What are the hyperglycemic medical emergencies for Type 1 diabetes. Give a brief description of each condition, the signs and symptoms, and the complications
Type 1: Diabetic Ketoacidosis: The body can't produce enough insulin, so it will have an EXCESSIVE amount of ketones in the body
SS: DKA is Deadly: Delirium/psychosis, Kussmaul respirations (rapid, deep breathing), Abdominal pain/nausea/vomiting, Dehydration. Fruity breath odor due to exhaled acetone.
Causes life-threatening mucormycosis (a fungal infection, cerebral edema, cardiac arrhythmias.
What are 3 signs and symptoms of Type 2 Diabetes (in medical lingo)
polyuria (excessive urination), polydipsia excessive thirst), fatigue, and weight gain.
Not always present
What is one major tell tale symptom that is completely opposite in Type 1 vs Type 2 diabetes?
Weight loss, insulin count is low (Type 1)
Weight gain, insulin count is high indicating resitance (Type 2)
How do you diagnose diabetes? Give me the tests and relative ranges

What is the first line treatment for type 2 diabetes? What is its MOA?
What are 2 adverse effects seen with this med?
Metformin
MOA:

Lactic acidosis, Vitamin B12 def.
What is the glucose level of a pt with DKA?
>300 mg/dl
At what point does an elevated glucose level become symptomatic? At what level does it become toxic?
Abnormal level of 126 is considered asymptomatic. Over 200 generally causes symptoms.
Toxic is over 240 ng/ml
How does insulin even get glucose into the cell.
Insulin binds to receptors (insulin receptors) on the cell's surface, causing GLUT4 (glucose transporters) molecules to come to the cell's surface in their vesicles.
What 2 hormones related to diabetes is produced in the Pancreas? What are their functions? What part of the pancreas produces them?
Bonus: What part of the pancreas produces the somatostatin?
Insulin: Glucose to cells (b-part)
Glucagon: Glucose to bloodstream (a-part)
Islet of langerhans
A patient with an elevated BUN and GFR comes in with diabete. You give her a medication and she comes back on a follow up with a broken arm after barely falling off her bike.
What medication did you give her? and What is its MOA?
Pioglitazone (rosiglitazone not really given because of MI issues).

Activate PPAR-γ (a nuclear receptor) which increases insulin sensitivity and levels of adiponectin in turn helping with regulation of glucose metabolism and fatty acid storage.

What is C-peptide? Why did the physician order that test?
How would the reason for ordering the test differ if the pt had type 1 diabetes?
C-peptide is measured to tell the difference between insulin the body produces and insulin that is injected into the body. Someone with type 1 or type 2 diabetes may have their C-peptide level measured to see if their body is still producing insulin
The physician ran this test to see if the body was secreting excess insulin for a really high amount of blood sugar
What is the difference between the transporters GLUT2 and GLUT 4
The key difference between GLUT2 and GLUT4 is that GLUT2 does not rely on insulin to carry out protein-facilitated glucose movement across cell membranes. In contrast, GLUT4 relies on insulin to carry out protein-facilitated glucose movement across cell membranes
What are the hyperglycemic medical emergencies for Type 1 diabetes. Give a brief description of each condition, the signs and symptoms, and the complications
Extra points if you explain why hyperglycemia causes dehydration
Type 2: Hyperosmolar hyperglycemic state: Profound hyperglycemia that causes dehydration by excreting the extra glucose which makes you to excrete fluids (water follows)
SS: Thirst, polyuria, lethargy, focal neurologic deficits, seizures.
Can progress to coma and death if untreated
What is the HgA1C test MOA?
Test that checks for the amount of glycated hemoglobin (hgb with a glucose attatched to it) in the RBC life cycle (~3 months).
If you wanna be a tweaker: the non enzymatic glycation of the beta chain of hemoglobin which occurs at the terminal valine
Chelsea F.C splurged a large quantity on a bust as per usual (sorry Jacob 🤓). This particular player gained a tremendous amount of weight and decided to take a popular weight loss drug (that Dr. Pittman mentioned in class) that is also used to treat diabetes.
What is this drug class and its MOA?
GLP-1 analogs (ex. most popular is ozempic brand name). They wil typically end in -tide, -glutide.
MOA: Decrease glucagon (excessive post meal glucagon) release and stimulate glucose dependent insulin release from the beta cells.
What is gestational diabetes?
Bonus points if you can explain the most likely theory for why this occurs
Unlike type 1 diabetes, gestational diabetes is not caused by a lack of insulin, but by other hormones produced during pregnancy that can make insulin less effective
The placenta supplies a growing fetus with nutrients and water, and also produces a variety of hormones to maintain the pregnancy. Some of these hormones (estrogen, cortisol, and human placental lactogen) can have a blocking effect on insulin. This is called contra-insulin effect, which usually begins about 20 to 24 weeks into the pregnancy.
Describe what MODY (mature-onset type 2 diabetes) is? And what population it would normally effect
A defect in the expression of the glucokinase gene. Causes an increase in the glucose threshold required to promote insulin secretions. Usually prevalant in populations before the age of 30.
Treatment is not usually beneficial
How does the pancreatic cells compensate to produce more insulin in Type 2 diabetes?
How does this lead to B-cell amyloid deposits.
The insulin (b-cells) in the islets will undergo hyperplasia and hypertrophy to secrete more insulin and will initially work and keep glucose levels normal.
The B-cells will also secrete Islet amyloid Polypeptide (Amylin) alongside insulin that will deposit aggregates of amyloid.
Eventually, this is not sustainable and the islets will undergo hypotrophy and hypoplasia
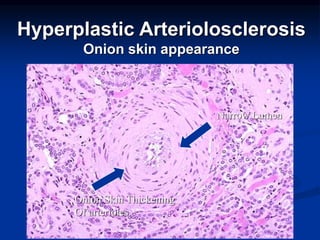
Bonus points if you can tell me how this looks histologically.
Hyaline arteriosclerosis occurs secondary to diabetes and is the thickening of the walls or arterioles due to the deposition of a "pink" hyaline material.
This is indicative f in diabetes (or most of the time hypertension) leakage of plasma components across the vascular endothelium leads to excessive matrix production by smooth muscle cells which leads to the thickening.
Your diabetic patient comes in with elevated blood pressure repeadetly. Urinalysis shows protein in the urine. The appropriate class of medication to give this patient at this time is:
Pt showing early signs of diabetic nephropathy
ACE Inhibitors or ARB blockers: slows diabetic nephropathy and helps modulate the blood pressure
What are the differences between Lispro, Aspart, and Glulisine and medications such as Detemir and Glargine
When do you take these drugs?
Short acting: Lispro, Aspart, and Glulisine-Take before meals
Long Acting: Detemir and Glargine. Preferably before bedtime for continuous management.
A long standing patient has diabetes and is beginning to feel tingling in the extremities and spots and blurriness in their vision. What condition do they have and explain how biochemically this is occuring with steps?
The absence of what enzyme can elicit the same clinical manifestation?
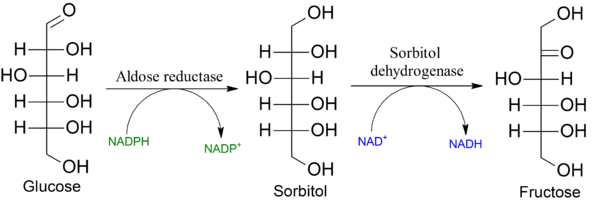 Normally, glucose will enter cells and be converted to sorbitol. Sorbitol is considered an osmotic agent meaning it attracts water in cells. As a protective mechanism we can convert sorbitol to fructose through the enzyme sorbitol dehydrogenase. An excess of glucose leads to an excess of sorbitol that is osmotic and (toxic).
Normally, glucose will enter cells and be converted to sorbitol. Sorbitol is considered an osmotic agent meaning it attracts water in cells. As a protective mechanism we can convert sorbitol to fructose through the enzyme sorbitol dehydrogenase. An excess of glucose leads to an excess of sorbitol that is osmotic and (toxic).
The cells of the lens, retina, and Schwann cells do not have the ability to convert to fructose. Therefore the neuropathy, and more noticably the diabetic retinopathy is noticed much sooner in these areas.
Explain how glucose utilizes a positive feedback to stimulate even more insulin release leads to insulin release from the B-cells.
Glucose enters the GLUT4 transporter channels-> Glucose enters the beta cells -> will increase ATP generated from glucose metabolism ->will close the K+ channel and will depolarize the B-cell membrane -> Voltage gated Ca2+ channels open leading to Ca2+ influx-> stimulates the release of insulin exocytosis

Your healthy and fit 21 year old patient comes in with the following labs:
Glucose: Elevated
HgA1C: Elevated
Insulin: Normal (not low, and not elevated)
What type of diabetes does this patient have? and WHY? How would you treat?
Type 1.5 Diabetes. Subtype of type 1 that presents such as type 2. Treat with restrictive diet and in severe cases insulin.
Your patient comes in with severe hypoglycelmia, what is the appropriate treamtment, and what is its MOA? Assume u don't have access to IV glucose
Assuming this patient has a standard diet, what could be causing this patient's hypoglycemia
IM/ Intranasal glucagon. Will upregulate hepatic glycogenolysis and gluconeogenesis by binding to a hepatic GPCR activating Gs -> stimulate adenylate cyclase -> produce more cAMP -> increases PKA which promotes those pathways
Insulinoma