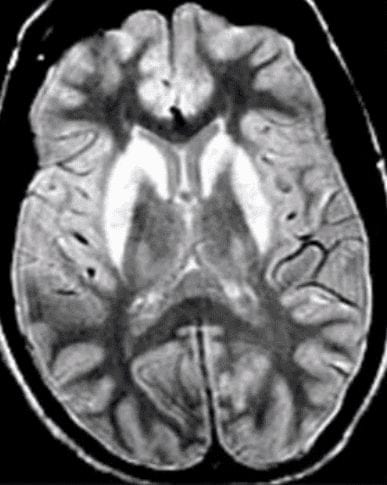
T2 hyperintensities in bilateral caudate and putamen. Seen in Wilson's Disease.
A 66‑year‑old man develops progressive difficulty using his left hand despite normal strength. He has trouble buttoning shirts and performing learned gestures with that limb. Exam shows asymmetric rigidity, limb apraxia, cortical sensory loss, and nonfluent speech. Levodopa provides no benefit.
FDG‑PET shows asymmetric hypometabolism involving the right perisylvian cortex. MRI demonstrates focal parietal atrophy.
Which pathological finding would be most expected at autopsy?
A. Flame‑shaped neurofibrillary tangles concentrated in the hippocampus
B. Globose neurofibrillary tangles with tufted astrocytes in the brainstem
C. Ballooned neurons and astrocytic plaques in the cortex
D. Round silver‑staining Pick bodies in bilateral anterior temporal lobes
E. Hyperphosphorylated tau concentrated within cortical sulci
C. Ballooned neurons and astrocytic plaques in the cortex
- These are hallmark features of corticobasal degeneration (CBD).
- Imaging shows asymmetric perisylvian hypometabolism and parietal atrophy, classic for CBD.
- The defining pathology of CBD is:
- Ballooned (achromatic) neurons
- Astrocytic plaques
For reference:
- A: Flame‑shaped tangles → Alzheimer’s disease.
- B: Globose tangles + tufted astrocytes → PSP.
- D: Pick bodies → FTLD‑tau (Pick’s disease).
- E: Tau in cortical sulci → chronic traumatic encephalopathy (CTE).
This is a VMAT2 inhibitor used to treat chorea
Tetrabenazine and deutetrabenazine.
Deutetrabenazine has a longer half-life and improved tolerability.
A 3-year-old girl presents with a 2-week history of chaotic multidirectional eye movements, myoclonic jerks of the limbs and trunk, and ataxia. She is irritable and has sleep disturbances. MRI of the brain is normal, and CSF analysis shows mild lymphocytic pleocytosis with normal protein and glucose. What is the most likely diagnosis, and which antibody is most commonly associated with this condition?
Opsoclonus-Myoclonus Syndrome.
Considered a paraneoplastic disorder secondary to neuroblastoma in children, and lung or gynecological cancers in adults.
- If suspected, the workup includes a pan CT scan (chest, abdomen, and pelvis) to evaluate for malignancy.
- Association with anti-Ri or anti-Hu antibodies.
- Symptoms often improve with treatment of the associated tumor.
DOUBLE JEOPARDY
SCN1A mutation is associated with which the following diseases?
A. Dravet Syndrome
B. Spinocerebellar ataxia Type 6
C. GLUT1 deficiency
D. Malignant Hyperthermia
E. Paramyotonia congenita
A. Dravet Syndrome
Remaining:
- Spinocerebellar ataxia Type 6 – CACNA1A
- GLUT1 deficiency – SLC2A1
- Malignant hyperthermia – RYR1
- Paramyotonia congenita – SCN4A
What disease is associated with the following pathology on silver stain?
A. Frontotemporal dementia
B. Alzheimer's disease
C. Lewy Body dementia
D. Progressive supranuclear palsy
E. Multiple systems atrophy
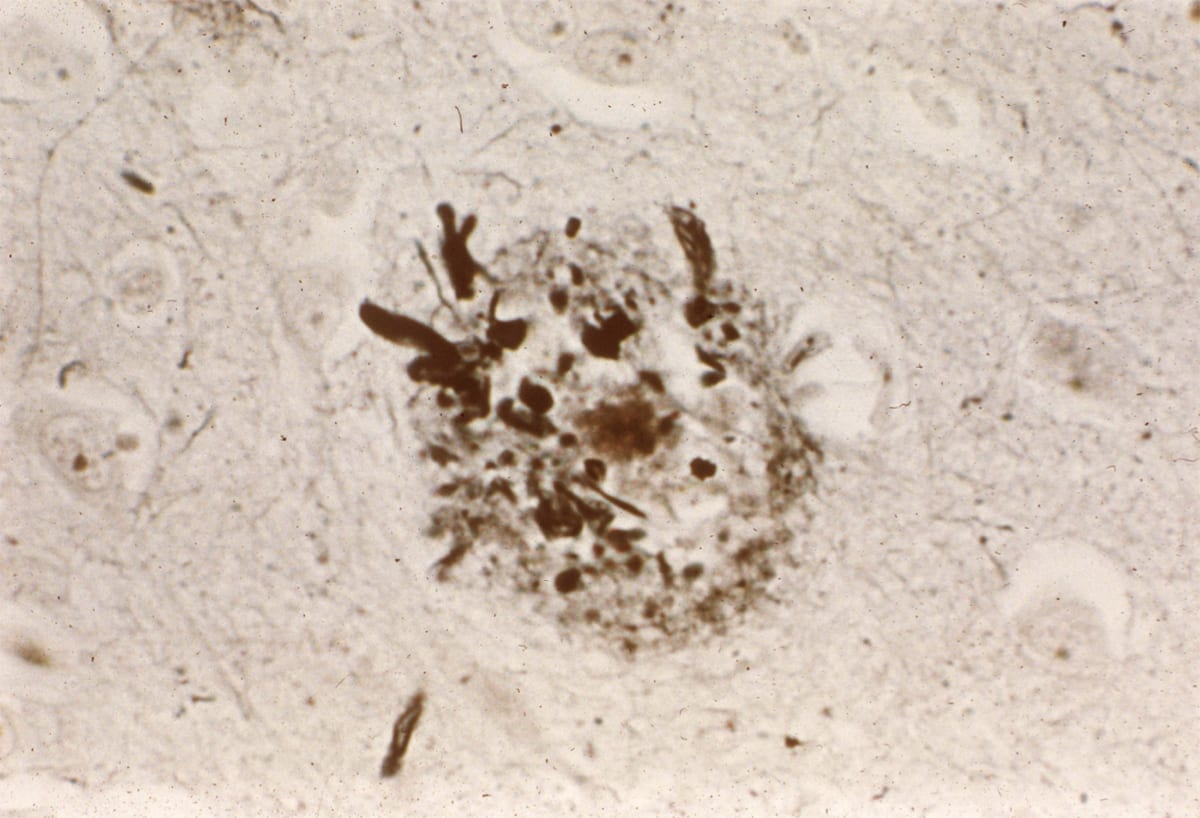
Alzheimer's Disease. Pathology shows amyloid neuritic plaque.
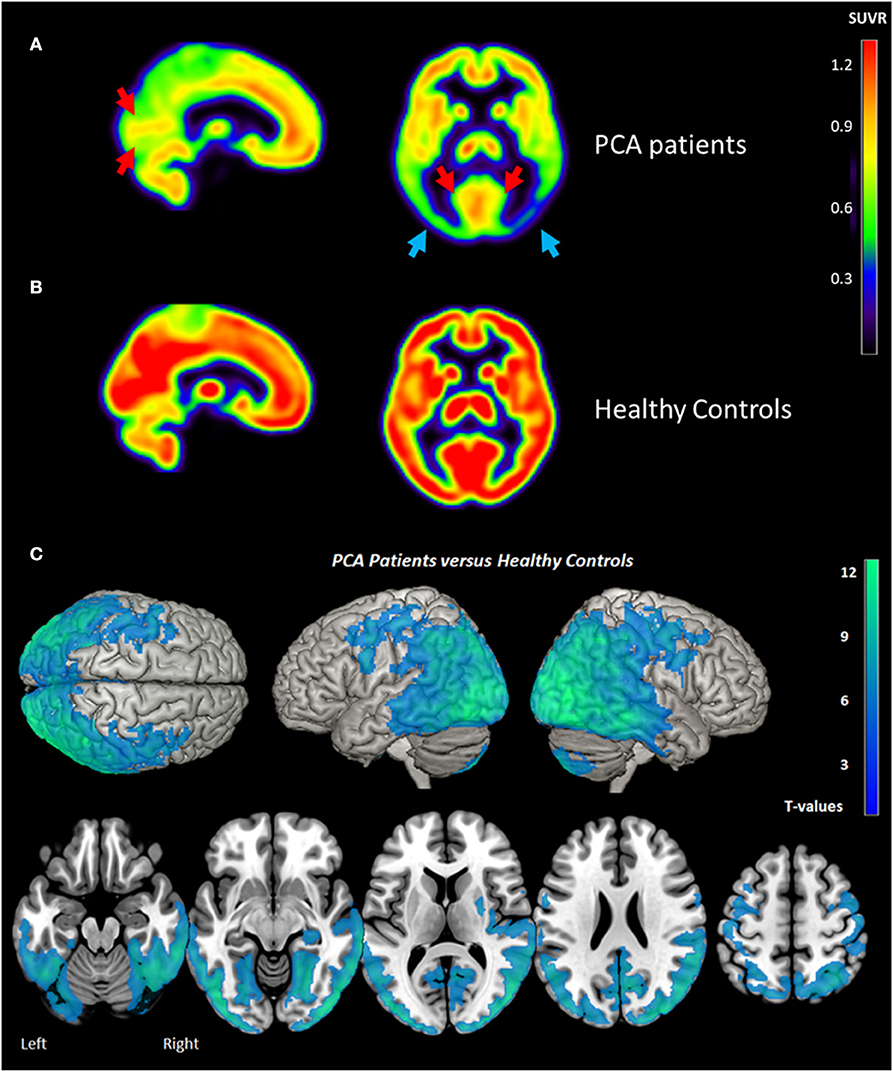
This dementia syndrome shows FDG‑PET hypometabolism predominantly in the parieto‑occipital cortices rather than the temporoparietal regions.
What is posterior cortical atrophy.
This is a visual variant of Alzheimer's disease. This pattern is distinct from typical Alzheimer's disease (temporoparietal and posterior cingulate hypometabolism), and from dementia with Lewy bodies (occipital hypometabolism with the cingulate island sign).