The 2 most common organisms that cause vascular graft infections.
Staph aureus (MC short term)
Staph Epidermidis (more indolent course)
- Coagulase-negative staphylococci such as S epidermidis can have a more indolent course as these bacteria are less virulent and aggressive.
- Infections from gram-negative bacteria such as Escherichia coli, Pseudomonas, Klebsiella, Enterobacter, Serratia, and Proteus usually occur early and are more severe. These infections can be prone to poor wound healing, anastomotic disruption, and hemorrhage. Systemic infections and subsequent seeding of grafts with these pathogens may have a prolonged course.
Fungal graft infections can occur, but they are much less common and typically limited to immunosuppressed patients. Candida albicans is the offending pathogen in most reported cases.
The anatomic defect that leads to a thoracic aortic dissection
Intimal tear
Most common cause of an AV graft thrombosis 1 year after creation?
Intimal hyperplasia
Late access thrombosis usually occurs 1 to 2 years after access placement and most commonly is due to intimal hyperplasia. In a prosthetic access, this occurs most commonly at the graft-venous anastomosis.
This structure lies between the subclavian vein and anterior scalene
phrenic nerve
This arterial disorder
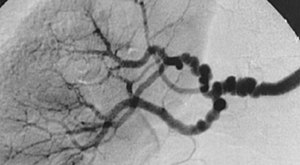
Fibromuscular dyplasia
Fibromuscular dysplasia (FMD) is a non-atherosclerotic, non-inflammatory arterial disease that primarily affects women. 1. It most commonly affects the renal, extra-cranial carotid, and vertebral arteries, but has been reported in almost every arterial bed
Name 2 perioperative risk factors for vascular graft infection
Perioperative risk factors:
Prolonged preoperative hospitalization
Infection in a remote site
Recent percutaneous arterial access at the implant site (peripheral or cardiac angiography)
Breaks in aseptic technique
Emergency/urgent operation
Reoperative vascular procedure
Extended operating time
Concomitant gastrointestinal or genitourinary procedure
Postoperative wound complication (superficial infection, skin necrosis, lymphocele)
Patient-related risk factors:
Malignancy
Lymphoproliferative disorder
Autoimmune disease
Corticosteroid administration
Chemotherapy
Malnutrition
Diabetes mellitus
Chronic renal insufficiency/end-stage renal disease
Liver disease or cirrhosis
Name 2 genetic syndromes that can make one high risk for aortic dissections.
Syndromic conditions commonly associated with a risk of aortic dissection include Marfan, Loeys-Dietz, and Ehlers-Danlos syndromes.
Classic initial symptom of an aortic graft-enteric fistula
Herald bleed (classically hematemasis)
EGD is the first diagnostic evaluation for an upper GI hemorrhage. With a history of an aortic graft, a high index of suspicion should prompt extension of the endoscopic evaluation to the distal duodenum to make the diagnosis and rule out other etiologies.
Name this neonatal brachial plexus injury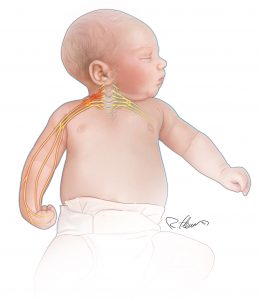
Erb-duchenne palsy (Erb's palsy)
This artery

Left anterior tibial artery
MC material used for dialysis AV grafts
Polytetrafluoroethylene (PTFE)
PTFE grafts are preferred over biological and other synthetic grafts due to low thrombosis risk, longer patency, ease of implantation, and low risk of disintegration with infection.
The Blood vessel that provides a critical collateral pathway for intestinal perfusion when the superior mesenteric artery is occluded
Pancreaticoduodenal artery
The mesenteric collateral circulation network is robust, explaining why most patients develop symptoms only when at least two of the tree arteries are severely narrowed. This is not an absolute requirement, and some patients develop symptoms with single-vessel disease. The pancreaticoduodenal artery provides a vital collateral pathway between the celiac artery and the superior mesenteric artery.
The anatomic location where most AAA grafts fistulize
Common aortoenteric fistulas involve the third or fourth part of the duodenum (D3/D4).
Surgical treatment for patients with neurogenic thoracic outlet syndrome who fail conservative mangement.
First rib resection
This is considered for patients that fail conservative approaches with physical therapy. Injection of botulinum toxin is a relatively new treatment and can allow patients to get additional benefit from physical therapy and provide relief to symptoms. This is not an initial treatment, however, and when performed, should be done under image guidance by experienced practitioners.
Typical dosing per kg of systemic heparin when occluding a vessel
80-100 U/kg
The surgical maneuver required to gain access to the infrarenal aorta
Maddox Maneuver

Retrograde filling of an aortic aneurysm sac by lumbar branches or by the inferior mesenteric artery
Type II endoleak (most common type)
Type II endoleak, the most common type, is characterized by retrograde filling of the aneurysm sac by lumbar branches or by the inferior mesenteric artery.
Type I endoleak is due to failure to achieve satisfactory seal at proximal zone (type Ia) or distal zone (type Ib).
Type III endoleak is due to failure of an individual component or of seal between components of graft system, preventing exclusion of the aneurysm sac.
Type IV endoleak is caused by leakage through porous materials of the graft.
Type V endoleak is due to persistent growth of the aneurysm sac without detectable leak (endotension).
The ideal initial location for an AV fistula creation in a left handed patient.
Right radiocephalic fistula (cimino fistula)
During a first rib resection for TOS, the resident accidentally transects the phrenic nerve. This complication most likely manifest as this.
Hemi-diaphragmatic paralysis/dysfunction
The half-life of heparin
60-90 minutes
The extra-anatomic procedure to perform in a patient with occlusive aortoiliac disease who is a poor surgical candidate.
Axillo-bifemoral bypass

Primary treatment for a type B thoracic aortic dissection
The mainstay of medical therapy for acute type B dissection is beta blockade with short-acting agents, such as esmolol, in an ICU.
Initial surgical intervention for a bleeding aortic-enteric fistula in an unstable patient.
Endovascular therapy with stent graft placement across the fistula
This offers a bridging therapy for hemodynamically unstable patients prior to their definite procedure.
The syndrome associated with axillary-subclavian vein thrombosis associated with strenuous and repetitive activity of the upper extremities.
Paget-Schroetter Syndrome, refers to axillary-subclavian vein thrombosis associated with strenuous and repetitive activity of the upper extremities.
On the first postoperative day after endovascular repair for a ruptured abdominal aortic aneurysm, a patient develops increased abdominal pain and tenderness, as well as hematochezia. Your next step is this.
Flexible sigmoidoscopy
Colonic ischemia has been shown in up to 23% of patients after ruptured abdominal aortic aneurysm (AAA). Therefore, it is recommended that patients undergoing endovascular repair for ruptured AAA have a postoperative flexible sigmoidoscopy to assess for colonic ischemia. If a patient shows signs of possible colonic ischemia such as hemodynamic compromise, hematochezia, abdominal pain or tenderness, and/or leukocytosis, sigmoidoscopy should be performed urgently to determine the next step in management.