This is the most common congenital heart defect, affecting approximately 1.5 to 3 out of every 1,000 term infants.
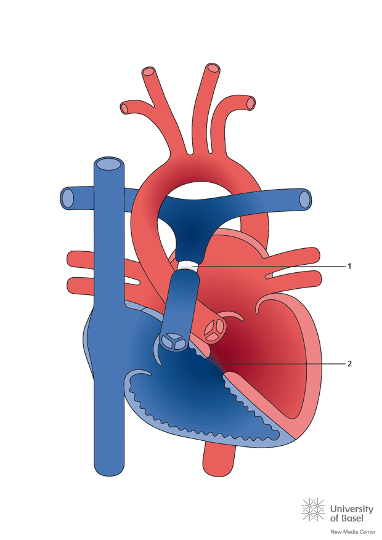
What is a ventricular septal defect (VSD)?
The difference between a restrictive and a non restrictive VSD is
Restrictive VSD: The defect is small enough that it limits (or "restricts") the amount of blood flow between the ventricles. This results in a pressure difference between the left and right ventricles. The left ventricle maintains higher pressure, and the shunt is typically left-to-right, causing relatively mild symptoms. Pulmonary pressures remain low.
Non-restrictive VSD: The defect is large, allowing equalization of pressures between the left and right ventricles. This means that the shunt is significant, and both ventricles share the same pressure. This can lead to high pulmonary blood flow, pulmonary hypertension, and heart failure. Eventually, this may cause right-to-left shunting and cyanosis.
This complication is often seen post-surgery for perimembranous VSD
What is complete heart block (AV block)?
2 month old Trisomy 21 with complete AV canal for emergency exploratory laparotomy. Baseline vital signs: HR 170 SpO2 98% BP 71/50
Echo with balanced complete AV canal, normal biventricular function, RVH, large ASD, large VSD, mild AVVR.
What would your goals for induction would be
Preload
Contractility
Afterload
Rhythm and Rate
PVR
Preload: Normal to mildly high
Contractility: Normal
Afterload: Normal to low, patient is overcirculating
Rhythm and Rate: Sinus, Normal HR for age. Do can
PVR: Aim for normal to high to avoid overcirculation
Patients with this advanced condition and markedly increased pulmonary vascular resistance are typically not candidates for VSD closure due to the risk of significantly increasing right ventricular afterload.
What is Eisenmenger's syndrome?
This is the most common type of VSD
What is perimembranous VSD?
These defects comprise approximately 80% of all VSDs, and are located in the subaortic region of the membranous septum.
These defects are commonly partially closed by a collection of tricuspid valve and membranous septal tissue, which gives an aneurysmal appearance to the septum.
Infants with a large VSD may present this condition when the pulmonary vascular resistance decreases
What is pulmonary overcirculation?
These echocardiographic parameters are important to determine perioperatively
•type, number, size, shunt
•direction, and assessment of adjacent structures.
3 yo with large VSD, SOB, pulmonary edema. Baseline vital signs: HR 130 SpO2 98% BP 80/50
Echo with decreased LV function, EF 45%, RV dilation, borderline RV function, moderate perimembranous VSD. No signs of pulmonary hypertension.
What would your goals for induction would be in terms of:
Preload
Contractility
Afterload
Rhythm and Rate
PVR
Preload: Normal to low
Contractility: normal to high in the setting of low EF
Afterload: Normal to maintain Qp:Qs 1:1
Rhythm and Rate: Sinus, normal rate for age
PVR: Normal to high to avoid pulmonary over circulation.
Non-operative closure of muscular VSDs can be achieved with...
And what are the most common complications?
What is a closing device?
What is an Amplatzer?
Complications: Arrythmias (CHB), device embolization, residual shunt/hemolysis
This type of VSD can close spontaneously and is often found in the lower part of the ventricular septum.
What is muscular VSD?
Over time, pulmonary over circulation may lead to endothelial changes leading to the development of this condition.
What is pulmonary hypertension?
•residual septal defects or patch integrity (associated aortic regurgitation, outflow tract obstruction, and hemodynamicsignificance)
•Residual VSDs measuring 3 to 4 mm require careful analysis including measurement of Qp:Qs byechocardiographic or blood oxygen saturation analysis to better determine need of return to bypass.
•A Qp:Qs of > 1.5:1 or a residual VSD >4 mm should have an additional attempt(s) at closure in most cases.
•PA pressures
•ventricular function
•device configuration in interventional cases
1 month old
•Hypoplastic transverse aortic arch with coarctation of the aorta, large perimembranous VSD, additional small mid muscular VSD and concern for VACTERL who is now s/p aortic arch repair/coarctectomy/ligation and division of PDA.
Echo with RVH, RV dilation, normal biventricular function.
•Today for VSD repair, MPA band take off, PA plasty
What are your goals for induction:
Preload
Contractility
Afterload
Rhythm and Rate
PVR
Preload: normal to high
Contractility: normal to high
Afterload: Normal to maintain a Qp:Qs of 1:1
Rhythm and Rate: sinus, normal HR for age
PVR: Necessary to achieve a Qp:Qs 1:1
In certain cases, particularly in infants, palliation with this technique may be preferred over left ventriculotomy to manage small muscular VSDs.
What is pulmonary artery banding?
This VSD is located near the atrioventricular valves and is commonly associated with atrioventricular canal defects.
What is inlet VSD?
This syndrome occurs when long-standing, untreated large VSDs cause high pulmonary vascular resistance and a reversal of the shunt to right-to-left."
What is Eisenmenger syndrome?
Surgical correction of atrioventricular canal defects may lead this arrhythmia
Junctional Ectopic Tachycardia (JET) is a type of arrhythmia characterized by an abnormal fast heart rate originating from the junctional area (the region between the atria and ventricles) instead of the normal pacemaker of the heart, the sinoatrial (SA) node.
Characteristics:
Heart Rate: The heart rate typically ranges from 100 to 200 beats per minute but can vary. It is generally consistent and can be seen in paroxysms (episodes of rapid heartbeats).
Origin: JET arises from ectopic (abnormal) pacemaker cells located in the junctional area or the atrioventricular (AV) node.
ECG Findings:
- P waves may be absent, inverted, or occur after the QRS complexes.
- The QRS complexes are typically narrow, reflecting that the ectopic focus is in the junctional area and not below the His-Purkinje system.
17 yo F who initially presented at the age of 4 years with increasing shortness of breath in her home country. There was cyanosis with clubbing and lower oxygen saturations (82%). On echocardiography there was evidence of severe pulmonary hypertension and a large VSD with low velocity bidirectional shunting (enlarged RV, low normal RV function, LV small and compressed by dilated RV). She underwent cardiac catheterisation at the time which showed a pulmonary arterial pressure equal to that of the aorta. Patient admitted with severe respiratory distress, and you are called to intubate.
What are your goals?
What are your goals for induction:
Preload
Contractility
Afterload
Rhythm and Rate
PVR
What are your goals for induction:
Preload: Normal to low in the setting of severe RV dilation
Contractility: Normal to high
Afterload: Normal to mildly high. The higher the afterload, more blood would be shunted to the pulmonary circulation, but there will be more strain to the RV
Rhythm and Rate: Sinus is important, pads, and normal HR for age
PVR: As low as possible, intubation and mechanical ventilation my help or hurt.
This type of VSD is located near the pulmonary valve and aortic valve
What is outlet, doubly committed or juxta-arterial VSD?
The lesions may be associated with aortic insufficiency due to a lack of support for the right coronary cusp of the aortic valve and prolapse of this leaflet.
VSDs are often found alongside these chromosomal syndromes
Trisomy 21, and also trisomy 13 and 18