What was noted in our patients MRI findings?
*Bonus 100 pts: what was noted to be intact?
What are:
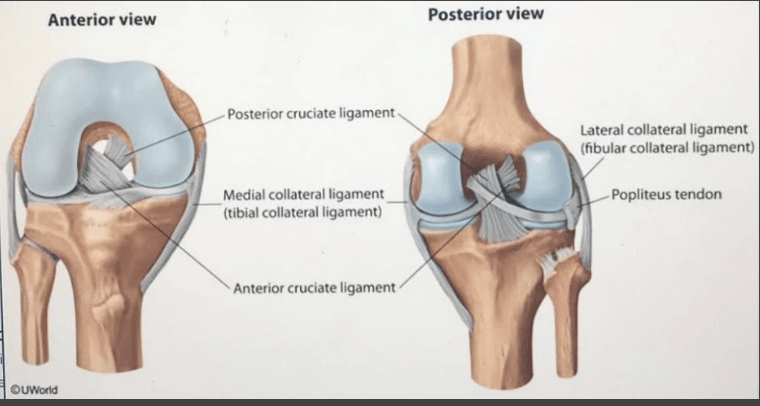
- Complete tear of ACL and PCL?
- Complete tear of MCL?
- Findings highly suspicious of horizontal tear of medial meniscus?
- Joint effusion?
Bonus:
What is lateral collateral ligament?
True or False
Consider this scenario:
Our same patient had a CT angiogram and no dissection, thrombosis, or thromboembolism were noted. Vascular pathologies no longer need to be monitored.
What is false?
Vascular surgery should be consulted in arterial injury identified. For patients without apparent vascular injury at the time of the initial evaluation, close surveillance, including daily vascular checks, must be performed for several days.
Popliteal artery lesion or thrombosis may not become clinically apparent for up to several weeks following the acute knee injury
What does it mean to reduce a joint?
What is the process by which a structure is brought back into its normal anatomic position?
What is the diagnosis in this image?

Tibiofemoral dislocation
Same as in our patient!

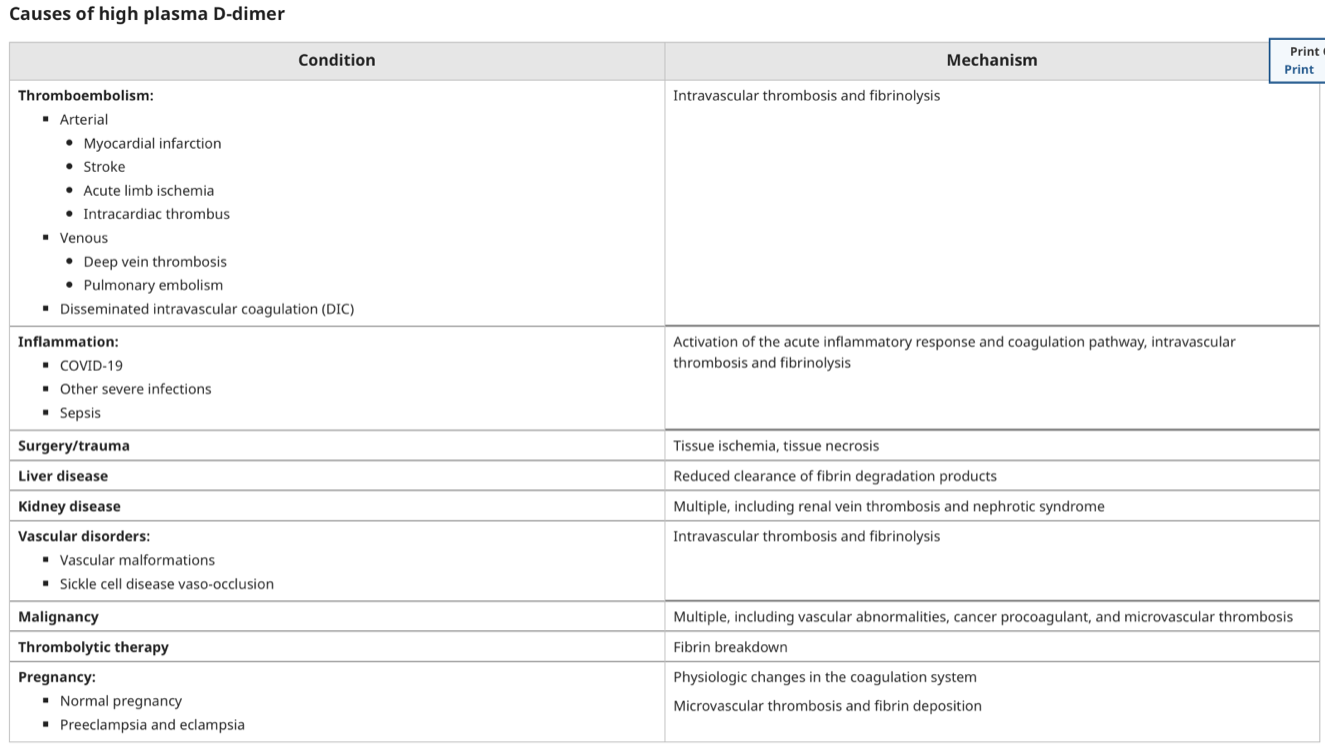
What are the indications for a d-dimer?
What are showing symptoms of blood clots?
Clinical uses of D-dimer include evaluation for: DVT, PE, DIC, Primary hyperfibrinolysis, prognostic assessment in COVID-19
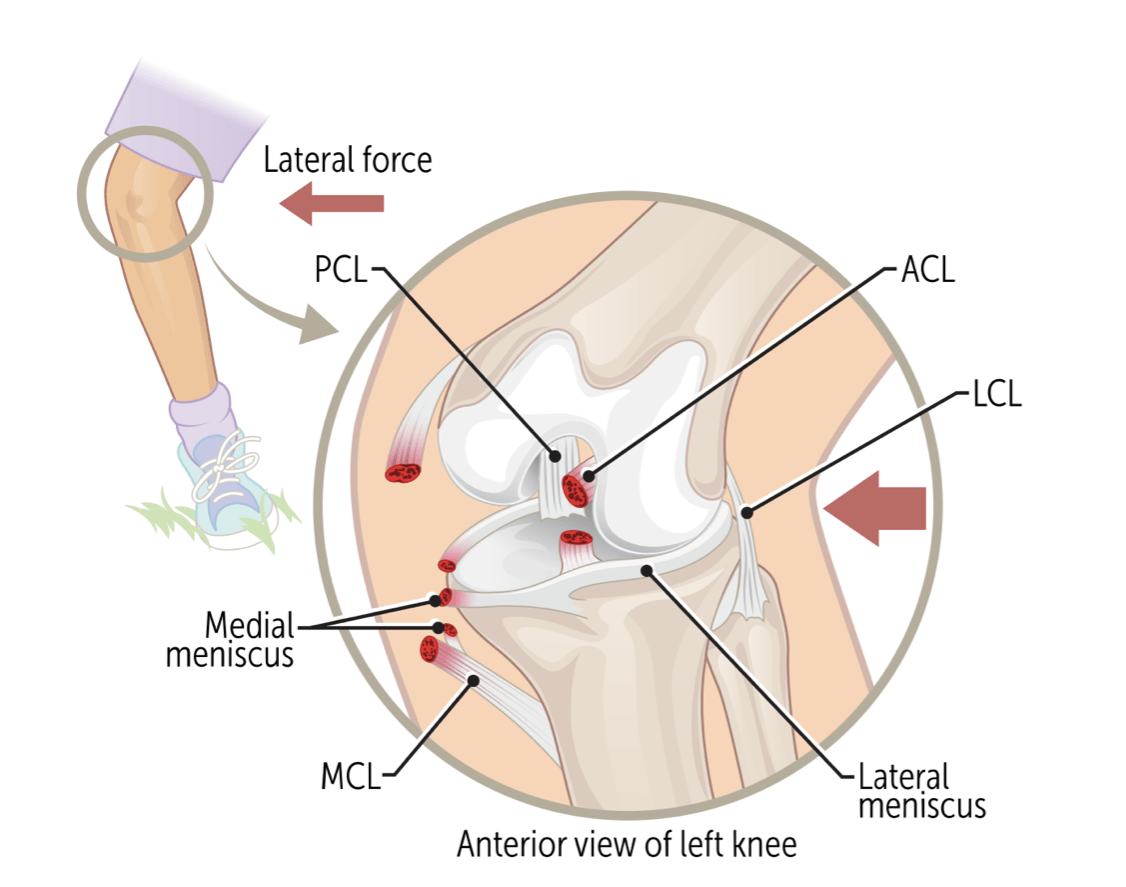
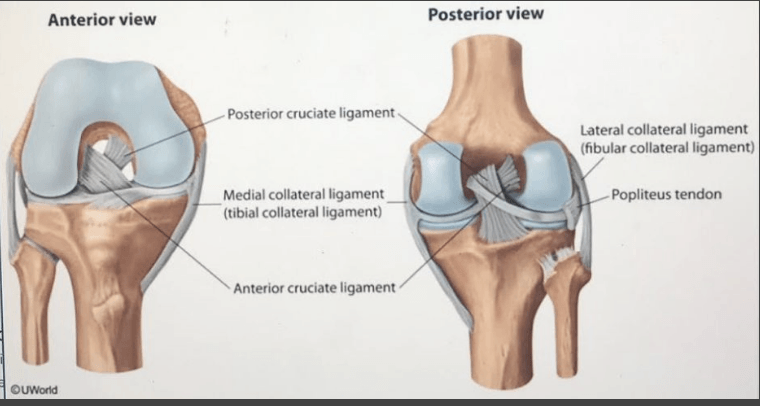
The Unhappy (Terrible) Triad involves damage to these structures.
What are the ACL, MCL and both menisci (more commonly the medial meniscus)?
All three are injured 50% of the time.
Treatment is usually surgery and requires a long recovery time.
What vascular injury of is associated with tibiofemoral dislocation?
What is the popliteal artery?
Up to 40% of patients with a knee dislocation will sustain a vascular associated injury.
Examination of distal and popliteal pulses is common in knee dislocations. Why?
What is to assess for limb-threatening ischemia?
Distal pulses, and popliteal pulses, should be assessed. Palpable distal pulse does not suggest the absence of vascular injury. Limb threatening vascular ischemia can result even in the presence of palpable distal foot pulses. The clinician should also assess for proper sensory and motor function though this can be somewhat limited by the pain and swelling associated with this injury.
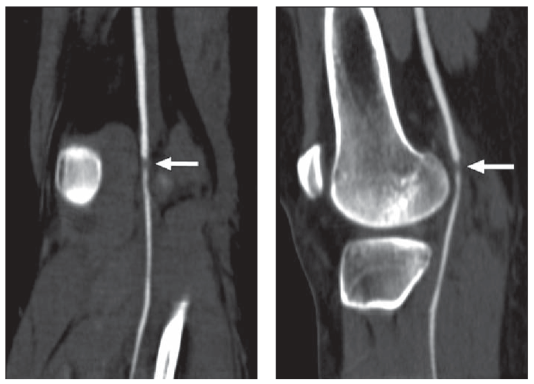
What kind of imaging is this? And what is the finding?
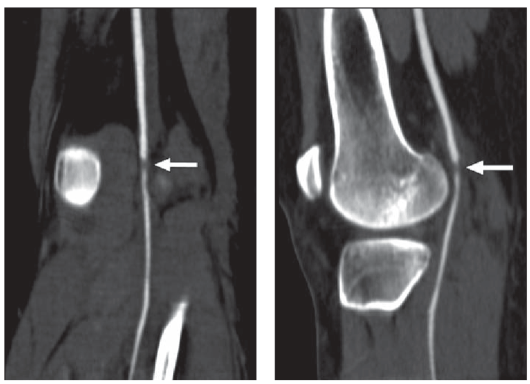
What is a CT angiogram?
What is a popliteal thrombosis?
Will this patient require an x-ray?
Tenderness and swelling of bony bridge of the nose with radiation
The patient can breathe through one nare
Obstruction present
The nose is slightly deviated
No septal hematoma is present
What is yes?
Nasal bone x-rays are unnecessary in the ED if the following criteria are met:
Tenderness and swelling are isolated to the bony bridge of the nose
The patient can breathe through each naris
No obstruction
The nose is straight (ie, no deviation of the septum)
No septal hematoma is present
CT scan is the preferred means of imaging facial trauma and should be obtained if concern exists about more extensive injury in the vicinity of the nose.
Septal hematomas are associated with necrosis of the septum if left untreated and should be drained as soon as possible, only requires drainage and packing
Fractures of the thin bones of the nasal bridge are common. Patients with a contusion or tenderness over the bridge of the nose may be assumed to have a fracture of the nasal bones. Imaging is often unnecessary
Perforated septal injuries may be identified during patient evaluation. They should be referred to an otolaryngologist for outpatient management within three to five days.
Generally, what structures in our patient require repair?
(Hint: here are the injuries
- Complete tear of ACL and PCL
- Complete tear of MCL
- Findings highly suspicious of horizontal tear of medial meniscus)
What are the ACL and medial meniscus?
Treatment of the unhappy triad depends on severity of the injury and the extent of damage to the surrounding structures. Patient activities and activities (e.g. sports) are also considered.
MCL responds well to non-surgical treatment.
PCL is usually allowed to heal on its own.
Immediately after a terrible triad injury, PRICE method as a form of conservative treatment to manage symptoms: Protection, Rest, Ice, Compression and Elevation
Physical therapy is an important part of the healing process and the PT would recommend a good regimen of sessions several weeks before surgery, and this continues after the surgery for 6-9 months, depending on the extent of the injury
A delay in diagnosis and repair of our patients popliteal thrombosis leads to prolonged ischemia. How many hours can a limb ensure ischemia until amputation is required?
What is eight hours?
Delay in diagnosis and repair increases the period of warm ischemia and the corresponding risk for irreparable injury requiring above the knee amputation. After eight hours of ischemia, the great majority of injuries will require amputation.
Which nerve can be damaged as a result of a tibiofemoral dislocation?
Peroneal nerve injuries can occur is > 20% of patients.
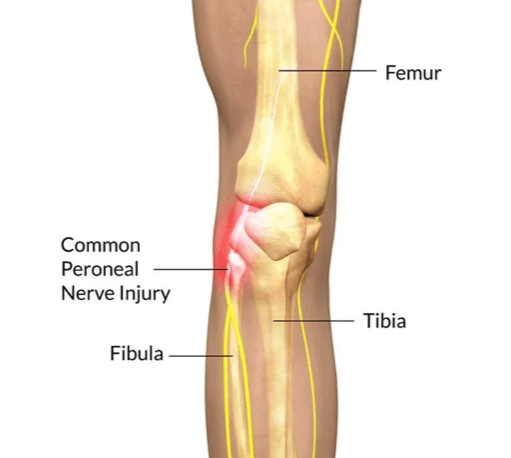
Mild symptoms include: numbness, tingling, pain and weakness of lower extremity.
More severe symptoms include: foot drop and limited foot/toe dorsiflexion
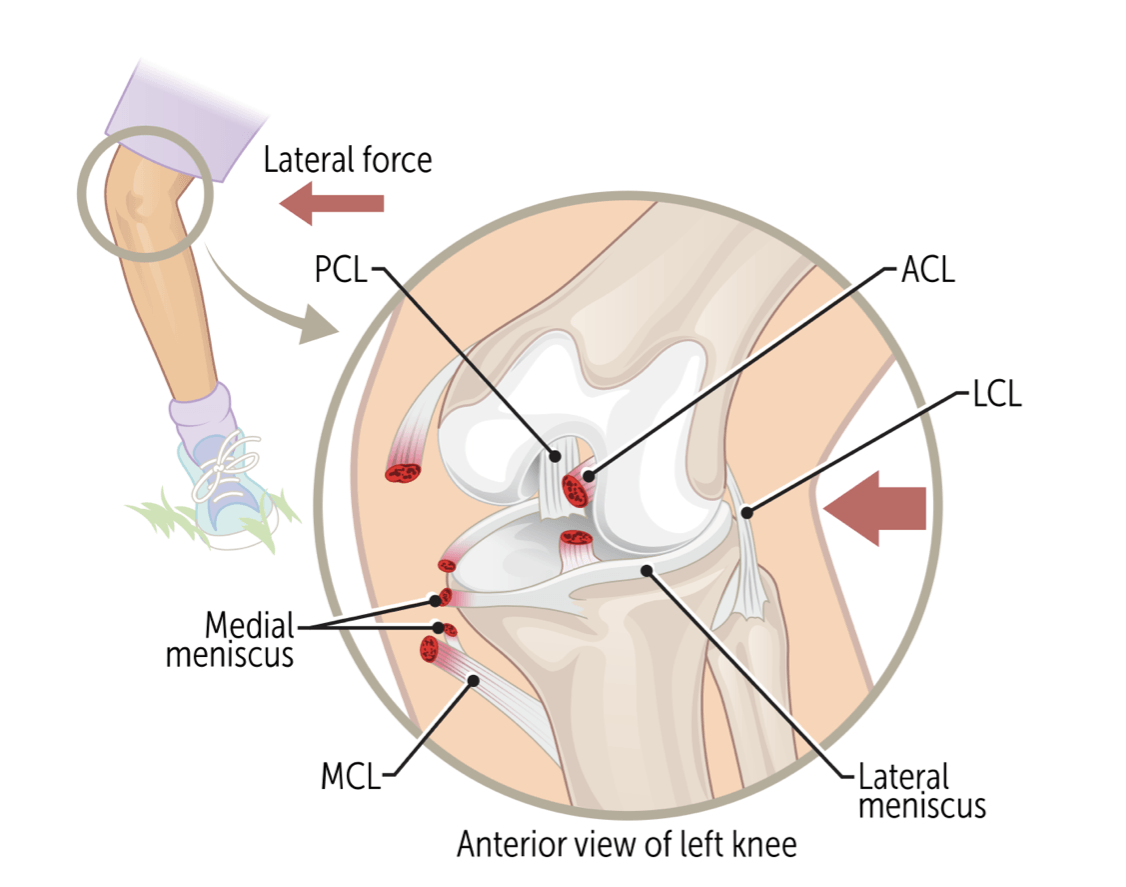
Identify the encircled structure:

*Bonus 100 pts: where does it specifically attach?
What is the posterior cruciate ligament (PCL)?
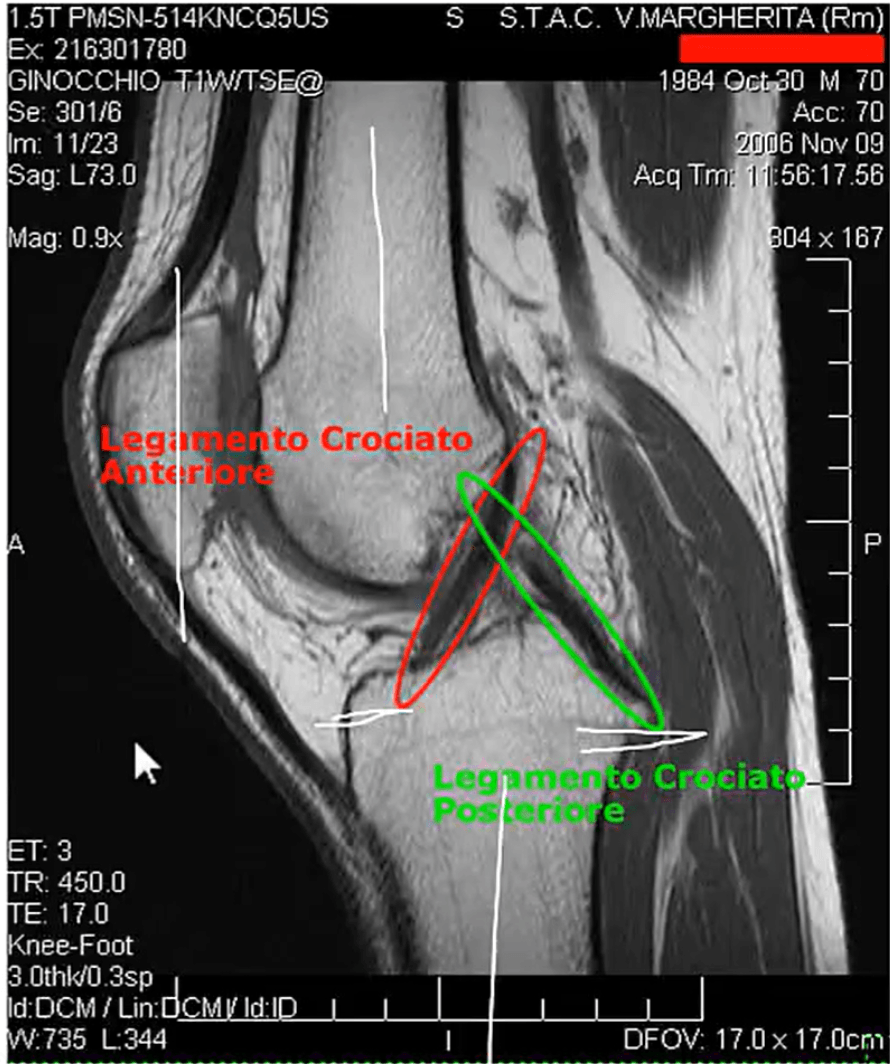
The PCL extends from the medial femoral condyle to the posterior tibia.
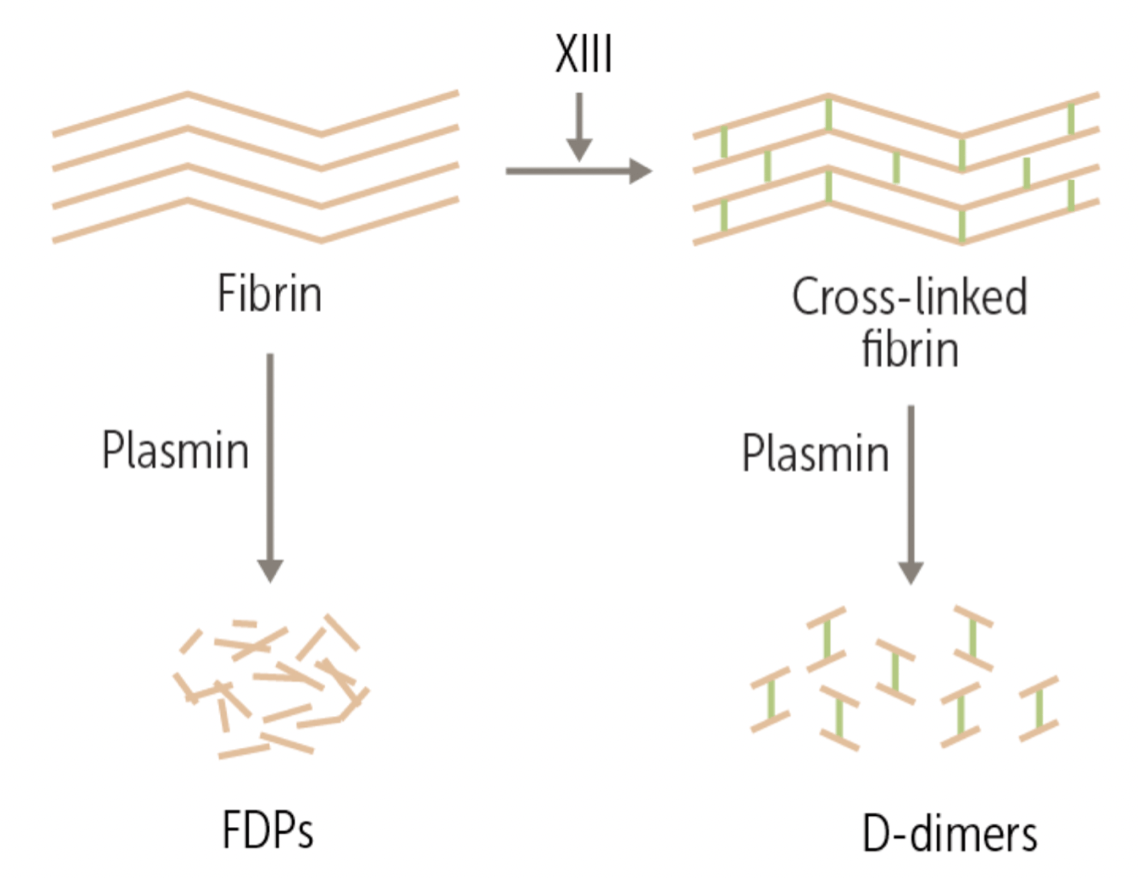
Mechanism of a D-dimer assay?
What is breaking down a clot - measure D-dimers, chunks of fibrin that have been crosslinked by factor XIII.
Fibrin d-dimer is one of the major fibrin degradation products released upon cleavage of cross-linked fibrin by plasmin. The dimer consists of two D domains from adjacent fibrin monomers that have been crosslinked by activated factor XIII.
What is the standard of care definitive surgery for an anterior cruciate ligament (ACL) repair?
What is graft selection?
Arthroscopy using a tendon graft to replace ACL
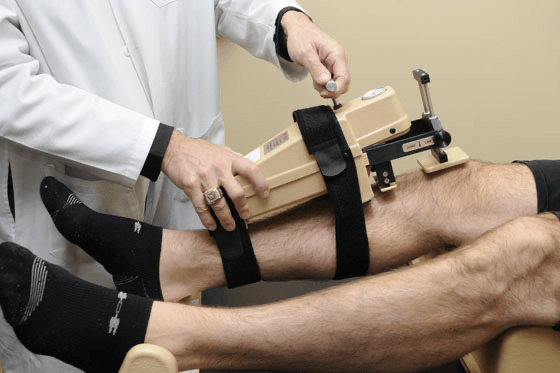
Traditionally, anterior translation of more than 5 mm with testing on KT1000 (objective measure anterior tibial motion relative to the femur for ACL – anterior drawer test?) or comparable device has been used as criterion for surgery. Some experts believe that a positive pivot shift test three months following injury is the best predicitve measure for need of surgical repair.
Acute management: rest ice, compression of the injured knee, and elevation of the affected lower extremity. Crutches, OTC analgesics, NSAIDS.
Injury risk associated with non-operative management: osteoarthritis, subsequent knee injury
Arterial injury due to traumatic posterior knee dislocations can lead to acute lower extremity ischemia. In our patient, Sasha, what was the most-likely mechanism of this ischemia?
What is traumatic arterial dissection with subsequent thrombosis.
The ischemia leads to the diminished values in the distal and popliteal pulses found on physical examination.
What is the Ankle Brachial Index (ABI) used for?
What is to determine for lower extremity arterial stenosis or occlusion?
Procedure: measure BP, inflate cuff until BP on doppler signal disappears. Release pressure in cuff until signal returns using continuous wave doppler.
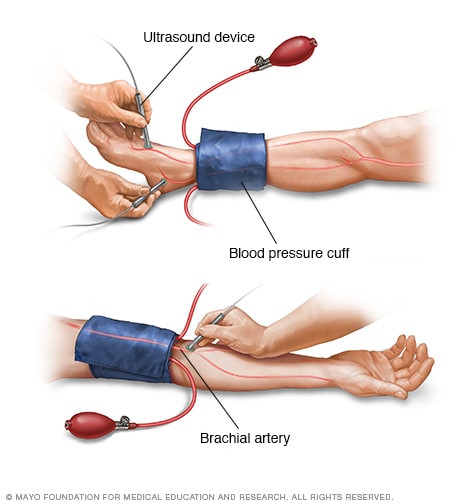
The ABI measurement is a ratio of lower extremity perfusion (posterior tibial and dorsalis pedis arteries) and upper extremity perfusion (brachial artery).
An ABI of 0.9 or greater is considered normal, while an ABI less than 0.9 can indicate a vascular compromise.
Identify the encircled structure:

*Bonus 100 pts: where does it specifically attach?
What is the anterior cruciate ligament (ACL)?
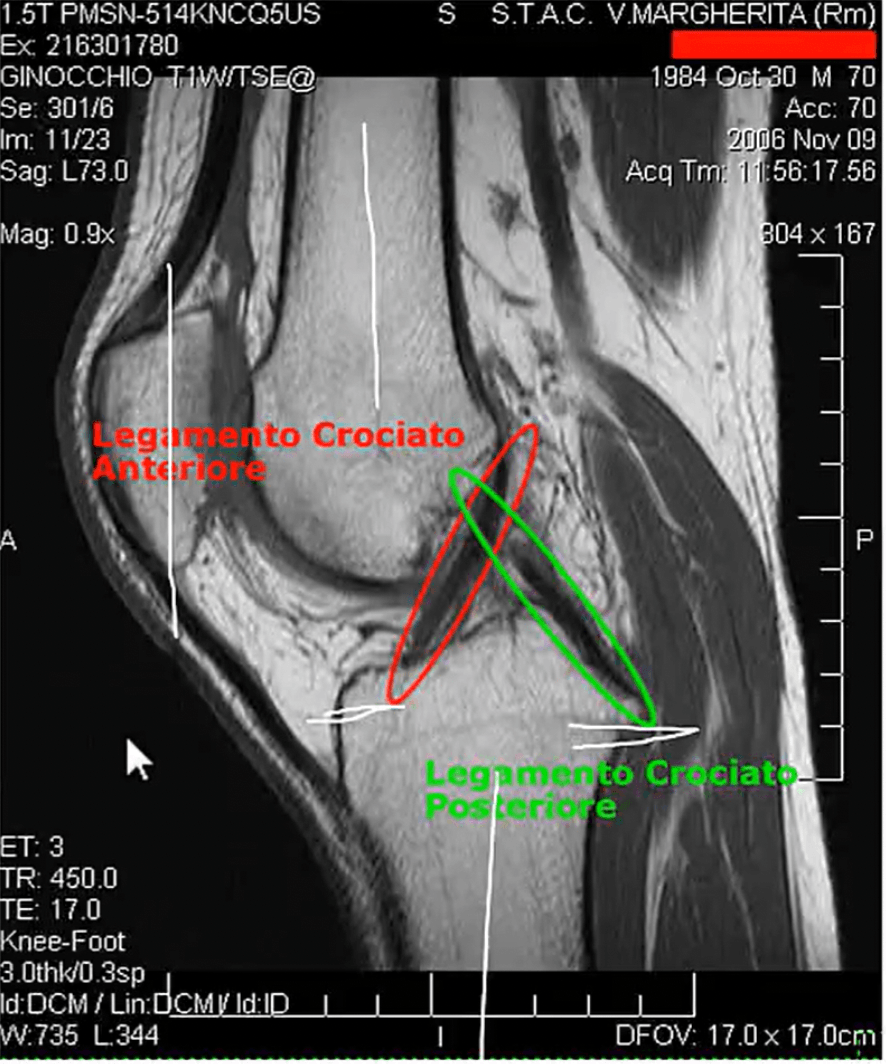
The ACL extends from the lateral femoral condyle to the anterior tibia.
What is a common finding in patients with meniscal tears?
What is an effusion?
An effusion may be detected in patients with meniscal tears, particularly large or complex tears. Small effusions will fill the peripatellar dimples with the knees extended and quadriceps muscles relaxed. Milking the knee detects highly viscous effusions. The ballottement sign is positive when there is at least 10-15 mL of intraarticular fluid. Large effusions fill the suprapatellar space.
What is the standard of care definitive treatment for a meniscal tear repair?
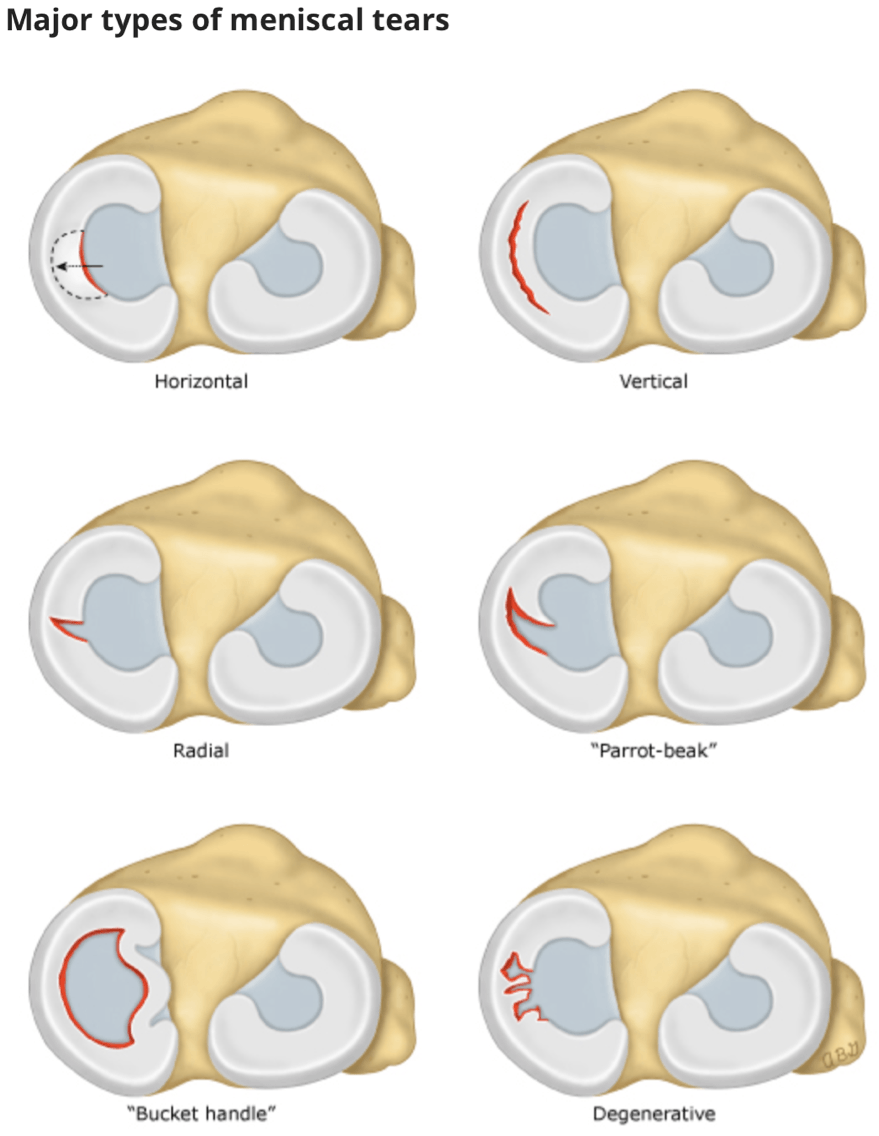
What are partial or total meniscectomy?
Open or arthroscopic surgery can be performed. An important surgical principle when performing a meniscectomy is to retain as much functioning meniscus as possible.
Partial meniscectomy performed arthroscopically is the preferable owing to the speed of recovery and overall functional outcomes
Surgery is required for patients with: severe twisting injury and activity can be resumed after; the knee is locked or motion is severely restricted; pain develops with Mcmurray testing involving minimal knee flexion; an associated anterior cruciate ligament tear exists; there is little improvement in symptoms after 3-6 weeks despite proper conservative treatment
McMurray test for meniscal injury:
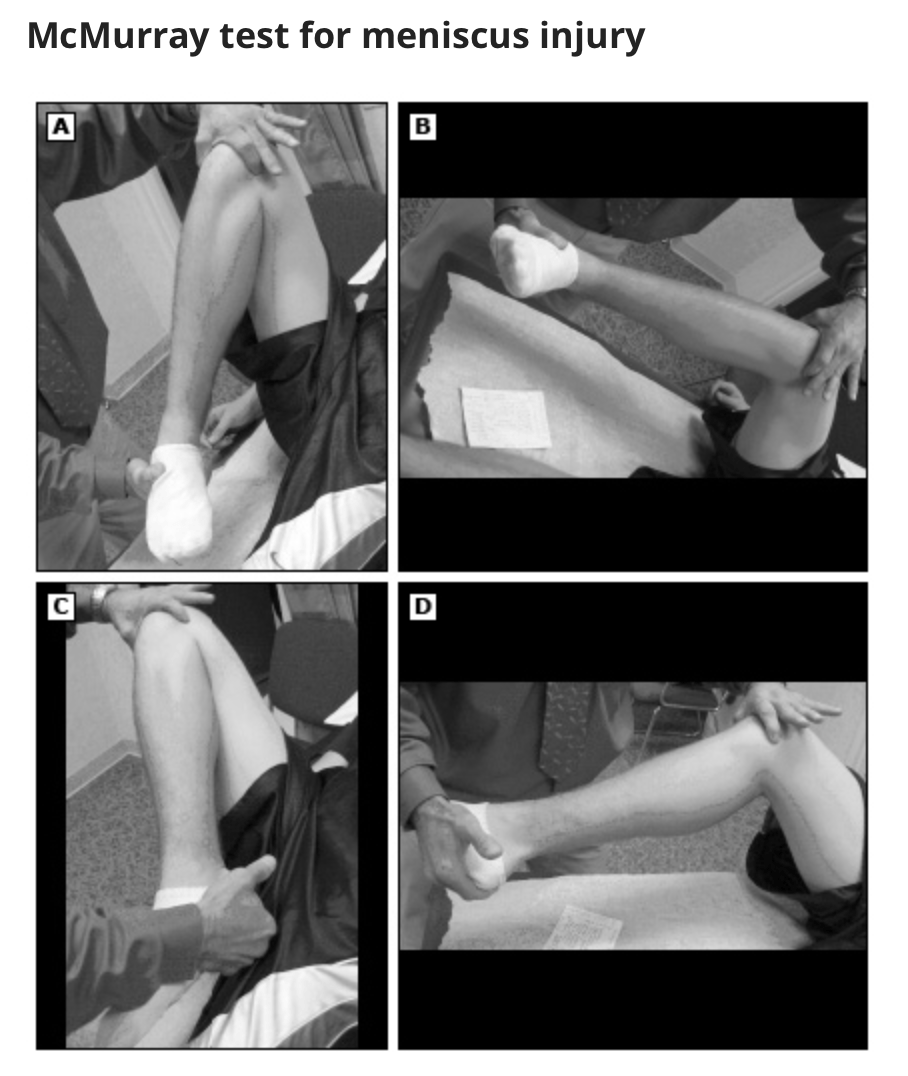
To perform maneuver, the examiner places their thumb and index finger on the medical and lateral joint lines while the knee is passively flexed and extended several times in a smooth back and forth motion. Flexion and extension is performed with the tibia internally rotated for several repetitions (A and B), and then with the tibia externally rotated for several repetitions (C and D). While performing the maneuver the clinician feels for a popping sensation along the joint line. The test is positive when there is pain at the joint line, with or without a “clunk,” and possibly limited range of motion. A positive test suggests meniscal injury.
Name at least one option for vascular surgical treatment for a partial popliteal occlusion?
What are:
- surgical bypass: graph used to bypass the occlusion site?
- endarterectomy: surgical removal the blockage plus part of the inner lining (intima) of the artery, followed by stenting to support the walls of the artery?
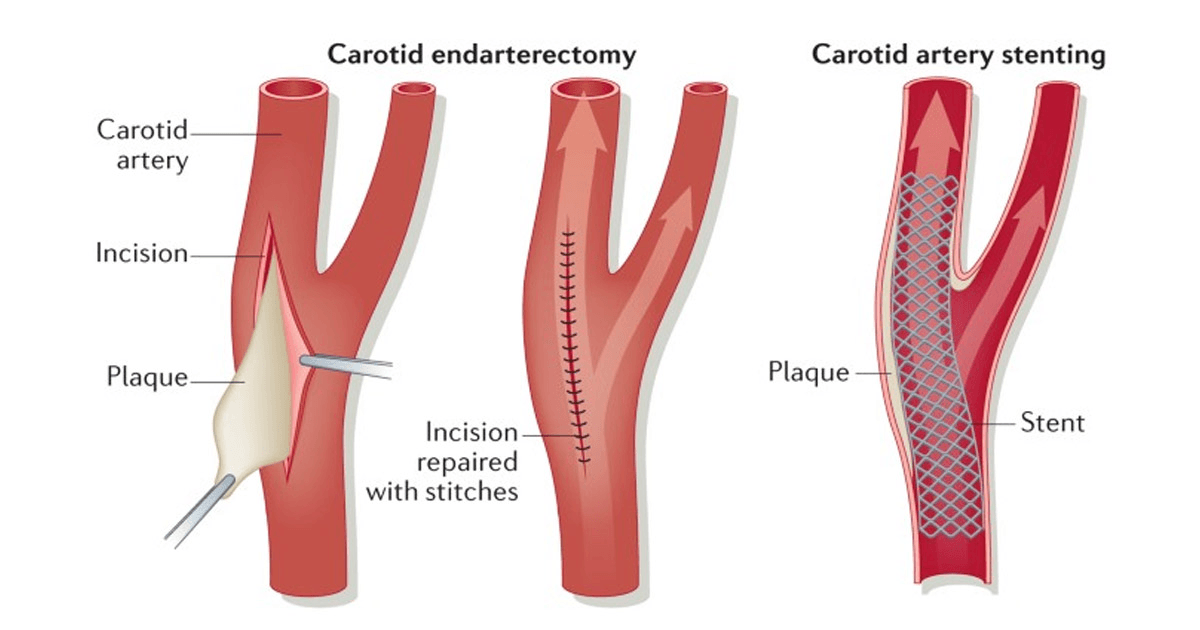 - Embolectomy (thrombectomy): removal of the clot?
- Embolectomy (thrombectomy): removal of the clot?
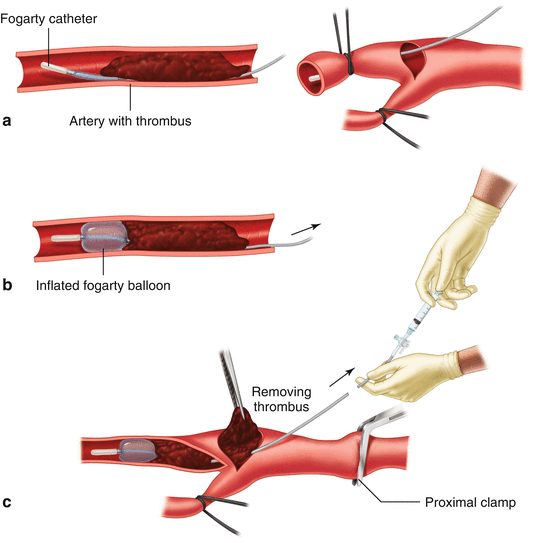
- Catheter directed thrombolysis (IR)?
Early therapy prevents long term complications like limb loss.
After working up your patient that sustained a tibiofemoral dislocation you note these findings:
- Well perfused limb
- asymmetric pulses
- ABI <0.9
- abnormal duplex ultrasound
What are your next steps?
What is:
Obtain urgent arteriogram or comparable vascular study (e.g. CT angiogram) in consultation with vascular surgery?
If weak or absent pulses and signs of ischemic limb or vascular injury, then emergency vascular surgery consultation or operative surgery are required.
The following is a doppler study. What do you see?
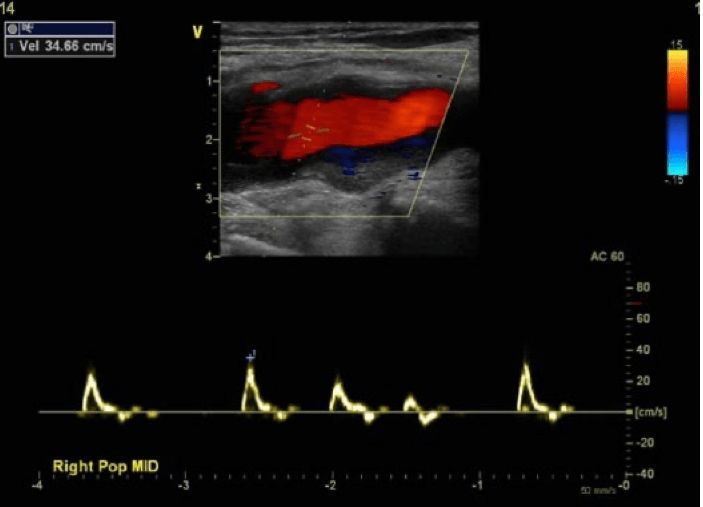
What is a color and spectral Doppler image taken at the site of maximal right popliteal artery aneurysmal dilation showing mural thrombus but no evidence of significant obstructive disease and an essentially normal triphasic spectral Doppler signal.
https://www.youtube.com/watch?v=bAHGJk8PQIs
DAILY DOUBLE (1000 pts)
What receptors do:
- ketamine bind to?
- morphine bind to?
What are:
- NMDA receptors?
- opioid receptors?
Ketamine
- NMDA Receptor antagonist and blocks glutamate from binding
- Low doses (IV method) it is used as analgesia
- Higher doses induce anesthesia
Morphine
- Binds to opioid receptors in CNS to induce inhibition of pathways and alter response to pain
- Used for pain management and for critically ill patients