Which of the following entities exerts its predominant pathologic effect at the site marked with the arrow?
A) Myasthenia Gravis
B) Guillain Barre
C) Aminoglycosides
D) Botulism
E) Tick Paralysis
A) Myasthenia Gravis
B) Guillain Barre
C) Aminoglycosides
D) Botulism
E) Tick Paralysis
This neurodiagnostic study can be considered when myasthenia gravis is considered high on a differential diagnosis.
repetitive nerve stimulation
T/F: Research has shown administration of fingernail polish (formaldehyde, toluene, and dibutyl phthalate) prior to removal of an embedded tick decreases toxin release.
False
Mainstays of therapy for GBS include the following:
A) IVIG
B) Pulse Dose Steroids
C) Plasmapheresis
E) Monoclonal antibody therapy
A) IVIG
B) Pulse Dose Steroids
C) Plasmapheresis
E) Monoclonal antibody therapy
Acetylcholine (ACh) is the primary neurotransmitter of the parasympathetic nervous system. ACh stimulates which two types of receptors in the parasympathetic nervous sytsem?
What are muscarinic and nicotinic.
A parent reports their recently admitted child (transferred from an outside hospital with respiratory failure) seemed okay during the morning over the last few weeks but became more fatigued as the day progressed. You ask you medical student which medication could be utilized to assist in the patients diagnosis.
What is edrophonium (or neostigmine).
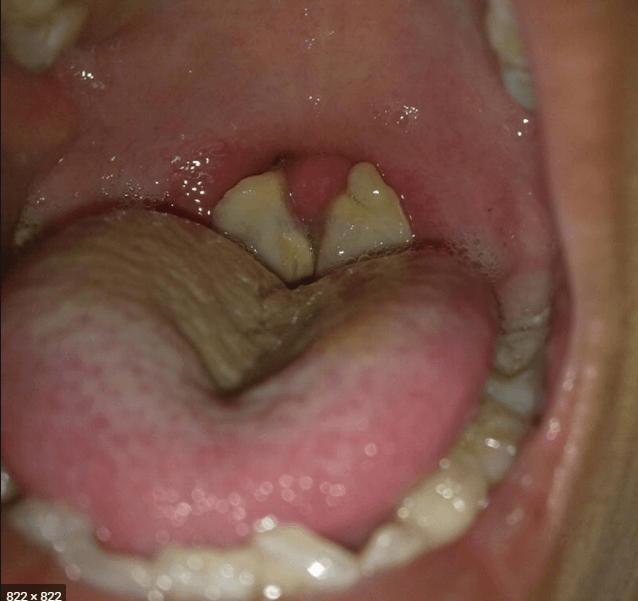
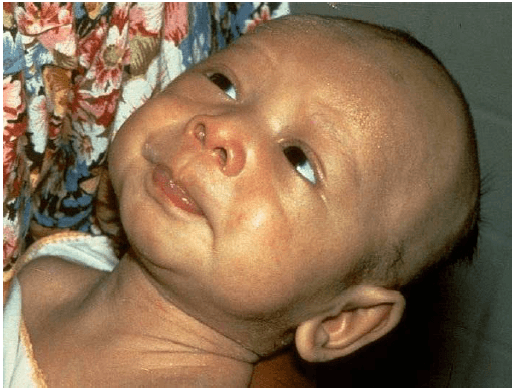
This physical exam finding is associated with what diagnosis?
What is Spinal muscular atrophy
Which of the following findings would not be expected in a patient with a lower motor neuron lesion?
A. Flaccidity
B. Depressed tendon reflexes
C. Absent deep tendon reflexes
D. Fasiculations
E. Muscle Hypertrophy
Muscle Hypertrophy
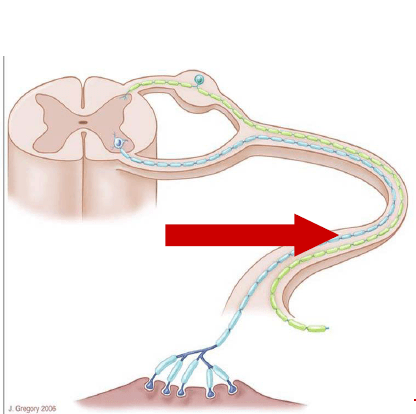
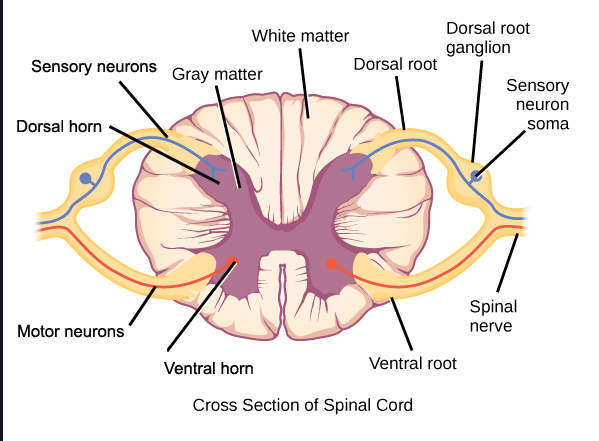
You have a 9 month old patient who comes in with new onset weakness. He has a poor suck, a weak cry, and enlarged, sluggishly reactive pupils. Where in the diagram above is the likely etiology of his disease process?
a) 1
b) 3
c) 5
d) 7
D- this infant has classic signs of infant botulism, caused by ingestion of botulinum spores which subsequently germinate and produce toxin. Botulinum toxin works by inhibiting fusion of the vesicle containing Ach with the presynaptic membrane, thus preventing release of acetylcholine to propagate muscular contraction. Hence, "7" is the correct answer.
Spinal Muscular Atrophy is associated with a mutation of this gene.
Survivor Motor Neuron gene (which is associated with halting apoptosis)
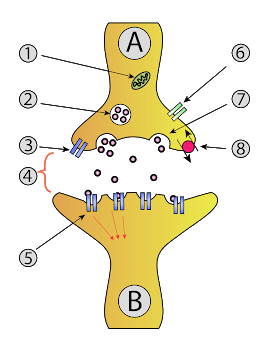
This is the typical time to recovery for patients with tick paralysis following removal of the tick.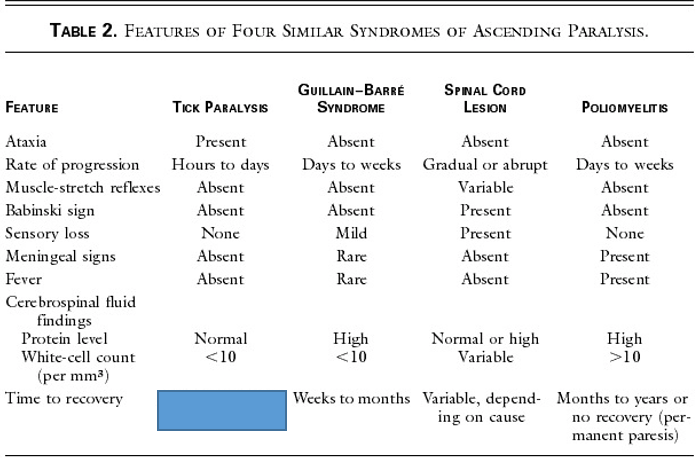
What is less than 24 hours.
This treatment has been shown to significantly decrease the length of hospital stay, duration of mechanical ventilation, and duration of either parenteral and/or NG nutrition in infants with botulism.
botulism immune globulin (BIG)
Avoidance of this class of antibiotics should be heeded in patients with myasthenia crises.
aminoglycoside
In the ED, you assess a high school football player with trouble walking. He reports he consumed a large meal of spaghetti followed by a nap. Shortly after waking from his nap, he noted reports that his legs felt weak. You suspect a derangement of this electrolyte.
What is hypokalemia.
In addition to experiencing weakness, infants with botulism often experience symptoms related to dysregulation of this component of the nervous system. Sequelae include constipation, tachycardia, fluctuating blood pressure, urinary retention, decreased tears or saliva, and/or flushed skin/pallor.
Autonomic nervous system: botulism toxin also binds at ACh mediated preganglionic parasympathetic and sympathetic synapses, as well as postganglionic parasympathetic synapses.
Upon performing a lumbar puncture on a patient your team highly suspects has GBS, your medical student is disappointed to see that there is no evidence of albuminocytologic dissociation. How long (in general) after symptoms of GBS are noted do you typically see albuminocytoligic dissociation in the CSF?
1 week +
The following are muscle biopsy slides. The first image was taken from a normal 3 yr old. The two slides to the right were taken from a 3yr old and 9yr old with a disease process caused by a mutation in what gene?
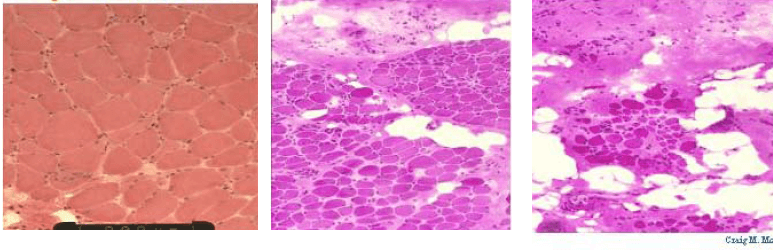
What is the dystrophin gene?
Absent or decreased function of dystrophin leads to cycles of muscle fiber degeneration and regeneration
- this subsequently leads to fatty replacement and a distorted fascicular architecture
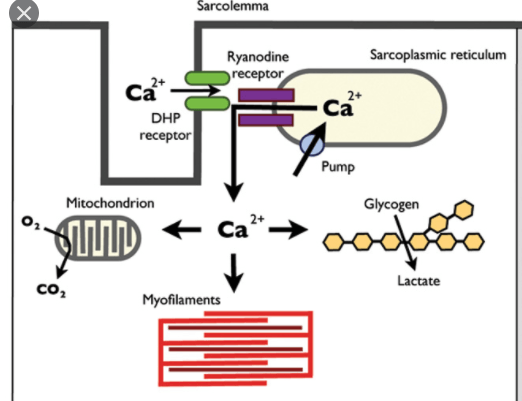
Ryanodine receptor
The pathophysiology of tick paralysis is due to a neurotoxin that has this effect at the neuromuscular junction.
What is inhibition of release of acetylcholine.
When administering a trial dose of short-acting anticholinesterase to a patient with suspected myasthenia gravis, you should have a dose of this medication prepared to address potential side effects (name of medication and primary side effect required)
atropine/bradycardia
*Edrophonium is an intravenous short acting anticholinesterase (Tensilon challenge)
What feature of the infant intestinal track places them at particular risk for bolulism?
Spores ingested, germination occurs, and toxin causes symptoms. Lack of competitive intestinal flora allows spores to germinate in infants.
While relatively uncommon, confirmed cases of this condition rose during summer/fall months from 2014-2018. Symptoms including fever, cough/congestion, rhinorrhea, vomiting/diarrhea often preceded development of weakness in one or more limb(s). Cranial nerve dysfunction and AMS were less common.
What is Acute flaccid myelitis. Classically associated with Enterovirus D68.
While on an oversees medical trip to the Ukraine you encounter a child with difficulty swallowing and a history of ascending weakness. What is the diagnosis?
Diptheria
What is GBS
A patient comes in to clinic for follow-up of a known neuromuscular disorder. She is treated with daily pyridostigmine, which improves her symptoms of generalized weakness, ptosis, and fatigability. Where in the diagram above is the likely etiology of her disease process?
a) 2
b) 3
c) 5
d) 6
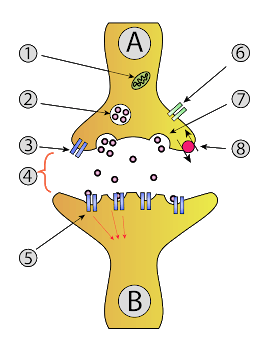
C- this patient has myasthenia gravis, caused by antibodies which attack the Ach receptor at the postsynaptic membrane. Myasthenia gravis is treated using Acetylcholinesterase inhibitors such as pyridostigmine. Hence, "5" is the correct answer.
An adolescent female presents to the ED with complaints of colicky abdominal pain and back pain. In triage she had a brief seizure. On your exam, you note she has diminished strength in her upper extremities. This is the urine test will likely yield a diagnosis.
Urine Porphobilinogen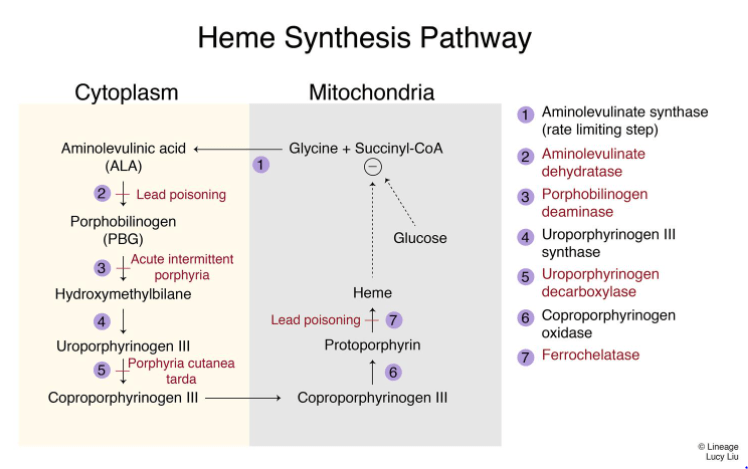
The onset of symptoms often occurs this many days after tick attachment.
What are 5 days.
Which of the following agents is NOT known to exacerbate neuromuscular weakness?
a) methylprednisone
b) rocuronium
c) aminogylcosides
d) cephalosporins
D- all the other agents are known to exacerbate neuromuscular weakness and should be used with caution in patients with neuromuscular weakness. Cephalosporins, in contrast to aminoglycosides, are not thought to exacerbate neurmouscular weakness.
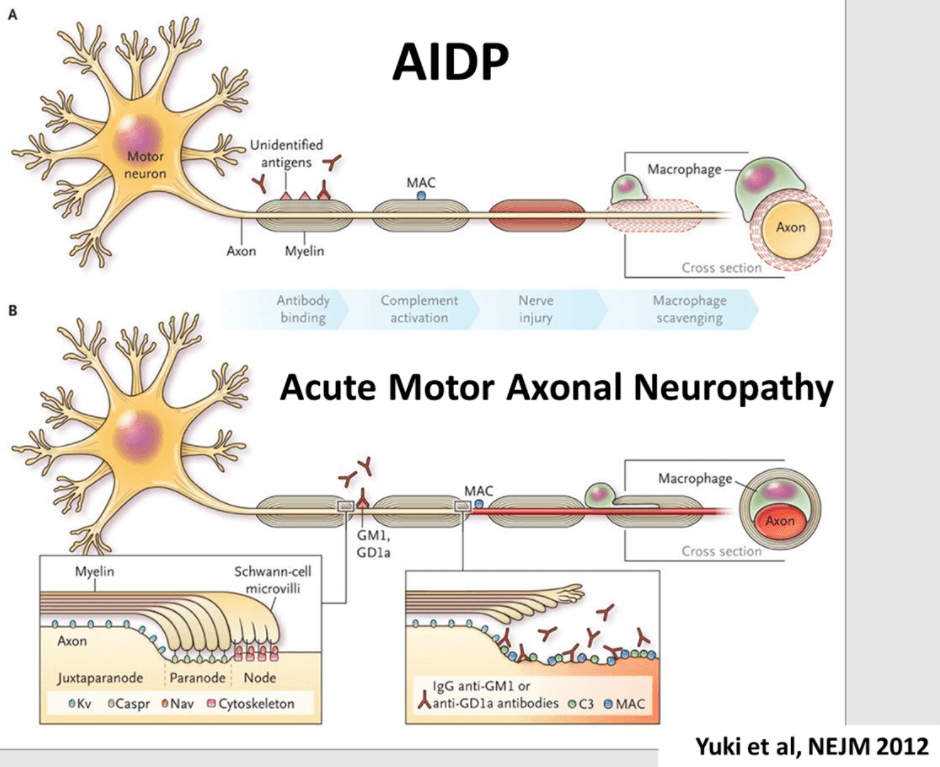
The most common North American form of GBS is Acute inflammatory demyelinating polyradiculoneuropathy (AIDP). Subtypes of GBS include Acute motor axonal neuropathy (AMAN) and Miller Fisher variant. How does the pathophysiology of AMAN vary from the more classic form of GBS, AIDP?
A 13yo female presents to the ED with diffuse myalgias and weakness. Earlier in the day she participated in a school field day. Her parents note she tends to avoid strenuous exercise as she says it makes her feel bad for several days after. The ED nurse notifies you her urine is a dark red color. Initial lab-work reveals a CK of >400,000UI/L. Genetic testing for this disorder should be considered in her work-up.
McArdle's disease (glycogen storage disease Type V)
This boy's skin features can be seen in children with this underlying disorder which is characterized by symmetrical proximal muscle weakness, a scaly rash involving the elbows, neck, upper torso, and elevated CPK (name the disease process).
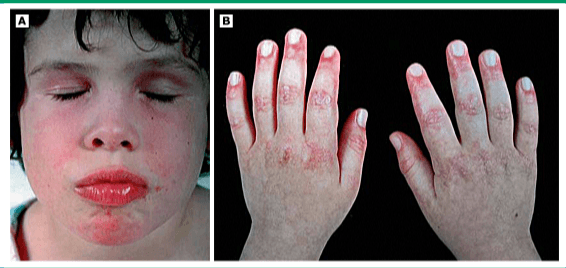
What is Dermatomyositis
(A) Heliotrope discoloration of the eyelids and malar or facial erythema.
(B) Scaly, red rash on the knuckles with Gottron papules (erythematous, papulosquamous eruption over the dorsal surfaces of the knuckles).
This medication may be used for prophylaxis in patients with periodic paralysis.
Acetazolamide
This characterstic facial expression is due to sustained muscle spasm of the facial muscles due to tetanus.
What is risus sardonicus
Workup of patients with concern for acute flaccid myelitis often includes:
MRI of the cervical and thoracic spine
CSF analysis
Nasopharyngeal swabs for viral testing
Serum tests for potential mimics (e.g. anti-myelin oligodendrocyte glycoprotein antibodies)
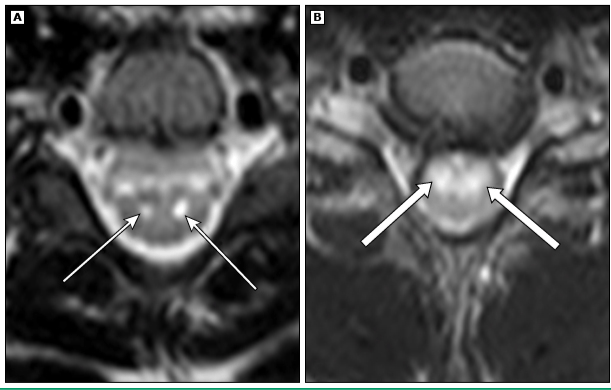
The primary spinal cord MRI abnormality is:
Hyperintensity of the central gray matter.
These two types of ticks are the most common culprits of tick paralysis in North America. An image of one of them is below:

Dermacentor andersoni (wood tick)
Dermacentor variabilis (dog tick)
Treatment of organophosphate poisonings involves use of medications to treat the muscarinic and nicotinic side effects. Nicotinic side effects include muscle weakness and respiratory failure. This medication is used to address the nicotinic side effects.
What is pralidoxime (cholinesterase reactivator) Pralidoxime reactivates acetylcholinesterase, provides endogenous anticholinergic effects, and detoxifies unbound organophosphates.
*atropine is the antidote for muscarinic side effects (bronchorrhea, salivation, tearing and sweating, bronchoconstriction, tightness in the chest, wheezing, bradycardia, vomiting, increased gastrointestinal motility, abdominal tightness, diarrhea, and cramps )
Hyokalemic periodic paralysis is most commonly due to a mutation in this skeletal muscle receptor.
What is the dihydropyridine receptor in voltage sensitive Ca channel. Another common mutation is SCN4A (voltage sensitive sodium channel)
*most cases of HypoKPP are hereditary (autosomal dominant with incomplete penetrance); acquired cases are associated with hyperthyroidism
* It is postulated that triggering factors cause a rise in plasma epinephrine level or insulin level, causing an intracellular shift of potassium, resulting in lower serum potassium level, thus triggering the episode of weakness
A young child in brought to the ER after his mother found him on the ground in the garage. His exam is notable for presence of an unpleasant odor and muscle fasciculations. You also note excessive drooling and pinpoint pupils. You're unable to elicit reflexes. Inhibition of this enzyme is responsible for findings related to the poisoning in this case.
What is cholinesterase (organophosphates irreversibly bind cholinesterases, carbamate compounds reversibly bind cholinesterases).
The Miller-Fisher variant of GBS is characterized by a triad of abnormal neurologic findings which include:
-ataxia
-areflexia
-opthalmoplegia
Antibodies against GQ1b, a ganglioside component of nerve, are present in the vast majority of patients with Miller Fisher syndrome.
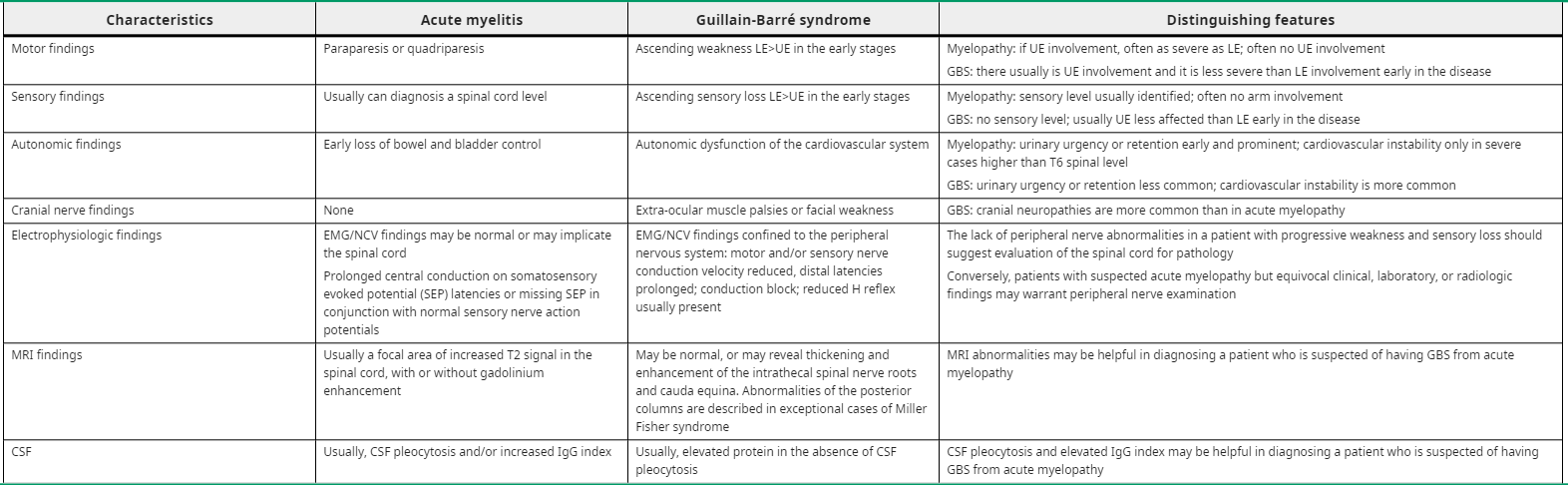
Distinguishing GBS from transverse myelitis can be difficult. These two disease processes tend to have characteristic types of dysfunction of the autonomic nervous system. Autonomic dysfunction in GBS is likely to involve _________ instability while autonomic dysfunction in transverse myelitis often involves _________________.
GBS - cardiovascular instability
TM - urinary or bowel urgency or retention