This anatomic area, colloquially termed "the box", is delineated by these 3 anatomic borders.
What is sternal notch, xiphoid process and nipples?
Primarily matters for stab wounds

These 2 criteria should prompt a thoracotomy.
What is evacuation of > 1500 mL of blood immediately after chest tube placement or > 200 mL/hr for 4 hours?
Some suggest a lower threshold such as 150-200mL/hr for 2 hrs or > 1000 mL initial.
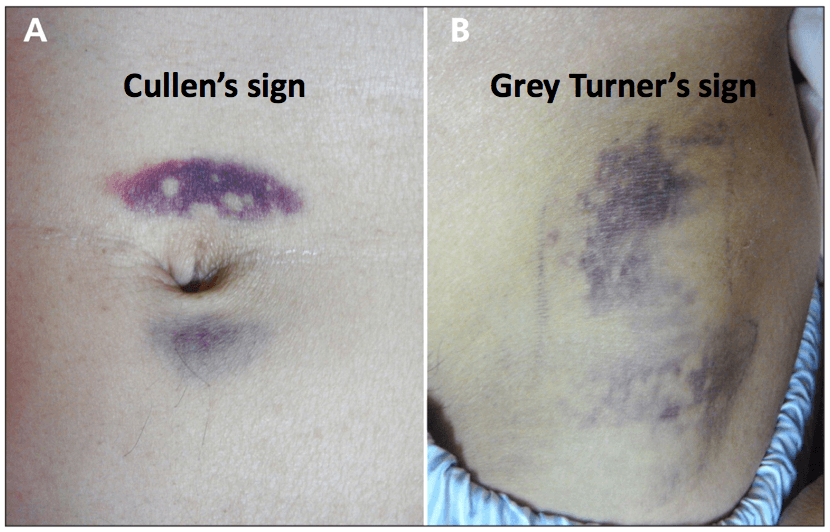
These 2 physical exam signs indicate a retroperitoneal injury.
What are Grey-turner (flank) and Cullen's (peri-umbilical) signs?
One leg makes up this percentage of TBSA.
What is 18%?
You should suspect this injury in a patient who was the front seat passenger in an MVC and now has IR and shortened leg.
What is posterior hip dislocation?
This pathology is caused by blunt trauma to the chest wall and is the 2nd leading cause of death in young athletes.
What is commotion cordis?
Small projectiles (baseball, hockey puck, lacrosse ball, etc)
According to accepted practice algorithms, this is the appropriate management for a stable patient with an isolated sternal fracture and an initial normal ECG.
What is repeat ECG at 6hrs and discharge home if vital signs remain stable?
Easily missed on XR -> CT
High suspicion for associated injuries as high mechanism
This organ is most likely to be injured from penetrating abdominal injury.
What is liver?
Aggressive transfusion in burn patients has been associated with this outcome.
What is increased morbidity and mortality?
You should be concerned about this structure in a pt that was front seat passenger in MVC and now has severe knee pain/swelling and abnormal ABIs.
What is popliteal artery?
Posterior knee dislocation easy to miss as usually spontaneously reduces by the time patient presents to ED.
This finding indicates aspiration of blood from the right ventricle during pericardiocentesis.
What is free flowing blood without clots?
> 20cc without any clots or having to reposition needle = right ventricle
A stab wound patient presents to your rural ED. You find a single stab wound to right chest wall. Initial work-up is negative for significant injury, no evidence of pneumothorax. After 4 hrs the patient develops shortness of breath and hypotension. The treatment for this injury.
What is needle/tube thoracostomy for pneumothorax?
Pneumothorax after a stab wound may be delayed for up to 6 hours. Consequently, repeat chest imaging in 4 to 6 hours is indicated in these patients or at any time when symptoms worsen. Patients with initially asymptomatic stab wounds to the chest have a reported 12% incidence of delayed hemothorax or pneumothorax that required tube thoracostomy.
Coiling of NG tube in thorax is pathopneumonic for this injury.
What is diaphragmatic rupture?
Penetrating trauma most frequent cause.
CXR only ~ 25% sensitive.CT is gold standard . . . but as trauma conference reflects it still misses diaphragm injuries.
A pt with diffuse full thickness burns presents to your ED. You intubate and proceed with remainder of survey when RT says "doc he's getting hard to bag" and you note dropping SpO2 on 100%. This is the emergent treatment to address the pathology.
What is escharotomy of chest?
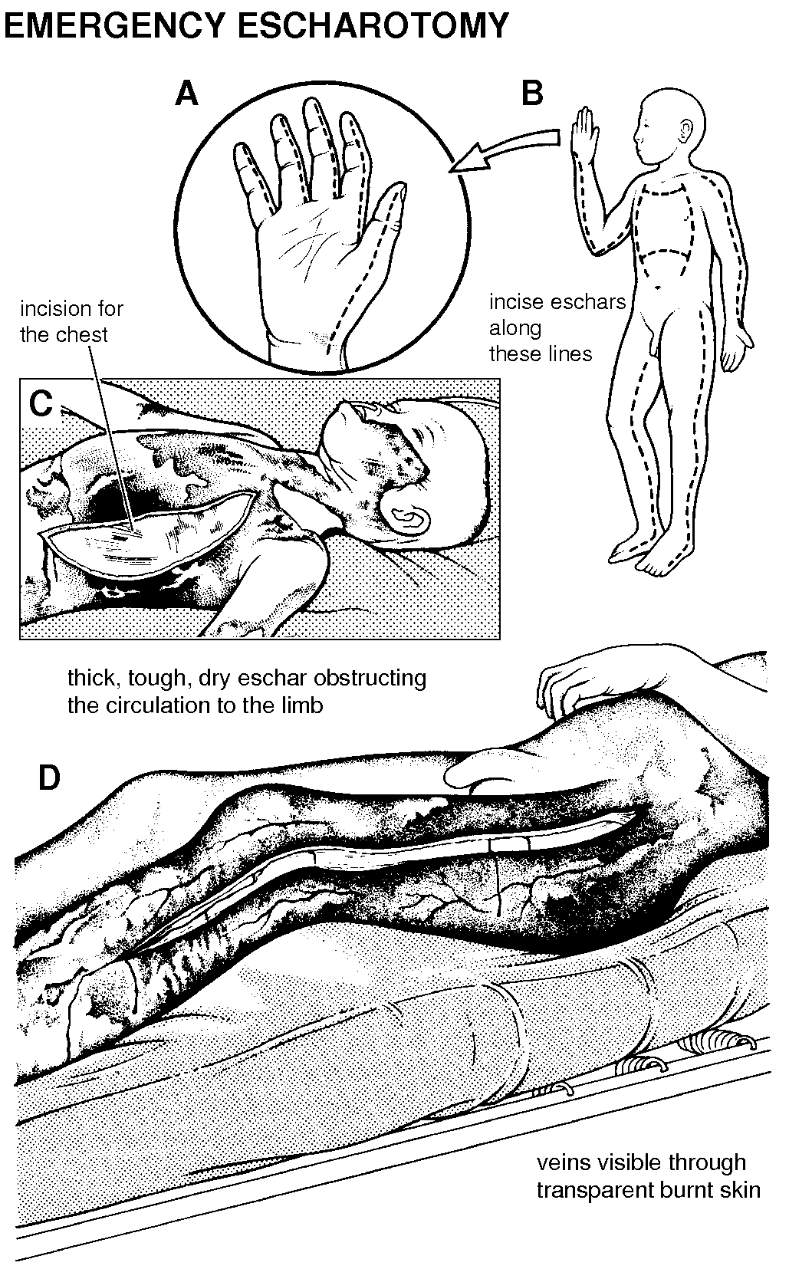
Trunk
- Longitudinal incisions along the anterior axillary lines to the costal margins, or upper abdomen if also burnt.
- These longitudinal incisions are connected by convex upwards transverse incisions below the clavicles across the upper chest, and across the upper abdomen.
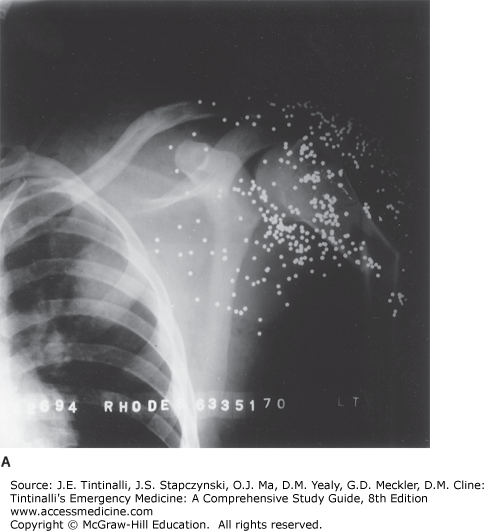
A pt who has sustained a shotgun GSW to his shoulder. He has received a CXR and shoulder XR. Evaluation of his wound is incomplete without these plain films.
What are xrays of distal extremity to rule out embolization of shotgun pellets?

This syndrome develops in patients 2-4wks after sustaining cardiac trauma and is characterized by chest pain, fever and effusions.
What is pericardial inflammation syndrome?
Delayed hypersensitivity reaction from damaged myocardium. May also have friction rubs, arthralgia, and pulmonary infiltrates.
The ECG will often show ST-T wave changes consistent with pericarditis.
Treatment is primarily symptomatic. Nonsteroidal anti-inflammatory drugs and rest can often reduce symptoms dramatically within 12 to 24 hours, and glucocorticoids are occasionally required.
A patient presents with a laryngotracheal injury. You attempt orotracheal intubation but fail. The patient is easily ventilated with BVM. This is the next preferred method of obtaining an airway.
What is tracheostomy?
Tracheostomy preferred surgical airway 2/2 risk of worsening laryngeal injury. However, situation may dictate what is appropriate.
These 3 blunt abdominal injuries are classically hard to diagnose on CT.
What are diaphragmatic, bowel, pancreas injuries?
A burn patient presents to your ED. She develops mydriasis and significant ST elevation. This treatment should be initiated for this suspected pathology.
What is hydroxycobalamin for cyanide poisoning?
- The spectrum of the clinical presentation of cyanide poisoning varies from mydriasis, to tachypnea and central apnea, to hypotension, to loss of consciousness and seizures
- Can see ST segment changes (elevation or depression)
- If concerned for cyanide toxicity, initiate 100% O2 therapy and administer hydroxocobalamin, with consideration for sodium thiosulfate (slower mechanism of action).
- Note: The commercially available cyanokit contains hydroxycobalamin.
An ABI below this number should concern you for severe or multiple segment arterial injury.
What is < 0.5.
0.5-.09: injury to single artery segment
ABI is up to 95% accurate to diagnose arterial injury, but largely variability with user.
A pt is in high speed MVC and strikes steering wheel with chest. Presents with unstable vitals. On physical exam you note what sounds like a splashing mill wheel, a physical exam finding termed "bruit de moulin" and denotes this traumatic cardiac injury.
What is cardiac rupture?

A patient presents after blunt thoracic injury with obvious right sided chest trauma. You suspect severe pulmonary hemorrhage. SpO2 is 52% with BVM. This is the emergent treatment for this condition.
Intubation with attempt to ventilate good lung.
Left sided- right mainstem
Right sided- more difficult
Double lumen endotracheal tube

This is the most common intra-abdominal injury from a fall from height.
What is hollow viscus rupture?
These are the 3 zones of a burn.
What is the zone of coagulation (tissue is irreversibly destroyed with thrombosis of blood vessels), the zone of stasis (stagnation of the microcirculation), and the zone of hyperemia (increased blood flow)?
Important to delineate between coagulation and stasis zones. Goal is to prevent conversion of stasis -> coagulation which can occur up to 48 hrs after burn.
ABIs are not effective in diagnosis this vascular injury.
What is pseudoaneurysm?