Coloring, helping, cognitive questions, taking walks, etc
Name this move!
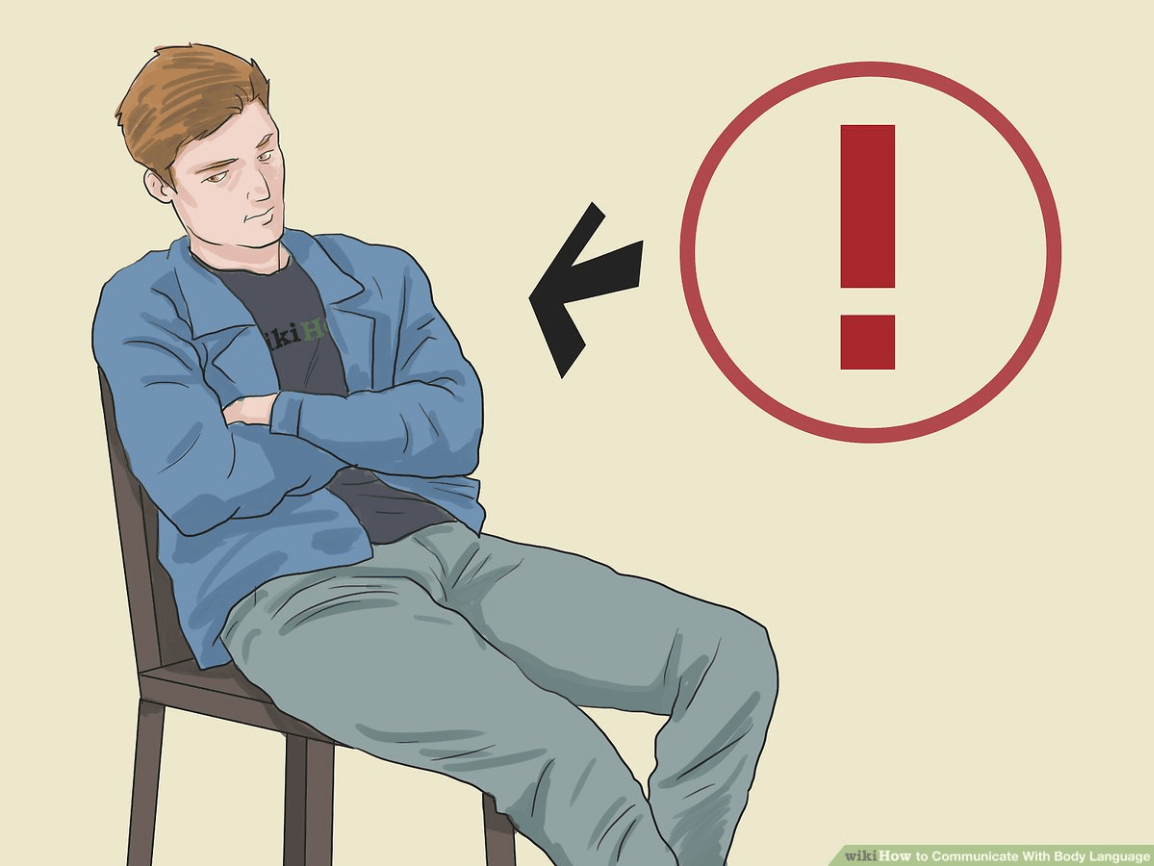
Protective Stance
Youth is threatening another youth with a knife; restrain or don't restrain?
NO - they have a weapon
Name 3 potential triggers in a hospital setting
Examples: parent leaving, having to be admitted, having phone taken, not going outside, etc.
Share one of your go-to positive self-talk thoughts when faced with a crisis
Examples: "They are in crisis, I just happen to be in the way," "I've got this," or "This is just temporary."
True or false: it is often helpful to utilize physical touch and close proximity when a patient is angry/agitated
FALSE
What is the LSI acronym we use to remember the steps?
I-ESCAPE
Anything that makes challenging behavior more or less likely to occur is called a...?
Setting Condition
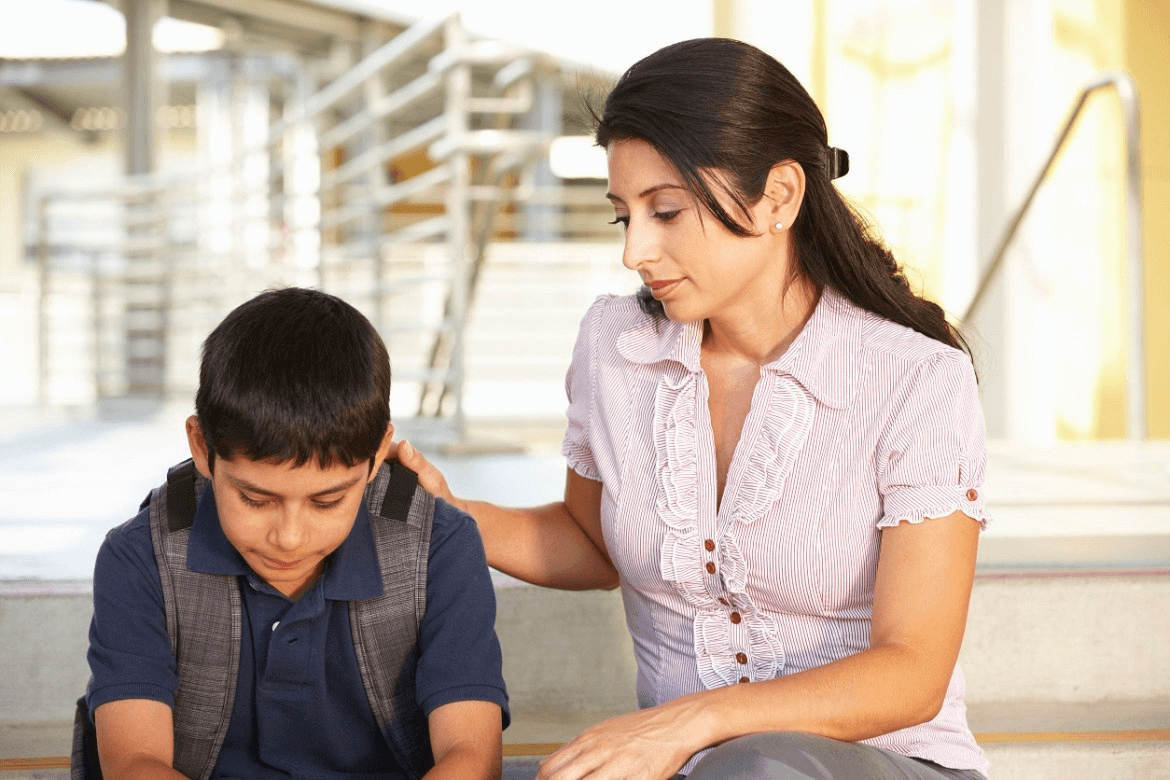
Name this Behavior Support Technique!
Caring Gesture
Physical restraints are NOT used to... (name 2)
Demonstrate authority, enforce compliance, inflict pain or harm, punish or discipline
What are 3 warning signs of Asphyxia?
Examples: Going limp, saying they can't breathe, vomiting, making grunting noises, turning dusky purple, respiration is labored.
List the 5 stages of the Stress Model of Crisis
Basline, Triggering Event, Escalation Phase, Outburts/crisis, and Recovery
Label this
Stressful event, youth feelings, youth behavior, adult's response
 What might this patient be thinking/feeling?
What might this patient be thinking/feeling?
"You feel disappointed when plans are cancelled" is an example of what?
Reflective Response
The "three R's" of Emotional First Aid stand for what?
Reduce stress; resolve the immediate crisis; remain in the program/activity
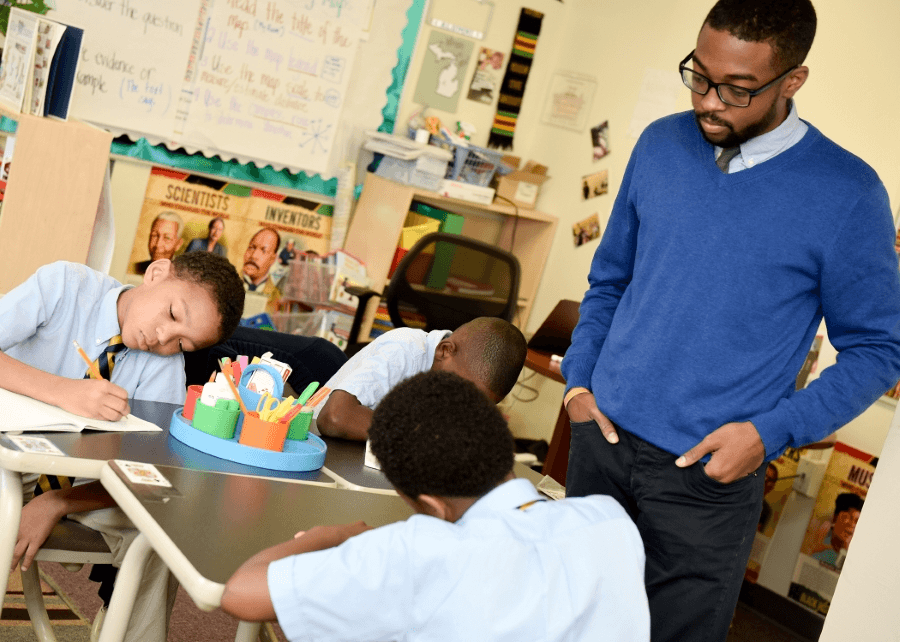
Name this Behavior Support Technique
Proximity
What are things we want to monitor during a restraint?
Examples: Skin color, respiration, and positioning
Name 3 things to remember/consider with positioning when in this restraint:
Examples: stay off wrists; stay off knees; do not bend child forward; face out on the legs; wrap legs; maintain shoulder contact with your partner on the way down the wall; heads out of the way
What are the 3 Recovery Phase Outcomes?
Higher (Educateur), No Change (Firefighter), and Lower (abuser)
A patient is standing on the bed. You are concerned he will get hurt. You ask the patient to get down; he refuses. Name one option to avoid the conflict cycle.
Options include: redirect to something more positive; change the expectation; manage the environment and make the ground around the bed safe, etc.
What are 3 non-verbal techniques to utilize when working with an agitated individual?
Silence, head nods, facial expression, eye contact, and personal space
List the steps of an LSI
Isolate, Explore, Summarize, Connect Feelings to Behaviors, Alternative Behaviors, Plan/Practice, Enter back into the program
Running away, self-harm, and defiance are all examples of what type of behavior?
Pain Based Behavior
"Adam! Stop fighting now!" is an example of which Behavior Support Technique?
Directive Statement
Physical restraint should only be used when what criteria are present?
Agency policies and state regulations approve it; ICMP approves it, professional dynamic risk assessment indicates it.
What are the 4 elements of a potentially violent situation?
Trigger, target, weapon, level of stress or motivation
Proactive or Reactive?
Reactive Aggression
Give an example of something that could be used as a redirection to a more positive activity
Examples: having child help with something, coloring, writing thoughts down, etc
What are 3 non-verbal considerations when working with an agitated patient?
Height, gender, eye contact, personal space, body language, culture
Which LSI step is demonstrated here?
Connect
What are the two goals of crisis intervention?
Support environmentally and emotionally to reduce stress and risk; Teach new coping skills
Name the technique!
Prompting
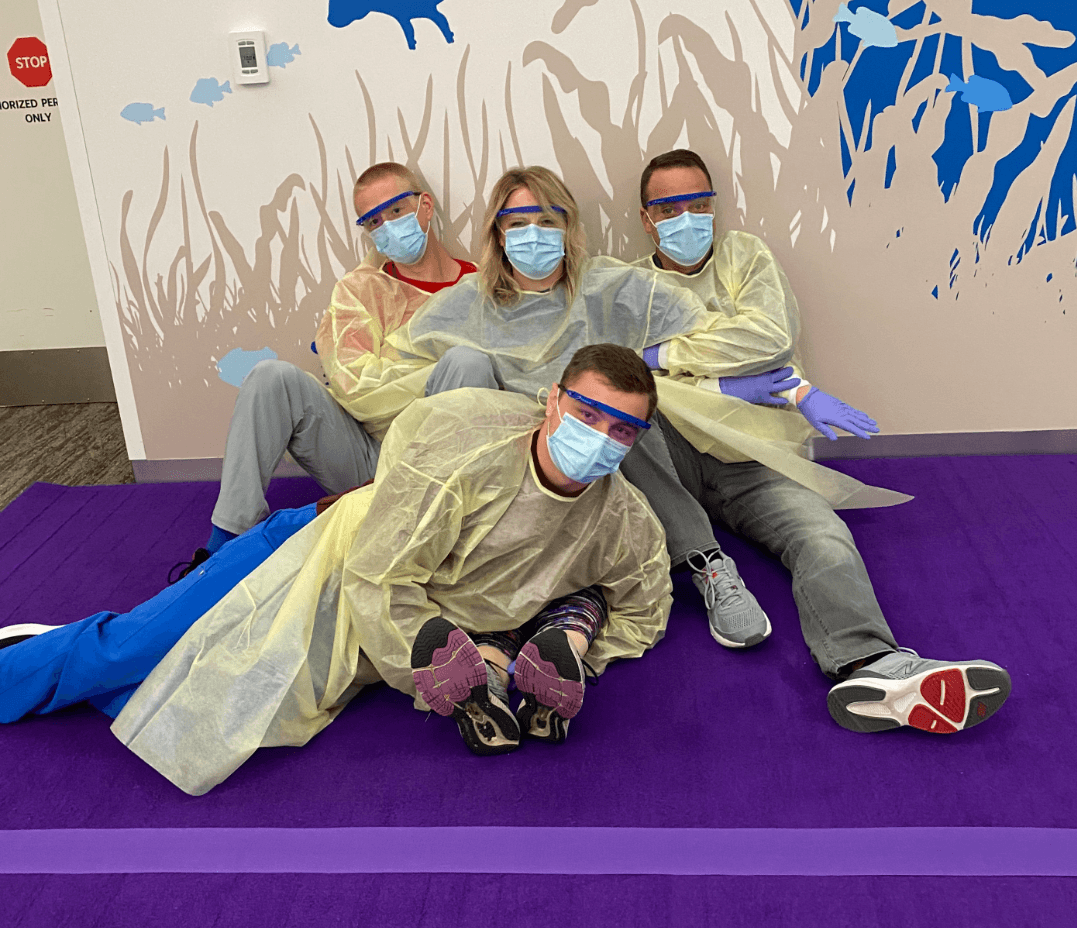
Name this maneuver!
NCH-approved Backwards Carry
List 4 ways to handle physical violence that DON'T include a restraint
Eliminate one of the elements, make a directive statement, use releases and keep distance, leave situation and get help
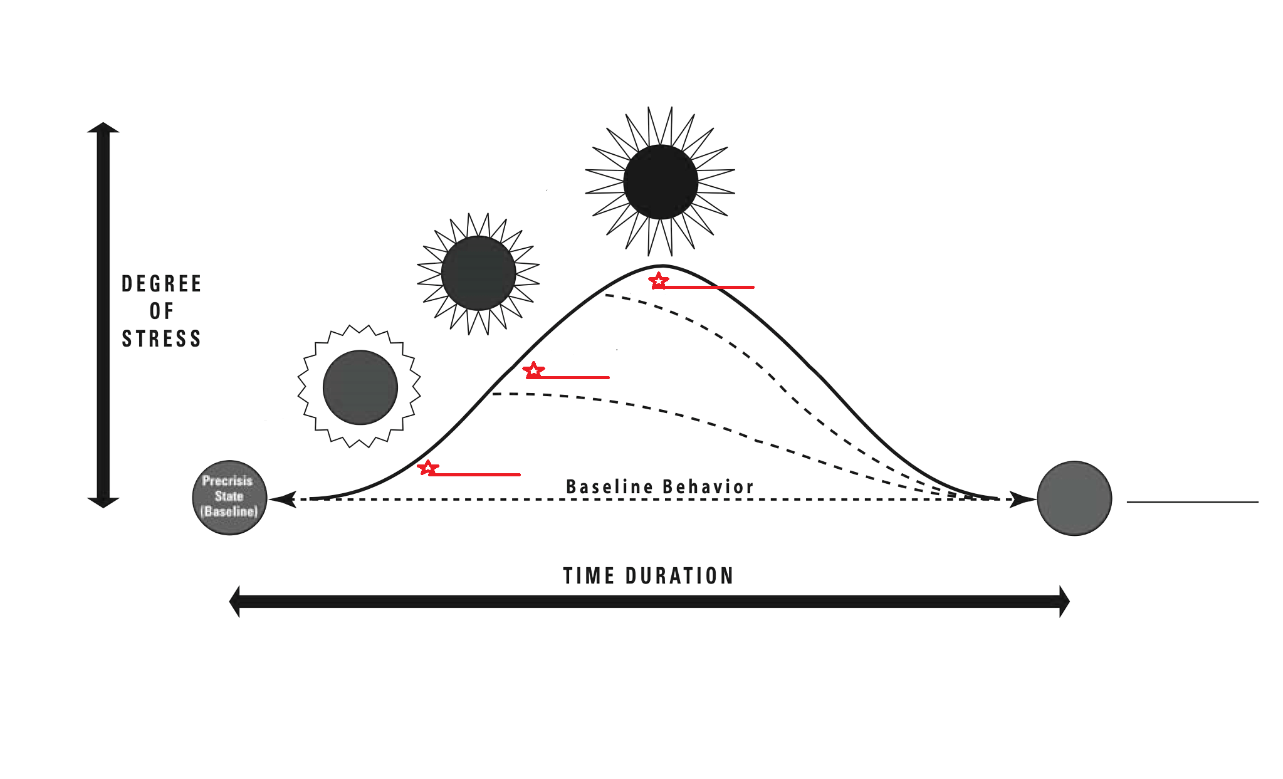 Label the off-ramps...
Label the off-ramps...
Agitation, Aggression, and Violence
"If you're in it to win it, you've ____ ______!"
If you're in it to win it, you've already lost!
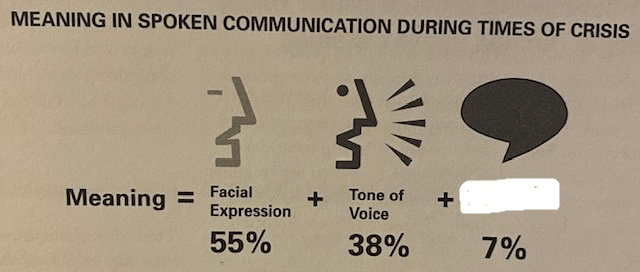 Fill in the blank. Then, explain the point of this graphic
Fill in the blank. Then, explain the point of this graphic
Words; graphic shows that our facial expression and our tone are so important in terms of what we are communicating; words are not primary. It's also important for our body language and expressions to match the words we are saying.
As a careworker, you should be spending the most time inside of this step when conducting an LSI.
Explore
Make a "connect" statement
Example: "Every time you feel threatened, you punch what's in front of you."
Adam and Dan are playing UNO on the unit. Both are very energetic about the game and have difficulty remaining appropriately calm. Dan begins to tease Adam for picking the wrong cards. Adam begins to escalate and appears overwhelmed. Which Behavior Support Technique would you use, and what would we need to know about Adam for this to be an option?
Time Away; we need to know he can self-regulate
Name 3 ways to reduce injury/death in a restraint
Examples: never place weight on chest or back, never put pressure on neck, never bend a child forward, never use on kids under 5, never restrain on a soft surface, etc.
List all 6 predisposing risk factors to a restraint
Obesity, under influence of alcohol/drugs, prolonged agitation, underlying natural disease, hot humid, taking certain meds
 True or False (and explain your answer): A patient throws a chair at the TV in his room. This is an example of a violent outburst.
True or False (and explain your answer): A patient throws a chair at the TV in his room. This is an example of a violent outburst.
False; TCI would consider this aggression (not violence), as it is property destruction and NOT harm toward self or others.
Share a good validating statement that could be used when a child is upset about having to stay at the hospital
Example: "I'm sorry, I know today isn't going the way you had hoped. You're right, this is a stressful situation...but we will get through it together."
What are the 4 questions we ask ourselves when faced with a crisis situation?
What am I feeling? What does the patient feel/need/want? How is the environment affecting the patient? How do I best respond?
List the 5 goals of an LSI
Return to baseline, clarify events, repair relationship, teach new coping skills, re-enter back into the program
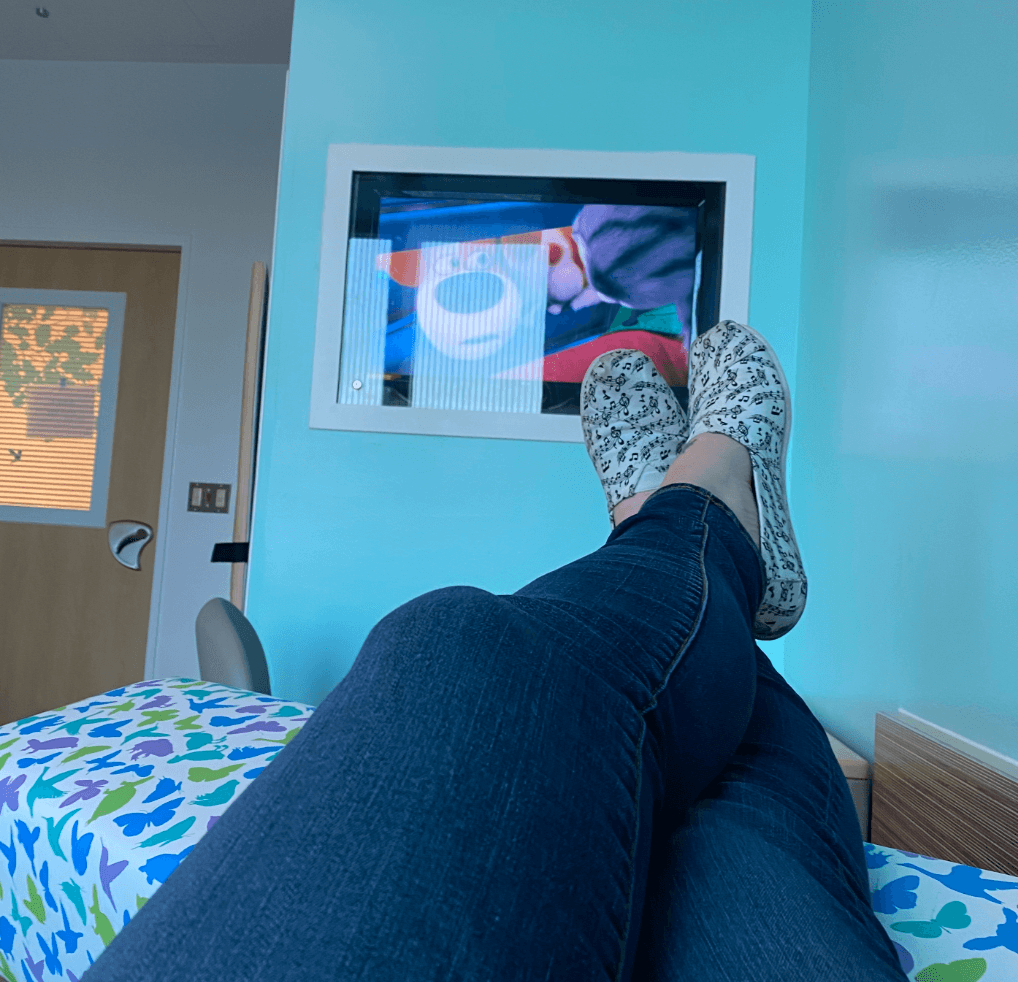
The BHP has TV's installed in each patient room, providing kids with the ability to control channels, movies, etc. on their own. This is an example of an environmental setting condition. How might this choice make challenging behavior more or less likely to occur?
Example answer: Patients may feel that they have control and personal choice during their leisure time; tv/movies can offer a distraction/redirection; can promote a calming physical environment