Which meniscus is more firmly attached to the tibia?
Medial meniscus
Describe the role of the quadricep during the normal gait cycle
What does it do at initial contact and loading response?
What happens towards mid stance?
preswing?
initial swing?
Loss of function results in what?
Controls flexion during initial contact and loading response
Extends knee toward midstance
Controls flexion during pre swing
Prevents excessive heel rise during initial swing
**Loss of function results in lurching trunk anteriorly at initial contact to extend knee
Different kind of TKA designs
Unconstrained: no built in ______ to the prosthesis
What needs to be in tact?
Used mainly with what kind of TKA?
Semiconstrained: some stability built in with little compromise to ______
Are these common?
What ligaments are needed?
Fixed bearing/mobile platform: has a ______ platform to allow______ and ______ to reduce premature wearing
Cruciate retaining: _____ is excised except in Unicomp design. _____can be saved for posterior stability
Unconstrained: no built in stability to the prosthesis
In tact MCL and LCL are needed
Used mainly with unicompartmental design
Semiconstrained: some stability built in with little compromise to mobility
Most TKAs today
MCL and LCL ligaments are needed
Fixed bearing/mobile platform: has a rotating platform to allow rotation and sliding to reduce premature wearing
Cruciate retaining: ACL is excised except in Unicomp design. PCL can be saved for posterior stability
Precautions after ACL reconstruction
What are some precautions for resistance training?
Hamstring graft vs Patellar tendon graft: which should you progress slower with?
What should we keep in mind with CKC training? (squatting)
Avoid CKC strengthening between what degrees of flexion?
In open chain training avoid applying resistance to what part of the tibia for 4-8 weeks?
Resistance training - general precautions
Progress slower with hamstring graft than patellar tendon graft
Use caution progressing hamstring strength if ham graft is used
Hamstrings are extra support for ACL
Use caution progressing knee extensor strength if patellar tendon graft is used
CKC training
Keep knees even or behind toes when squatting to avoid anterior shear forces on graft
Avoid CKC strengthening between 60-90 degrees of knee flexion
Open chain training
During PREs to strengthen hip muscles, place resistance above the knee at first until control is established
Controls valgus moment - responsible for which way the femur is going to go
Avoid resisted open chain SAQ between 45-0 for 6-12 weeks
Avoid applying resistance to distal tibia during quad strengthening (maybe 4-8 weeks)
Probably wont do any MRE for ACL recovery
A condition described as softening and fissuring of the posterior surface of the cartilaginous area of the patella
Chondromalacia patellae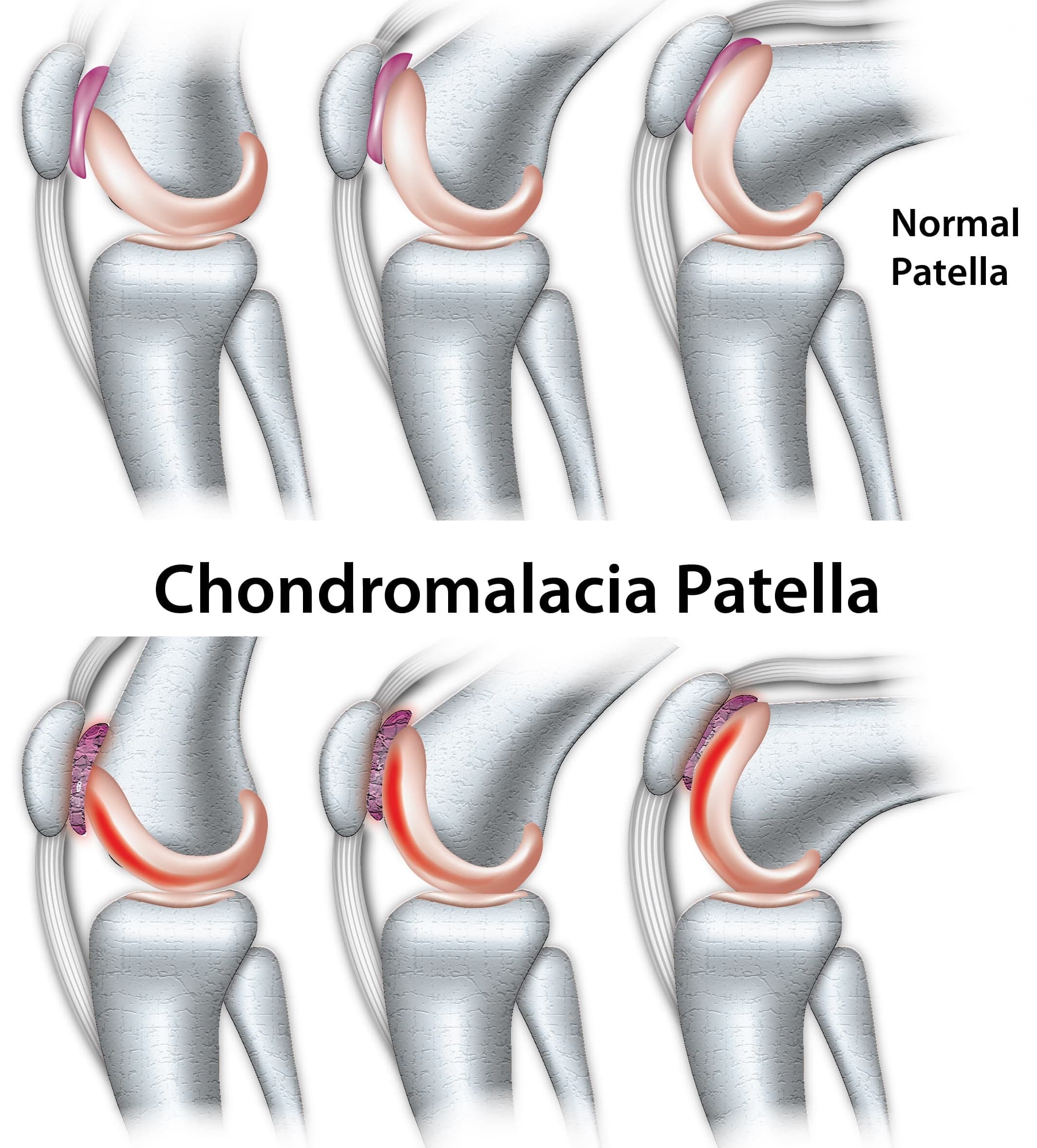
Which femoral condyle is longer
The medial femoral condyle
Describe the role of the Hamstrings during the normal gait cycle
Loss of function results in what?
Decelerate and control extension during terminal swing
**Loss of function results in genu recurvatum and snapping into extension
Cemented vs non-cemented vs hybrid TKA
Which is the gold standard?
Which method provides immediate stability?
Which will last longer?
Which can you not put weight on right away?
Which combines both?
Cemented
The gold standard for TKA, cemented fixation uses a thin layer of bone cement to secure the prosthesis to the bone. This method provides immediate stability and fixation. However, younger patients who have cemented TKAs have a higher risk of revision.
Non-cemented
Some surgeons use cementless prostheses to reduce aseptic loosening and promote long-term implant survival. However, critics say that cementless implants may have increased rates of periprosthetic and femoral component fractures, and reduced long-term implant survival.
Hybrid
Hybrid fixation combines cemented tibial fixation with cementless femoral fixation. This technique may offer the advantages of cementless fixation while avoiding the risk of tibial loosening that can occur with full-cementless TKA
Return to Function Post-ACL reconstruction
How do we know when our patients are ready to return to sport?
No knee pain or effusion during final stage of rehab
Full active ROM
Quad strength is 90% of non-surgical leg
Hamstring strength is 100% of other leg
Negative pivot shift test (surgeon does this)
Passes functional testing of hopping, jumping, squat at 90% of other leg
Articular cartilage degeneration
Most common disease affecting weight bearing joints
33% over 65 have radiographic evidence of OA
Pain, medial joint laxity, limited ROM, weakness, knee buckling sensation, genu varum deformity
Osteoarthritis
Factors that influence:
Excess weight
Joint trauma
Weak quads
Abnormal tibia rotation
Plica syndrome
condition in which a fold of synovial tissue in the knee, called a plica, becomes irritated or inflamed. The plica is a normal structure found in the knee, and in most people, it is asymptomatic. However, if it becomes thickened or irritated due to overuse, trauma, or repetitive movements, it can lead to pain and dysfunction.
Describe the role of the soleus during the normal gait cycle
Controls amount of knee flexion during pre swing by controlling forward movement of tibia
Goals, interventions, and presentation of a TKA in the maximum protection phases
ROM will be limited to?
WBAT with what kind of TKA?
Delayed WBAT with what kind of TKA?
How strong should we want there quads to be?
Why ankle pumps?
Muscle setting of what?
Stretching what?
Presentation
ROM will be limited to 10-60 degrees
WBAT with cemented; delayed with hybrid or non-cemented
Goals
Control pain and swelling
Gain ROM to 0-90*; at least ⅗ quad strength
Ambulate with/without assistive device
Establish a HEP
Interventions
Pain modulation modalities
Compression wraps
Ankle pumps to minimize DVTs
AAROM/AROM
Muscle setting of quads, hams, add
Gait training
Stretching of hams, calf, IT band
Trunk/pelvis stabilization exercises
Posterior Cruciate Ligament (PCL).
How common is an injury of this ligament?
What kinds of grafts are used?
Open chain knee flexion is delayed for how long?
Emphasis on strengthening what?
Will this take longer or shorter to recover than an ACL injury?
Take precaution with exercises that place what kind of force on the tibia?
Rare form of injury
Uses same types of grafts as ACL with addition of achilles tendon, anterior tibialis
Knee usually be immobilized in extension for 4-8 weeks to prevent accidental posterior translation of tibia by knee flexors - evidence is poor to support this theory
Open chain knee flexion delayed 6-12 weeks
Rehab is mostly the same as ACL except:
Emphasis on quad strengthening in functional positions
Closed chain activities are delayed due to WB being restricted for a longer period
May take up to 3 months longer for full return than ACL injuries
Need to take caution with exercises that place posterior shear forces on tibia
Hamstrings pulling back
Occurs in response to trauma to the knee joint and structures
Posttraumatic arthritis
Describe the role of the gastroc during the normal gait cycle
Provides muscle tension to post knee when its in extension (end of loading response)
TKA Management Moderate Protection Phase (Week 4-8)
What is ROM be limited to?
How much pain will they have?
FWB except with what type of TKA design?
What are some goals?
What are some interventions?
What mobs?
Presentation
Pain in minimal
ROM 0-90*
FWB except with uncemented
Joint effusion controlled
Balance and functional mobility is impaired
Diminished cardio
Goals
Reduce swelling
ROM 0-110
⅘ MMT
HEP
Good balance and functional mobility
Interventions
Patellar mobs
LE stretching
CKC strengthening
Limited range PREs
Tib-fem joint mobs
Proprio training
Stabilization/balance exercises
Swimming/walking/biking
PCL Rehab
Avoid exercises that place what kind of force on the tibia?
What to consider in early and immediate rehab?
Avoid leaning forward too much during squatting why?
Avoid knee flexion past 60-70* when squatting why?
Where should resistance be in relationship to the knee when performing standing hip exercises?
IN ADVANCE TRAINING
Is jogging down hill okay?
How long to wait before returning to vigorous activities?
General Precautions
Avoid exercises that places shear forces posterior
Early and immediate rehab considerations
To restore knee flexion early on, begin in seats allowing gravity to assist, and allowing hams to remain inactive
Avoid leaning forward too much during squatting because it increases ham activity
Avoid knee flexion past 60-70* when squatting because it causes post translation
Place resistance above the knee when performing hip exercises in standing
Postpone open chain knee flexion against gravity for 6-12 weeks
Advanced rehabilitation considerations
Postpone resistance training for knee flexors using ham curl machine for 5-6 months AND use low loads
Avoid downhill inclines during walking, jogging, or hiking
Avoid activities that involve knee flexion combined with rapid deceleration when one or both feet are planted
Wait 9-12 months before returning to vigorous activities
Manifests early in hands and feet
Later moves to knees
Presents with warm swollen knees with limited ROM and genu valgum deformity
Rheumatoid arthritis
Does the MCL attach to the medial meniscus
Yes
Explain pathological gait when there is a hip flexure contractures
What is there a loss of?
How will this affect gait?
Loss of hip extension = flexed knee at terminal stance
TKA Management Minimum Protection Phase (beyond week 8)
How much muscle function will they have compared to the non-involved leg?
Will the pt. still present with pain?
What will be impaired?
What are some goals?
What kind of interventions?
Presentation
Muscle function is 70% of non-involved
No pain or swelling
Impaired balance and functional mobility
Goals
Develop maintenance program
Community ambulation
Improve cardio
Interventions
Continue as previous phase and advance as appropriate
Progression of balance and advanced functional activities
Meniscus injuries.
How much of the meniscus is vascular?
What kind of tear can cause knee lock?
Which side of the meniscus is fixed more firmly to the tibia plateau?
Both menisci have a degree of movement with flexion and extension of the knee
Flexion - moves ______
Extension - moves ______
Part of what knee ligament attaches to the medial meniscus?
Which menisci do the hamstrings attach too?
Meniscus repair will require a period of _____ while meniscectomy will not
Mechanism
Can be degenerative tears or traumatic
If traumatic, usually flexion or rotation forces are involved
Meniscus is vascular in outer ⅓ and has the ability to heal itself if the tear is in this portion - most tears are not in this red zone (blood supply zone)
Bucket handle tear can cause knee to lock - sometimes responds to manipulation
Medial meniscus is fixed more firmly to tibial plateau than lateral meniscus
Medial more prone to injury because it doesn’t move as much
Both menisci have a degree of movement with flexion and extension of the knee
Flexion - moves posterior
Extension - moves anterior
Important to note that part of deep MCL attaches to medial meniscus
Hamstring musculature has attachment sites to both menisci
Meniscus repair will require a period of NWB while meniscectomy will not
What happens with immobilization?
Contractures of capsule, muscles, soft tissue
Adhesions restrict caudal glide of patella limiting knee flexion
If patella does not glide proximally with quad contraction = extensor lag
Extensor lag = can’t hold extension actively but ROM is there passively
Knee Basics
What type of joint is the knee?Cruciate ligaments provide stability in which direction?
Collateral ligaments provide stability in which direction?
What do coronary ligaments attach to?
Biaxial modified hinge joint
Anterior-posterior stability provided by cruciate ligaments
Mediolateral stability provided by collateral ligaments
Menisci improve articulation - attached to joint capsule by coronary ligaments
Explain pathological gait when there is length/strength imbalances
What can a length/strength imbalance do to the knee? (or any part of the body)
example?
Changes stresses on structures of the knee
Ex: tight TFL = lateral knee pain = maltracking of patella (abnormal alignment or movement during walking)
Activities with a Post-TKA
What kind of activities are highly recommended?
What kind of activities are recommended?
What kinds of activities are not recommended?
Highly recommended
Stationary bike, swimming, water aerobics, walking, golf with cart, ballroom dancing, table tennis
Recommended
Road cycling, speed/power walking, low impact aerobics, cross country skiing, doubles tennis, rowing, bowling, canoeing
Not recommended
Jogging, basketball, volleyball, singles tennis, baseball, high impact aerobics, water skiing, football, soccer
Explain the screw home mechanism during extension close packed (think baseball)
Femur rotates internally, hip moved into extension
As knee is unlocked, femur rotates laterally
Hip extension is important to achieve full knee extension
Explain pathological gait when there is a foot impairment
What is pes planus?
What is pes cavus?
How would these deformities impact the position of the knee and hip?
Impact position of the knee and position of the hip
Ex: Pes planus = genu valgus = coxa vara
Ex: Pes cavus = genu varum = coxa valgus
Ligament Injuries.
Generally happens to what ages?
Which is the most common?
Which is the most rare?
What is the terrible triad?
A forceful blow to anterior tibia usually injures this ligament...
Which ligament would get injured from a valgus force?
Generally happen between 20-40 yrs old
ACL is most common
Contact or non-contact
Terrible triad - ACL, MCL, medial meniscus (usually go together)
What forces cause ACL tear?
Valgus with ER of tibia (weak glutes, hip abductors)
Forced hyperextension
PCL
Usually from forceful blow to anterior tibia - pushes tibia posteriorly
MCL (deep and superficial)
From valgus forces - straight blow from the lateral side
Tears can be partial or complete
Deep MCL can heal well - lock in 0* brace
In flexion there is more movement - ligament isn’t taut
MCL attaches to the medial meniscus
LCL (rare)
From medial blow
Varus force
Which meniscus is more firmly attached?
Which is more prone to injury?
Medial meniscus is more firmly attached Higher weight bearing stress and higher risk of injury
Describe the protection phase of joint hypomobility management as pertains to the knee.
What to teach me?
What should they avoid?
How can we maintain soft tissue integrity and joint mobility?
How can we maintain muscle functions and prevent patellar adhesions?
Control pain and protect the joint
Teach patient how to protect the joint, bed positioning, ROM and muscle setting
Instruct patient to minimize stair climbing, avoid sitting on low surfaces, minimize excessive flexion ranges with weight bearing
Maintain soft tissue integrity and joint mobility
PROM, AAROM, AROM within pain free range
Gr I, II joint distractions or A/P glides in loose packed position
Stretching is contraindicated at this stage
Maintain muscle function and prevent patellar adhesions
Pain free muscle setting
Quad sets with SLF
Patella mobilization
Ligament injuries and female athletes
What type of ACL injury is much more prevalent for women? (3x more likely than men)
What role does hormonal changes play in injury?
T/F: Women have a larger femoral notch- A shaped rather than U shaped.
Non contact ACL injuries much more prevalent (3x more likely than men)
Increased Q angle - more chance of landing incorrectly from a jump
Valgus moment at landing after a jump and decreased use of hip extensors
Hormonal changes (increased risk of injury during ovulation)
Smaller femoral notch - A shaped rather than U shaped - causes ACL to contact bones sooner from blow and tear easier
Notchplasty to fix shape and size of femoral notch
ACL is less elastic in females
The meniscus moves _______ in flexion and _______ in extension
1.posteriorly
2.anteriorly
Describe the controlled motion and return to function Phase of joint hypomobility management as pertains to the knee.
What would you educate the patient on?
What would be in the HEP?How would you decrease pain from mechanical stress?
What kind of stretching if any?
What kind of exercises?
How can we improve their cardio endurance?
Patient education
Talk to them about recovery and what to expect
Provide HEP with strengthening, ROM, stretching, low impact exercises, stationary bike
Decrease pain from mechanical stress
Use assistive devices as necessary
Increase joint play/ROM (tib-fem & patellar mobs) MWM (lab)
Stretching
PNF stretching; low load long duration stretching (grocery bag hanging)
Improve muscle performance in supporting muscles
Progressive stretching
Start with multiple angle isometrics and progress to open and closed chain exercises
Open chain are less painful with lighter loads and faster reps instead of the opposite
Resistance through midrange (45-90) tends to increase PFP due to compression
Strengthen both hip and ankle
Include endurance
Functional training
Steps, squats, sit-stands, partial lunges, balance activities
Improve cardio endurance
Bike, swimming, water aerobics
ACL Reconstruction
What are some indications?
What are some treatment options?
Indications
Severe tear or chronic insufficiency of the ACL
Pivot-shift test is abnormal
Limitation of functional movements
Failed conservative treatment
Treatments
Patellar tendon graft; allograft; synthetic graft; autograft involving semitendinosus/gracilis tendon
Bone-tendon-bone
Chronic instability = early onset OA - proper management is super important
As the knee extends the patella slides in which direction?
Superiorly
What role does microfractures play in Repair of articular cartilage defects?
What does arthroscopic mean?
Used for repair of small defects usually to the medial or lateral femoral condyle
Arthroscopic - subchondral bone is penetrated to stimulate marrow based response leading to local ingrowth of fibrocartilage to repair the lesion
ACL Rehabilitation
What is a Cyclops lesion?
Types of grafts?
What's the key?
Depends on the type of surgical procedure and type of graft
Any graft type will be weakest the first 6-8 weeks
Key is re-vascularization of the graft
Cyclopse lesion
Inhibits knee extension - usually when can’t get back through PT
Fibrous nodule in intracondylar notch - error in surgery
As the knee flexes what happens to the patella?
The patella enters the intracondylar groove
What is a osteochondral autograft transplantation?
What surfaces of the knee are they usually done on?
MD uses plugs from a site that has part bone and part articular cartilage
Used usually on weight bearing surfaces of the knee
Patella graft
What are some advantages?
What are some disadvantages?
Would you be able to return pre injury, high demand activities?
Patella BTB (Bone to Bone)
Advantages
High tensile strength
Secure and reliable bone to bone graft fixation with screws
Rapid revascularization in 6 weeks at bone to bone interface permitting safe rehab
Ability to return to preinjury, high demand activities safely
Disadvantages
Anterior knee pain in surgical knee
Pain with kneeling
Patellofemoral dysfunction
Patellar fracture during graft harvest (rare)
Patellar tendon rupture (rare)
Does the patella affect knee flexion and extension?
If patellar movement is restricted, interferes with knee flexion and active knee extension.
What are autologous chondrocyte implantations?
They are usually for lesions where?
How many stages is the procedure?
How long does the whole process take?
Usually for lesions on patella or femoral condyles
2 stage procedure - healthy cartilage is harvested from patient then chondrocytes are extracted and cultured; implanted in the patient under a patch
Long process - up to 9 months
Hamstring Graft
What are some advantages?
Will kids get a disturbance in the epiphyseal plate with this type of graft?
What are some disadvantages?
What is the healing time?
Advantages
High tensile strength, greater than ACL
No disturbance of epiphyseal plate in adolescent
Patellar BTB can’t be done if epiphyseal plate isn’t fully fused
Evidence of ham tendon regeneration at donor site
Disadvantages
Tendon to bone fixation devices not as reliable as bone to bone fixation
Longer healing time at tendon bone interface 12 weeks
Hamstring muscle strain early on can happen
Ham is active stabilizer of ACL - cautious with hamstring exercises
Short and long term knee flexor weakness
Possible increased anterior knee translation
What is the Q angle and what forces maintain its alignment
The Q angle is a measure of the alignment between your hip, knee, and lower leg. It's the angle formed by two lines:
- From the hip to the center of the kneecap (patella).
- From the kneecap to the shinbone (tibia).

normal angle = 15*
Forces maintaining alignment:
Trochlear groove
ITB/lateral retinaculum
VMO
Patellar ligament
What is a Allograft transplant?
Rare - needs a fresh cadaver
Freezing kills chondrocytes
A procedure that involves transferring tissue, organs, or cells from a donor to a recipient who is not an identical twin of the donor
ACL rehabilitation Maximum Protection Phase (0-4 weeks)
How will the patient present?
How will they ambulate?
What are the goals of this phase?
List some interventions:
What does PRICE stand for?
Why ankle pumps?
Patient presentation
Pain and hemarthrosis
Decreased ROM
Diminished quad contraction
Ambulating with crutches
Sometimes use of protective brace
Goals
Protect healing tissue
Prevent muscle inhibition
Decrease joint effusion
AROM 0-110
Active control of ROM
WBAT or sometimes 75%
Establish HEP
Interventions
PRICE
Gait training with crutches if needed
PROM-AAROM; wall slides for flexion
Patellar mobilizations
Muscle setting with towel under heel for extension
Quad sets/quad contractions is the golden ticket for recovery (pre and post)
Myotrack - patient has to do contraction (can see on the screen)
Assisted SLR supine - quad set first then SLR to keep leg straight (knee will bend without quad contraction)
Ankle pumps to prevent DVTs
After 2-4 weeks progress to full WB with minisquat (only with quad contraction), heel raises, SLR 4-way, ham curls
Open chain knee ext 90-40
Aerobic conditioning
Trunk stabilization (core) - HEP
Compression against femur rises sharply after __* knee flexion
30
Indications for a TKA
Severe pain with what?Whats wrong with the articular cartilage?
What is an example of a marked deformity?
Severe pain with weight bearing
Motion that interferes with functional activity
Destruction of articular cartilage (bone-on-bone)
Gross instability or limitation of motion, marked deformity (genu valgus or varus)
Failure of a previous surgical procedure
Moderate Protection Phase (4-10 weeks) of an ACL repair
What might their MMT test for the knee be?
Will they have full ROM?
Can they ambulate independently?
What are some goals of this phase?
What are some interventions to help towards these goals?
After 7-10 week start more advanced what?
Surgery and swelling prevents what from getting to the brain?
Patient presentation
Decreased swelling and pain
Near full ROM
3+/5 to ⅘ MMT
Independent ambulation
Goals
Full pain-free ROM
⅘ MMT
Dynamic control of knee
Improved kinesthetic awareness
Normalize gait pattern and ADL function
Adherence to HEP
Interventions
Multiple angle isometrics
CKC strengthening and PREs (progressive resistive exercises)
LE stretching; especially hamstrings, ITB, and plantar flexors
Endurance training on bike or elliptical
Proprioceptive training in single leg stance
Bosu ball, balance board, foam, star balance
Stabilization exercises, elastic bands, band walking
After week 7-10 start more advanced strengthening, endurance, and flexibility exercises
Proprioceptive training (surgery and swelling prevents proprioceptive info getting to the brain - need to be retrained)
Stepping drills in high speed
Unstable surface challenge drills
Initiate a walk/jog program
What is a bicompartmental TKA?
What is a Tricompartmental TKA?
1.Entire tib-fem surfaces are replaces (most common)
2. Addition of the patella
What is a Unicompartmental TKA?
What joint surface(s) is replaced
Generally done with patients in what age range?
Only medial or lateral joint surfaces are replaced
Generally in patients <55 yrs

Minimum Protection Phase (11-24 weeks)
Will they have pain?Will they have symmetrical gait?
Goals?
Interventions?
Minimum Protection Phase (11-24 weeks)
Patient presentation
No joint instability or pain or swelling
Muscle function 75% of involved extremity
Symmetrical gait
Goals
Increase strength, endurance, and power
Improve neuromuscular control, dynamic stability, and balance
Regain cardio endurance
Transition to maintenance program and reduce risk of reinjury
Regain ability to function at highest desired level
Interventions
Continue LE strengthening and advance PREs
Advance CKC exercises
Initiate plyos - progress
Bounding, jumping, skipping, jump rope, box jumps, 4 square
Progress agility drills - cones, figure 8
Varied running patterns
Simulate work/sport specific patterns
Transition to full speed jogging, sprints, running, and cutting